沙库巴曲缬沙坦治疗AMI后射血分数中间值心力衰竭的疗效研究
张晓旭 杨文奇

摘要:目的 探讨沙库巴曲缬沙坦治疗急性心肌梗死(AMI)后射血分数中间值心力衰竭(HFmrEF)患者的疗效及安全性。方法 将102例AMI后HFmrEF患者依治疗方案的不同分为对照组和试验组,各51例。对照组给予AMI常规治疗及抗心力衰竭(HF)治疗,在无禁忌证前提下使用血管紧张素转化酶抑制剂(ACEI)/血管紧张素Ⅱ受体拮抗剂(ARB);试验组在对照组治疗的基础上将ACEI/ARB替换为沙库巴曲缬沙坦。治疗6个月,统计2组患者治疗后总有效率,比较治疗前后心功能、N末端B型脑钠钛前体(NT-proBNP)及血清C反应蛋白(CRP),记录治疗后不良反应发生情况,Kaplan-Meier法分析2组患者治疗6个月累积心血管死亡率、HF再住院率及无终点事件生存率。结果 治疗6个月,2组患者不良反应发生率差异无统计学意义(P>0.05),试验组总有效率高于对照组(P<0.05)。与治疗前比较,2组患者治疗后左心室射血分数(LVEF)、每搏输出量(SV)、二尖瓣环E峰与A峰比值(E/A)及6 min步行距离(6MWD)均增加,左心室舒张末期内径(LVEDD)及左房内径(LAD)均降低(均P<0.05);治疗后,试验组LVEF、SV、E/A及6MWD高于对照组,LVEDD及LAD低于对照组(均P<0.05)。与治療前比较,2组患者治疗后NT-proBNP和CRP均降低(P<0.05);治疗后,试验组NT-proBNP及CRP低于对照组(P<0.05)。试验组累积心血管死亡率与对照组差异无统计学意义(3.9% vs. 5.9%,P=0.524),试验组累积HF再住院率低于对照组(9.8% vs. 23.5%,P=0.042),累积无终点事件生存率高于对照组(86.3% vs. 70.6%,P=0.037)。结论 沙库巴曲缬沙坦相较于ACEI/ARB治疗AMI后HFmrEF患者更安全有效,值得临床推广。
关键词:心肌梗死;急性病;心力衰竭;药物评价;沙库巴曲缬沙坦;疗效
中图分类号:R541.6文献标志码:ADOI:10.11958/20230587
Clinical study of sacubitril valsartan in the treatment of patients with heart failure of midrange ejection fraction after acute myocardial infarction
Abstract: Objective To investigate the efficacy and safety of sacubitril valsartan in the treatment of heart failure (HF) of midrange ejection fraction(HFmrEF)in patients after acute myocardial infarction (AMI). Methods A total of 102 patients with HFmrEF after AMI were divided into the control group and the experimental group, with 51 cases in each group. The control group was given conventional treatment for AMI and anti-HF treatment, and the angiotensin-converting enzyme inhibitor (ACEI)/ angiotensin Ⅱ receptor blocker (ARB) was used without contraindications. The experimental group was replaced by ACEI/ARB with sacubitril valsartan on the basis of the control group. After 6 months of treatment, the total effective rates of the two groups after treatment were analyzed, and the cardiac function, N-terminal pro-brain natriuretic peptide (NT-proBNP) and serum inflammatory factor C-reactive protein (CRP) were compared before and after treatment. The occurrence of adverse reactions after treatment was recorded. Kaplan-Meier method was used to analyze the cumulative cardiovascular mortality, HF rehospitalization rate and end-event-free survival after 6 months of treatment in two groups. Results After treatment, there was no significant difference in the occurrence of adverse reactions between the two groups (P>0.05). The total effective rate was higher in the experimental group than that of the control group (P<0.05). Compared with before treatment, left ventricular ejection fraction (LVEF), stroke volume (SV), mitral diastolic blood flow velocity E peak and A peak ratio (E/A) and 6 min walking distance (6MWD) were increased in the two groups, and left ventricular end-diastolic diameter (LVEDD) and left atrial diameter (LAD) were decreased in the two groups after treatment (all P<0.05). After treatment, LVEF, SV, E/A and 6MWD were higher in the experimental group than those in the control group (P<0.05). LVEDD and LAD were lower than those in the control group (all P<0.05). Compared with results before treatment, NT-proBNP and CRP were decreased after treatment in the experiment group than those in the control group (P<0.05). There was no significant difference in the cumulative cardiovascular mortality between the experiment group and the control group (3.9% vs. 5.9%,P=0.524). The cumulative HF rehospitalization rate was lower in the experimental group than that of the control group (9.8% vs. 23.5%,P=0.042). The cumulative end-point-free survival rate was higher in the experiment group than that of the control group (86.3% vs. 70.6%, P=0.037). Conclusion Sacubitril valsartan is safer and more effective than ACEI/ARB in the treatment of AMI patients with HFmrEF, and it is worthy of clinical promotion.
Key words: myocardial infarction; acute disease; heart failure; drug evaluation; sacubitril valsartan; curative effect
心力衰竭(HF)是心血管疾病终末期常见结果,潜在的结构性或功能性心脏病是HF的先决条件,其中急性心肌梗死(AMI)是较常见的HF原因之一[1]。HF通常分为射血分数降低型HF(HFrEF)和射血分数保留型HF(HFpEF)。2016年欧洲心脏病学会(ESC)HF诊疗指南[2]引入了第3个类别——射血分数中间值HF(HFmrEF),目前临床上尚无统一的HFmrEF治疗指南或共识。沙库巴曲缬沙坦是全球首个血管紧张素受体脑啡肽酶抑制剂(ARNI)类药物,可改善心肌功能障碍,提高左心室射血分数(LVEF),预防HF并降低AMI所致心血管死亡風险[3-4]。研究认为,沙库巴曲缬沙坦可改善慢性HFrEF患者的预后及生活质量[5-6],提高心功能,安全性较好[7]。本研究旨在探讨沙库巴曲缬沙坦治疗AMI后HFmrEF患者的疗效及安全性。
1 对象与方法
1.1 研究对象 选取2022年1—10月就诊于丹东市第一医院心内科的102例AMI后HFmrEF患者为研究对象。纳入标准:患者符合《2020心肌梗死后心力衰竭防治专家共识》中早发AMI后HF的诊断标准;入组时心脏超声检查确认患者LVEF为0.40~0.49;纽约心脏病协会(NYHA)心功能分级Ⅱ—Ⅳ级。排除标准:对ARNI类药物过敏者;血流动力学不稳定者;未按医嘱服药或未达最大耐受剂量者;病史不清、无法言语、精神异常等影响资料收集和分析者;入院前已患有高钾血症(血钾>5.5 mmol/L)、症状性低血压、血管性水肿或严重肝肾功能不全者;伴有严重创伤、细菌感染、恶性肿瘤及风湿性关节炎等自身免疫性疾病者。本研究通过丹东市第一医院伦理委员会审核批准,患者及家属均签署知情同意书。依治疗方案的不同分为对照组和试验组,各51例,2组患者性别、年龄、体质量指数(BMI)、再灌注策略[经皮冠状动脉介入治疗(PCI)/静脉溶栓]、NYHA心功能分级、既往史差异均无统计学意义(P>0.05),具有可比性,见表1。
1.2 治疗方法 对照组给予AMI常规治疗及利尿、抗血小板聚集、扩血管等常规抗HF治疗,在无禁忌证前提下使用血管紧张素转化酶抑制剂(ACEI)/血管紧张素Ⅱ受体拮抗剂(ARB),并根据患者基础疾病、症状及检查结果合理调整用药方案。试验组在对照组治疗的基础上将治疗中的ACEI/ARB类药物替换为沙库巴曲缬沙坦(北京诺华制药有限公司,国药准字J20190001)进行治疗。具体用药:在使用沙库巴曲缬沙坦治疗前,先停止使用ACEI/ARB类药物36 h,使用时从小剂量开始,25 mg/次,2次/d,在服药过程中动态监测患者血压,每2~4周沙库巴曲缬沙坦剂量加倍,根据患者病情进展及时调整药物剂量,直至最大耐受剂量200 mg/次,2次/d。2组患者均连续治疗6个月。
1.3 观察指标
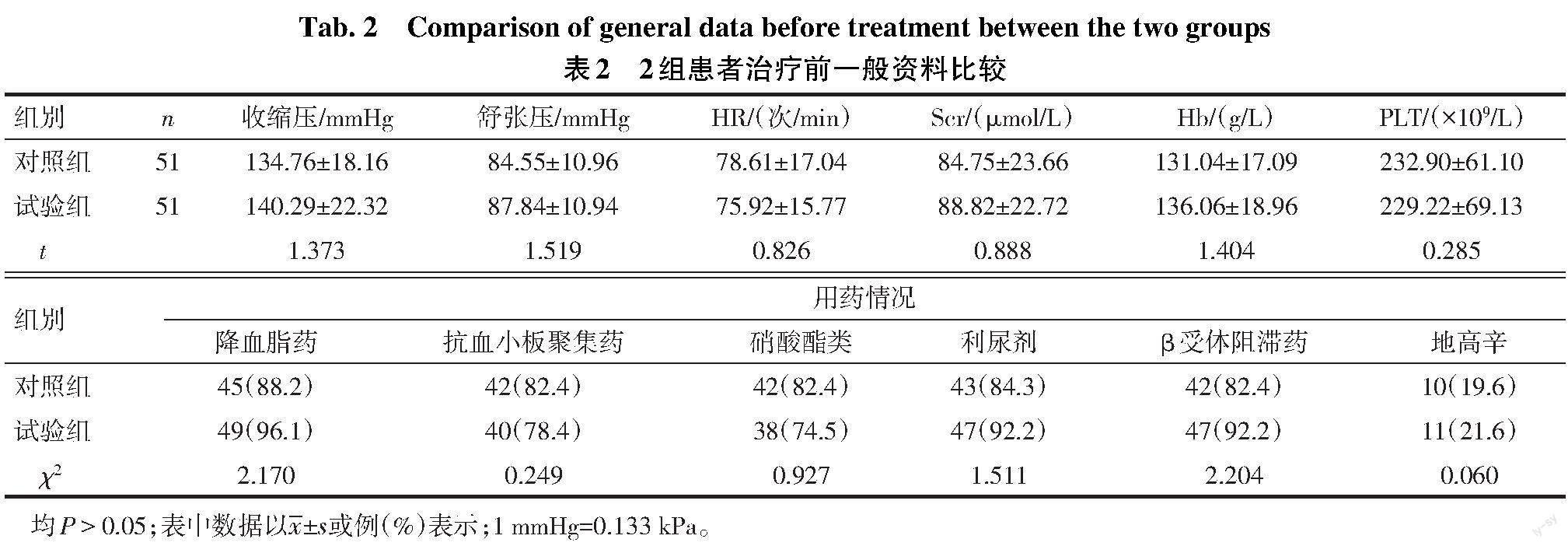
1.3.1 一般资料 治疗前,记录所有患者收缩压、舒张压、心率(HR)、血肌酐(Scr)、血红蛋白(Hb)、血小板(PLT)及用药情况(降血脂药、抗血小板聚集药、硝酸酯类、利尿剂、β受体阻滞药、地高辛)。
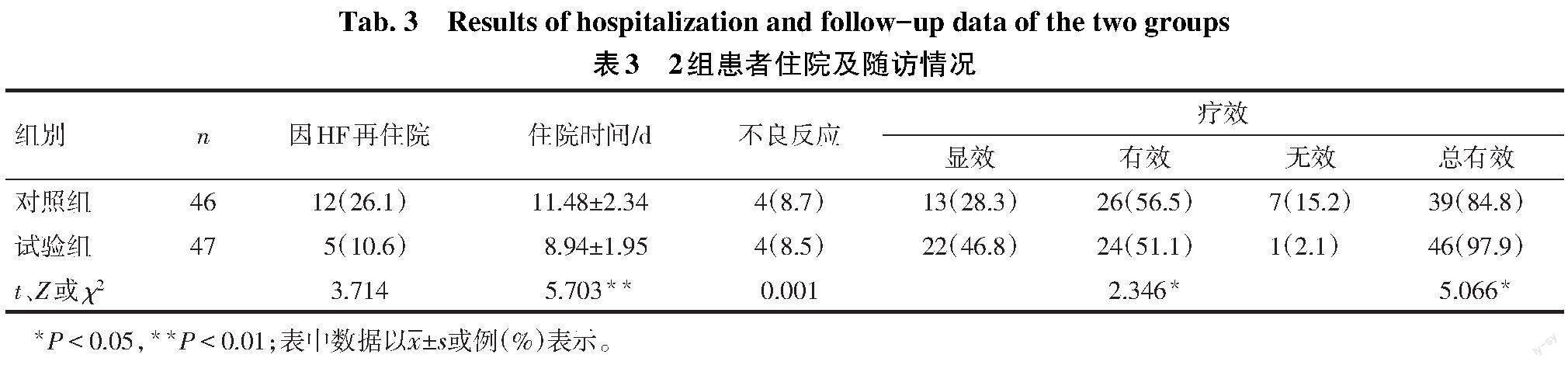
1.3.2 疗效判定标准 依据NYHA心功能分级改善标准统计显效、有效及无效者数。治疗6个月后统计总有效率,失访或因心血管死亡患者不计入疗效判定,总有效率=(显效+有效)/总人数×100%。
1.3.3 心功能、N末端B型脑钠钛前体(NT-proBNP)及血清C反应蛋白(CRP)检测 治疗前及治疗6个月,多普勒超声测定2组患者LVEF、每搏输出量(SV)、左心房内径(LAD)、左心室舒张末期内径(LVEDD)、二尖瓣环E峰与A峰比值(E/A),记录6 min步行距离(6MWD);检测治疗前及治疗6个月NT-proBNP及CRP。失访或因心血管死亡患者不计入观察。
1.3.4 不良反应及终点事件发生情况 所有患者每月门诊随访1次,持续6个月。记录2组患者在治疗6个月内肾功能损害、高钾血症、低血压和血管性水肿等不良反应发生情况,失访或因心血管死亡患者不计入观察。以心血管死亡或HF再住院为终点事件,随访6个月,统计2组患者治疗后累积心血管死亡率、因HF再住院率及无终点事件生存率。
1.4 统计学方法 采用SPSS 25.0软件进行数据分析。采用Graph Pad Prism 8.0作图。正态分布计量资料用[[x] ±s
]表示,2组间比较采用独立样本t检验,组内比较采用配对t检验;非正态分布计量资料以M(P25,P75)表示,组间比较采用Mann-whitney U检验,计数资料以例或例(%)表示,组间比较采用χ2检验或Fisher精确检验。生存分析采用Kaplan-Meier法,组间生存率比较采用Log-rank χ2检验。P<0.05为差异有统计学意义。
2 结果
2.1 2组患者治疗前一般资料比较 2组收缩压、舒张压、HR、Scr、Hb、PLT和用药情况差异均无统计学意义(P>0.05),见表2。
2.2 住院及随访情况 治疗6个月内,对照组和试验组各有2例失访;2组患者共有5例发生心血管死亡,其中试验组2例,对照组3例。对照组4例发生不良反应中低血压2例、肾功能不全2例,试验组4例不良反应中低血压3例、肾功能不全1例,均经调整药物剂量而改善,2组不良反应发生率差异无统计学意义(P>0.05)。治疗6个月后,试验组总有效率高于对照组(P<0.05)。见表3。
2.3 2组患者治疗前后心功能指标比较 组间比较:治疗前,2组心功能各指标差异无统计学意义;治疗后,与对照组比较,试验组LVEF、SV、E/A及6MWD增加,LAD及LVEDD降低(P<0.05)。组内比较:与治疗前比较,治疗后2组LVEF、SV、E/A及6MWD均增加,LVEDD、LAD均降低(P<0.01)。见表4。
2.4 2組患者治疗前后CRP及NT-proBNP比较 治疗前,2组患者CRP及NT-proBNP差异无统计学意义(P>0.05);治疗后,2组患者CRP和NT-proBNP均低于治疗前(P<0.01),且试验组CRP、NT-proBNP较对照组降低(P<0.05),见表5。
2.5 生存分析 治疗6个月,试验组和对照组累积心血管死亡率分别为3.9%和5.9%(Log-rank χ2=0.406,P=0.524),累积HF再住院率分别为9.8%和23.5%(Log-rank χ2=4.120,P=0.042),累积无终点事件生存率分别为86.3%和70.6%(Log-rank χ2=4.360,P=0.037),见图1。
3 讨论
AMI可导致心肌细胞缺血坏死、细胞外基质损伤,最终导致心室重构。目前研究证实,PCI机械血运重建术可以改善冠状动脉病变,降低AMI患者病死率,但治疗后患者仍存在HF的可能[8]。沙库巴曲缬沙坦具有独特的双重抑制作用,即在阻断肾素-血管紧张素-醛固酮系统(RAAS)激活的同时,又能抑制脑啡肽酶活性,是近年来HF治疗的突破性药物[9-10]。NT-proBNP是由前体B型钠尿肽(BNP)分解而成,其稳定性强且半衰期长,是评价心肌损伤的重要指标。在一项涉及LVEF>0.4的HF患者的临床试验中显示,沙库巴曲缬沙坦治疗4周可以明显降低NT-proBNP水平,降低的程度不受试验前治疗药物的影响[11]。本研究结果亦显示,2组患者治疗后NT-proBNP水平较治疗前均明显降低,且试验组下降幅度明显高于对照组。Pieske等[11]研究显示,沙库巴曲缬沙坦并未改善HF患者的6MWD。但本研究结果显示,沙库巴曲缬沙坦较ACEI/ARB更能改善HFmrEF患者6MWD,提高患者的运动耐力。LVEF是反映心脏收缩功能最常用的指标,其大小与HFrEF患者的无终点事件生存率呈正相关[12]。相关研究显示,在AMI后HFrEF和HFpEF患者早期使用沙库巴曲缬沙坦在增加LVEF方面优于ACEI,但并未对HFmrEF患者的临床疗效进行分析[13]。本研究结果显示,2组患者LVEF和SV均高于治疗前,LAD均低于治疗前,且试验组变化幅度明显大于对照组,表明沙库巴曲缬沙坦改善AMI后HFmrEF患者的心室收缩功能的效果优于ACEI/ARB。RAAS的过度激活会导致心肌肥厚、纤维化,甚至坏死,最终导致左心室重构。Frantz等[8]研究认为,左心室重构是HF发生、发展的决定性因素。LVEDD是反映HF患者心室重构的重要指标。本研究结果显示,治疗后2组患者的LVEDD均低于治疗前,且试验组较对照组明显降低,表明沙库巴曲缬沙坦相较于ACEI/ARB更能有效逆转心室重构,改善患者心功能,提高患者的生活质量。Nagueh[14]研究发现,心肌的肥厚和纤维化会导致心脏舒张功能减退,在多数心血管疾病发展过程中,心脏舒张功能障碍常先于收缩功能障碍出现,可用于HF的诊断和预后评估。既往研究显示,E/A的异常(>2或<1)可能是由心脏舒张功能不全引起,而沙库巴曲缬沙坦可以改善E/A,对HFpEF患者疗效显著[15]。本研究结果显示,2组患者治疗后E/A较治疗前明显改善,且试验组较对照组更为显著,表明沙库巴曲缬沙坦可以改善HF患者的心脏舒张功能。AMI后HF会导致心肌损伤、炎症及氧化应激等病理生理改变。Oprescu等[16]研究发现,血清炎性因子CRP与AMI的严重程度呈正相关。本研究结果显示,沙库巴曲缬沙坦可以明显降低AMI后HFmrEF患者的CRP,表明沙库巴曲缬沙坦可以抑制AMI后HF的炎症反应,改善心功能。以心血管死亡或HF再住院为终点事件,试验组累积无终点事件生存率高于对照组,证实了试验组的预后优于对照组。B?hm等[17]研究显示,沙库巴曲缬沙坦比ACEI/ARB降低血压效果更明显,但有导致低血压的风险。本研究结果亦显示,2组患者均出现少数低血压的情况,但均可以通过调整药物用量来改善。
综上所述,沙库巴曲缬沙坦能明显降低AMI后HFmrEF患者的NT-proBNP水平,逆转心室重构,改善心功能,提高患者的运动耐力和生活质量,改善患者临床预后,其效果优于ACEI/ARB,可以作为一个安全有效的治疗选择,值得临床推广。然而,HFmrEF是一种独特的表型,仍需大样本长期临床研究来进一步探索沙库巴曲缬沙坦对其临床疗效及安全性。
参考文献
[1] BAHIT M C,KOCHAR A,GRANGER C B. Post-myocardial infarction heart failure[J]. JACC Heart Fail,2018,6(3):179-186. doi:10.1016/j.jchf.2017.09.015.
[2] PONIKOWSKI P,VOORS A A,ANKER S D,et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology(ESC)Developed with the special contribution of the Heart Failure Association(HFA)of the ESC[J]. Eur Heart J,2016,37(27):2129-2200. doi:10.1093/eurheartj/ehw128.
[3] 张薇琳,周海英,杨小明. 双效血管紧张素受体-脑啡肽酶抑制剂沙库巴曲/缬沙坦的研究进展[J]. 世界临床药物,2017,38(12):851-854. ZHANG W L,ZHOU H Y,YANG X M. Sacubitril/valsartan,a dual angiotensin receptor and neprilysin inhibitior[J]. World Clinical Drug,2017,38(12):851-854. doi:10.13683/j.wph.2017.12.013.
[4] JERING K S,CLAGGETT B,PFEFFER M A,et al. Prospective ARNI vs. ACE inhibitor trial to determine superiority in reducing heart failure events after myocardial infarction (PARADISE-MI):design and baseline characteristics[J]. Eur J Heart Fail,2021,23(6):1040-1048. doi:10.1002/ejhf.2191.
[5] HEIDENREICH P A,BOZKURT B,AGUILAR D,et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure:a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines[J]. Circulation,2022,145(18):e895-e1032. doi:10.1161/CIR.0000000000001063.
[6] ZHANG M,ZOU Y,LI Y,et al. The history and mystery of sacubitril/valsartan:from clinical trial to the real world[J]. Front Cardiovasc Med,2023,10:1102521. doi:10.3389/fcvm.2023.1102521.
[7] QIN J,WANG W,WEI P,et al. Effects of sacubitril-valsartan on heart failure patients with mid-range ejection fractions:a systematic review and meta-analysis[J]. Front Pharmacol,2022,13:982372. doi:10.3389/fphar.2022.982372.
[8] FRANTZ S,HUNDERTMARK M J,SCHULZ-MENGER J,et al. Left ventricular remodelling post-myocardial infarction:pathophysiology,imaging,and novel therapies[J]. Eur Heart J,2022,43(27):2549-2561. doi:10.1093/eurheartj/ehac223.
[9] 張玥,边云飞,郭旭男,等. 沙库巴曲缬沙坦治疗心血管疾病的研究进展[J]. 中国动脉硬化杂志,2022,30(12):1071-1076. ZHANG Y,BIAN Y F,GUO X N,et al. Research progress of sacubitril/valsartan in the treatment of cardiovascular diseases[J]. Chinese Journal of Arteriosclerosis,2022,30(12):1071-1076. doi:10.20039/j.cnki.1007-3949.2022.12.010.
[10] DOCHERTY K F,VADUGANATHAN M,SOLOMON S D,et al. Sacubitril/Valsartan:neprilysin inhibition 5 years after PARADIGM-HF[J]. JACC Heart Fail,2020,8(10):800-810. doi:10.1016/j.jchf.2020.06.020.
[11] PIESKE B,WACHTER R,SHAH S J,et al. Effect of sacubitril/valsartan vs standard medical therapies on plasma NT-proBNP concentration and submaximal exercise capacity in patients with heart failure and preserved ejection fraction:the PARALLAX randomized clinical trial[J]. JAMA,2021,326(19):1919-1929. doi:10.1001/jama.2021.18463.
[12] 王相钰,别柳,王崇全. 沙库巴曲缬沙坦对急性前壁ST段抬高型心肌梗死患者心室重构的研究[J]. 湖北医药学院学报,2023,42(2):153-158. WANG X Y,BIE L,WANG C Q. Effect of sacubitril /valsartan on ventricular remodeling in patients with acute anterior wall ST segment elevation myocardial infarction[J]. Journal of Hubei University of Medicine,2023,42(2):153-158. doi:10.13819/j.issn.2096-708X.2023.02.008.
[13] ZHAO J,ZENG Y,SHEN X. Efficacy and safety of early initiation of Sacubitril/Valsartan in patients after acute myocardial infarction:a meta-analysis[J]. Clin Cardiol,2021,44(10):1354-1359. doi:10.1002/clc.23717.
[14] NAGUEH S F. Left ventricular diastolic function:understanding pathophysiology,diagnosis,and prognosis with echocardiography[J]. JACC Cardiovasc Imaging,2020,13(1/2):228-244. doi:10.1016/j.jcmg.2018.10.038.
[15] 賈红丹,丛洪良,赵云凤,等. 沙库巴曲缬沙坦治疗慢性心力衰竭患者的疗效观察[J]. 天津医药,2019,47(10):1076-1080. JIA H D,CONG H L,ZHAO Y F,et al. The efficiency of sacubitril/valsartan therapy in patients with chronic heart failure[J]. Tianjin Med J,2019,47(10):1076-1080. doi:10.11958/20191271.
[16] OPRESCU N,MICHEU M M,SCAFA-UDRISTE A,et al. Inflammatory markers in acute myocardial infarction and the correlation with the severity of coronary heart disease[J]. Ann Med,2021,53(1):1041-1047. doi:10.1080/07853890.2021.1916070.
[17] B?HM M,YOUNG R,JHUND P S,et al. Systolic blood pressure,cardiovascular outcomes and efficacy and safety of sacubitril/valsartan(LCZ696)in patients with chronic heart failure and reduced ejection fraction:results from PARADIGM-HF[J]. Eur Heart J,2017,38(15):1132-1143. doi:10.1093/eurheartj/ehw570.