母血及羊水中TIM-3、GATA-3水平对胎膜早破合并宫内感染的诊断价值
王思思 谢双双 孟玥秀 张翔云 刘云春
摘要:目的 分析母血及羊水中T细胞免疫球蛋白黏蛋白分子-3(TIM-3)、GATA结合蛋白3(GATA-3)水平对胎膜早破(PROM)合并宫内感染的诊断价值。方法 选择PROM患者89例作为研究对象,发生宫内感染者42例作为感染组,未发生宫内感染者47例作为未感染组,并选择同期正常足月孕妇45例作为对照组。根据宫内感染严重程度将PROM合并宫内感染患者分成轻度组16例、中度组17例、重度组9例。检测血、羊水中TIM-3、GATA-3 mRNA及蛋白水平,比较对照组、未感染组、感染组和不同感染程度孕妇血、羊水中TIM-3、GATA-3 mRNA及蛋白水平,受试者工作特征曲线分析血清及羊水中TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的效能。结果 对照组、未感染组、感染组血及羊水中TIM-3 mRNA、蛋白水平依次升高(P<0.05),GATA-3 mRNA、蛋白水平依次降低(P<0.05);輕度组、中度组、重度组血及羊水中TIM-3 mRNA、蛋白水平依次升高(P<0.05),GATA-3 mRNA、蛋白水平依次降低(P<0.05);血清TIM-3、GATA-3蛋白单独及联合,羊水TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的曲线下面积分别为0.854、0.813、0.937,0.834、0.850、0.922。结论 PROM合并宫内感染患者母血及羊水中TIM-3呈高表达,GATA-3呈低表达,两者均对PROM孕妇发生宫内感染有一定的诊断价值,联合诊断效能更高。
关键词:胎膜早破;羊水;甲型肝炎病毒细胞受体2;母血;T细胞免疫球蛋白黏蛋白分子-3;GATA结合蛋白3;宫内感染
中图分类号:R714 文献标志码:A DOI:10.11958/20221201
The diagnostic value of TIM-3 and GATA-3 levels in maternal blood and amniotic fluid for premature rupture of membranes complicated with intrauterine infection
WANG Sisi, XIE Shuangshuang, MENG Yuexiu, ZHANG Xiangyun, LIU Yunchun
Department of Obstetrics and Gynecology, the First Hospital Affiliated to Hebei North University, Zhangjiakou 075000, China
Abstract: Objective To analyze the diagnostic value of T cell immunoglobulin mucin molecule-3 (TIM-3) and GATA binding protein-3 (GATA-3) in maternal blood and amniotic fluid in the diagnosis of premature rupture of membranes (PROM) complicated with intrauterine infection. Methods Eighty-nine patients with PROM were regarded as the research subjects. Among them, 42 patients with intrauterine infection were regarded as the infection group, and 47 patients without intrauterine infection were regarded as the uninfected group. Meantime, 45 normal full-term pregnant women were used as the control group. According to the severity of intrauterine infection, PROM complicated with intrauterine infection patients were divided into the mild group (16 cases), the moderate group (17 cases) and the severe group (9 cases). The mRNA and protein levels of TIM-3, GATA-3 in whole blood and amniotic fluid were detected. The mRNA and protein levels of TIM-3, GATA-3 in whole blood and amniotic fluid were compared between the control group, the uninfected group, the infection group and pregnant women with different degrees of infection. The efficacy of TIM-3 and GATA-3 proteins in serum and amniotic fluid alone and in combination in the diagnosis of intrauterine infection in pregnant women with PROM were analyzed by receiver operating characteristic curve. Results The TIM-3 mRNA and protein levels in whole blood and amniotic fluid of the control group, the uninfected group and the infection group were increased in turn (P<0.05), and GATA-3 mRNA and protein levels decreased in turn (P<0.05). The TIM-3 mRNA and protein levels in whole blood and amniotic fluid of the mild group, the moderate group and the severe group increased in turn (P<0.05), and GATA-3 mRNA and protein levels decreased in turn (P<0.05). The area under curve of serum TIM-3 and GATA-3 protein alone and in combination, and amniotic fluid TIM-3 and GATA-3 protein alone and in combination to diagnose intrauterine infection in pregnant women with PROM were 0.854, 0.813, 0.937, 0.834, 0.850 and 0.922, respectively. Conclusion The maternal blood and amniotic fluid of patients with PROM complicated with intrauterine infection have high expression of TIM-3 and low expression of GATA-3, both of them have certain diagnostic value for intrauterine infection in pregnant women with PROM, and the combined diagnostic efficiency is higher.
Key words: fetal membranes, premature rupture; amniotic fluid; hepatitis A virus cellular receptor 2; maternal blood; T cell immunoglobulin mucin molecule-3; GATA binding protein-3; intrauterine infection
胎膜早破(premature rupture of membranes,PROM)是指在分娩开始前发生胎膜破裂,是常见的产科并发症,PROM在所有妊娠中的發生率为5%~10%,其中足月产妇PROM发生率为2.0%~3.5%,未足月产妇PROM发生率为6%~10%[1]。PROM可诱导早产、脐带异常、胎盘早剥、胎儿畸形、宫内感染、绒毛膜羊膜炎等的发生,严重影响孕产妇及胎儿的生命健康[2]。PROM的发生与炎症有关,炎性细胞因子浸润可导致慢性非特异性炎症,与PROM宫内感染的发生发展密切相关[3]。孕妇发生PROM后,宫内感染的概率增高,可导致新生儿多脏器损伤、败血症等,甚至死亡[4]。PROM与感染互为因果,大多数亚临床期的宫内感染症状不明显,早期诊断困难[5]。因此,急需寻找可识别早期PROM宫内感染的生物学指标物。T细胞免疫球蛋白黏蛋白分子-3(T cell immunoglobulin mucin molecule-3,TIM-3)在T细胞激活、分化、抗原提呈等过程中发挥调控作用,可介导相关细胞因子表达,抑制免疫应答[6]。GATA结合蛋白3(GATA binding protein-3,GATA-3)是辅助性T细胞(Th)1/Th2分化过程中的重要转录因子,可正调控Th2细胞发育,从而影响炎症反应[7]。目前,关于TIM-3、GATA-3与PROM孕妇发生宫内感染关系的研究较少。本研究拟通过检测母血及羊水中TIM-3、GATA-3水平变化,分析两者对PROM孕妇发生宫内感染的诊断效能,从而为PROM宫内感染早期诊断提供新的思路。
1 资料与方法
1.1 一般资料 选择2021年5月—2022年4月河北北方学院附属第一医院收治的PROM患者89例作为研究对象,其中发生宫内感染者42例作为感染组,年龄21~36岁,平均(27.90±5.26)岁,孕周36~41周,平均(38.14±3.73)周;未发生宫内感染者47例作为未感染组,年龄21~35岁,平均(28.45±5.37)岁,孕周36~41周,平均(38.34±3.97)周。纳入标准:(1)符合《妇产科学(第8版)》中PROM诊断标准[8]。(2)单胎初产妇,破膜后12 h内入院。(3)头位妊娠。排除标准:(1)合并子痫前期、妊娠期糖尿病等妊娠期合并症者。(2)合并心、肝、肾、肺等功能不全者。(3)凝血功能障碍者。(4)出现羊水污染、子宫压痛、宫缩、阴道分泌脓性物等症状。选择同期正常足月孕妇45例作为对照组,年龄22~37岁,平均(29.13±5.61)岁,孕周37~42周,平均(38.53±4.15)周。3组年龄、孕周比较差异无统计学意义(F分别为0.564和0.105,均P>0.05)。所有研究对象均签署知情同意书,并经医院伦理委员会核准(批准号:2021-01-04)。
1.2 研究方法
1.2.1 宫内感染严重程度评价 甲醛固定剖宫产术中所得胎膜,经组织学检查,制片,镜下观察中性粒细胞浸润程度,发生宫内感染标准为中性粒细胞数>5个/视野。其中5个<中性粒细胞数≤10个为轻度感染(轻度组),11个≤中性粒细胞数≤30个为中度感染(中度组),中性粒细胞数>30个为重度感染(重度组)[9]。轻、中、重度组分别为16、17、9例。
1.2.2 样本采集 于分娩前抽取孕妇的空腹肘静脉血6 mL,其中3 mL进行乙二胺四乙酸抗凝,3 000 r/min离心15 min,取上层血浆,提取总RNA,行荧光定量PCR(qRT-PCR)检测;另3 mL不进行抗凝处理,3 000 r/min离心15 min,取上层血清,-70 ℃冻存,用于酶联免疫吸附试验(ELISA)检测。于分娩时常规消毒外阴,上推胎头使羊水流出,用无菌注射器抽取羊水5 mL,3 000 r/min离心20 min,收集上清液,-20 ℃保存。
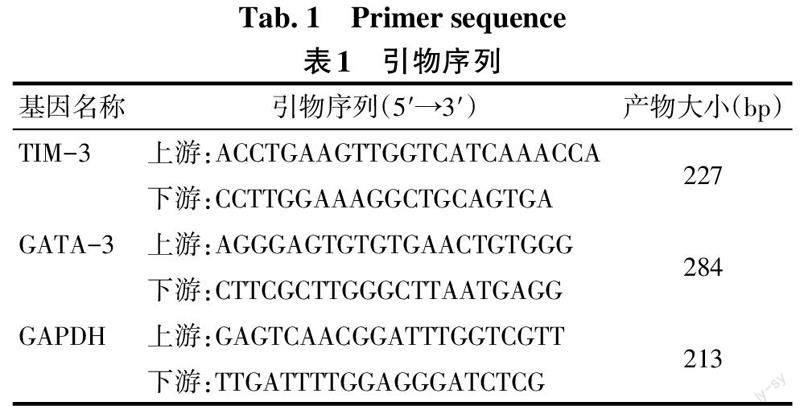
1.2.3 荧光定量PCR(qRT-PCR)法检测血浆及羊水中TIM-3、GATA-3 mRNA水平 TRIzol试剂(加拿大Fermentas公司,批号CR1437K)提取3组孕妇血浆及羊水总RNA,逆转录试剂盒(加拿大Fermentas公司,批号CR1760K)将RNA逆转录为cDNA。配制qRT-PCR(PCR试剂盒购自北京百奥莱博科技有限公司,批号YT381)反应体系(20 μL):cDNA 2 μL,上下游引物各0.5 μL,2×SYBR Green PCR Master Mix 10 μL,ddH2O 7 μL。PCR循环参数:95 ℃ 10 min;94 ℃ 5 s,58 ℃ 30 s,72 ℃ 20 s,40个循环。以2-ΔΔCt法计算TIM-3、GATA-3 mRNA的相对表达量。TIM-3、GATA-3及内参GAPDH引物由上海斯信生物科技有限公司设计合成,引物序列见表1。
1.2.4 ELISA法检测血清及羊水中TIM-3、GATA-3蛋白水平 采用ELISA法检测血清及羊水中TIM-3、GATA-3蛋白水平,分别按照人TIM-3 ELISA试剂盒(德国MERCK公司,批号RAB1087)、人GATA3 ELISA试剂盒(英国Abcam公司,批号ab230939)说明书进行操作。
1.3 统计学方法 应用SPSS 24.0软件进行数据分析,计量资料以均数±标准差(x±s)表示,多组间比较采用单因素方差分析,多重比较采用LSD-t检验;受试者工作特征(ROC)曲线分析血清及羊水中TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的效能。P<0.05为差异有统计学意义。
2 结果
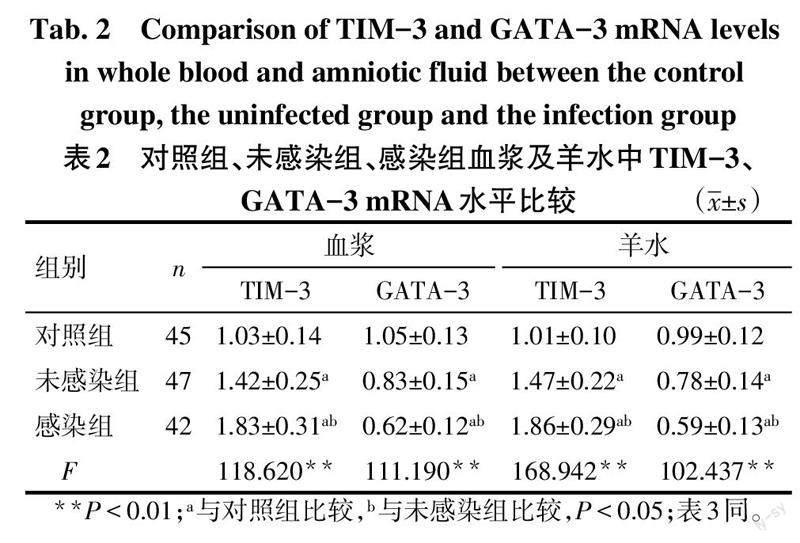
2.1 对照组、未感染组、感染组血浆及羊水中TIM-3、GATA-3 mRNA水平比较 对照组、未感染组、感染组血浆及羊水中TIM-3 mRNA水平依次升高,GATA-3 mRNA水平依次降低(P<0.05),见表2。
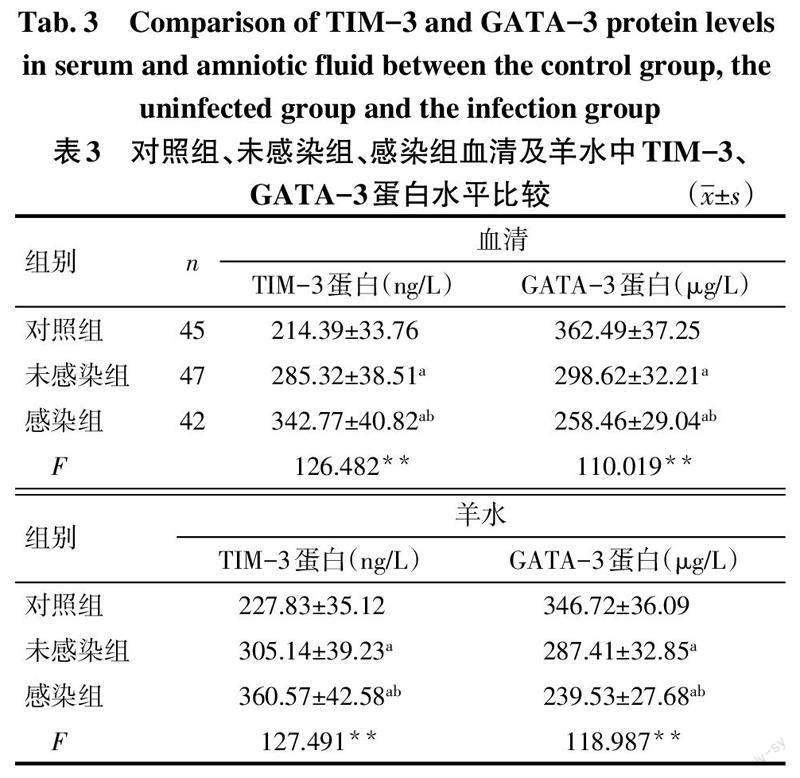
2.2 对照组、未感染组、感染组血清及羊水中TIM-3、GATA-3蛋白水平比较 对照组、未感染组、感染组血清及羊水中TIM-3蛋白水平依次升高,GATA-3蛋白水平依次降低(P<0.05),见表3。
2.3 不同感染程度孕妇血浆及羊水中TIM-3、GATA-3 mRNA水平比较 轻度组、中度组、重度组血浆及羊水中TIM-3 mRNA水平依次升高,GATA-3 mRNA水平依次降低(P<0.05),见表4。
2.4 不同感染程度孕妇血清及羊水中TIM-3、GATA-3蛋白水平比较 轻度组、中度组、重度组血清及羊水中TIM-3蛋白水平依次升高,GATA-3蛋白水平依次降低(P<0.05),见表5。
2.5 血清及羊水中TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的效能 ROC曲线显示,血清TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的曲线下面积(AUC)分别为0.854、0.813、0.937;羊水TIM-3、GATA-3蛋白单独及联合诊断PROM孕妇发生宫内感染的AUC分别为0.834、0.850、0.922,见图1、2,表6。
3 讨论
PROM是妊娠晚期常见并发症,其主要发病原因为胎膜发育不良、宫腔内压力异常、宫颈内口松弛、感染、创伤等导致母體胎膜结构被破坏,胎膜较为薄弱处可能会随着孕周的增长而发生破裂[10]。研究发现,PROM可减弱羊水的抑菌作用,增加感染风险,一旦PROM合并宫内感染,胎儿窘迫、早产、败血症、肺炎以及死亡等不良妊娠结局的发生风险增加[11]。但PROM合并宫内感染者几乎无典型临床症状,难以判断是否发生宫内感染,而产妇一旦出现羊水污染、白细胞异常、子宫压痛、宫缩、阴道分泌脓性物等症状,则需终止妊娠[12]。现阶段,细菌培养、胎盘病理为诊断宫内感染的“金标准”,但2种诊断方法较为滞后,往往在产后数日方可得到准确结果,难以满足临床诊断需求[13]。因而,需要寻找可靠的宫内感染早期诊断指标。
TIM-3是一种Ⅰ型膜蛋白,是Th1相关的负性共刺激因子,在T细胞分化、增殖、凋亡过程中发挥调控作用,参与T细胞免疫应答,且与多种自身免疫疾病、病毒感染等密切相关[14]。TIM-3可通过结合配体,在Th17、Treg细胞上表达,进而抑制Th17和Treg细胞分化、促进细胞凋亡,引起免疫应答下调[15]。李雪莲等[16]研究发现,TIM-3在早期自然流产患者外周血及子宫蜕膜中高表达,其可能通过破坏Th17/Treg平衡,抑制CD4+ T细胞增殖,导致母胎界面免疫调控失衡,造成胚胎发育停止。TIM-3信号通路在正常妊娠过程中可介导母胎界面Th1/Th2的平衡,在适应性免疫应答及固有免疫过程中发挥关键作用,维持母胎免疫耐受[17]。本研究中,感染组、未感染组母血、羊水TIM-3 mRNA及蛋白水平均高于对照组,感染组母血、羊水TIM-3 mRNA及蛋白水平均高于未感染组,且随着PROM合并宫内感染严重程度加重,TIM-3 mRNA及蛋白水平不断增加,提示TIM-3在PROM合并宫内感染患者中异常表达,且与感染程度有关,推测TIM-3可能通过调控炎性因子浸润,影响母体免疫应答,从而参与宫内感染。进一步分析显示,血清、羊水TIM-3蛋白水平诊断PROM发生宫内感染的AUC为0.854、0.834,均有一定的诊断价值,可作为诊断PROM发生宫内感染的潜在指标。
GATA-3可在胎盘发育过程中发挥调控作用,在所有类型的滋养细胞中均有表达,是一种较为敏感的滋养细胞免疫标志物,但无法准确鉴别滋养细胞肿瘤及其分型[18]。同时,GATA-3是Th2细胞的特异转录因子,T细胞转录因子(T-bet)/GATA-3比值可更为准确客观地反映Th1/Th2细胞的分化[19]。孕产妇若出现明显的Th1/Th2失衡,母胎免疫耐受遭到破坏,母体免疫排斥胎儿,从而引发一系列疾病[20]。本研究中,感染组、未感染组母血、羊水GATA-3 mRNA及蛋白水平均低于对照组,感染组母血、羊水GATA-3 mRNA及蛋白水平均低于未感染组,且PROM合并宫内感染越严重,GATA-3 mRNA及蛋白水平越低,表明GATA-3在PROM合并宫内感染中呈低表达,且与患者感染程度有关,推测GATA-3异常表达可破坏Th1/Th2平衡,从而参与宫内感染的发生发展。进一步分析显示,血清和羊水中GATA-3蛋白水平诊断PROM发生宫内感染的AUC为0.813、0.850,均可作为诊断PROM发生宫内感染的指标。但血清及羊水TIM-3、GATA-3单独诊断PROM发生宫内感染的敏感度、特异度尚不够理想,因此联合TIM-3、GATA-3进行诊断,结果发现,血清TIM-3蛋白联合GATA-3蛋白、羊水TIM-3蛋白联合GATA-3蛋白诊断PROM孕妇发生宫内感染的AUC分别为0.937、0.922,诊断效能均高于单独诊断,此外,血清相比于羊水更容易获得,临床应用更为方便、快捷,因此更加倾向于使用血清进行诊断。
综上所述,PROM合并宫内感染患者母血及羊水中TIM-3呈高表达,GATA-3呈低表达,两者均对PROM孕妇发生宫内感染有一定的诊断价值,联合诊断效能更高,但是否能够在临床中大范围应用,还需扩大样本量进一步探究。
参考文献
[1] DARLING A J,HARRIS H M,ZEMTSOV G E,et al. Risk factors for adverse maternal outcomes following expectantly managed preterm prelabor rupture of membranes[J]. Am J Perinatol,2022,39(8):803-807. doi:10.1055/s-0041-1740011.
[2] ZHU J,MA C,ZHU L,et al. A role for the NLRC4 inflammasome in premature rupture of membrane[J]. PLoS One,2020,15(8):e0237847. doi:10.1371/journal.pone.0237847.
[3] FAROOQUI R,SIDDIQUI Q U. Diagnostic accuracy of procalcitonin in maternal plasma to detect early intra-amniotic infection in preterm premature rupture of the membranes with respect of highvaginal swab as gold standard[J]. Pak J Med Sci,2022,38(1):310-314. doi:10.12669/pjms.38.1.4436.
[4] BEN M'BAREK I,LANDRAUD L,DESFRERE L,et al. Contribution of vaginal culture to predict early onset neonatal infection in preterm prelabor rupture of membranes[J]. Eur J Obstet Gynecol Reprod Biol,2021,261:78-84. doi:10.1016/j.ejogrb.2021.04.016.
[5] 狄紅丽,郝树磊,杨彩凤,等. β-HCG、CRP和TNF-α联合检测在胎膜早破宫内感染中的预测作用[J]. 分子诊断与治疗杂志,2022,14(3):483-486. DI H L,HAO S L,YANG C F,et al. Predictive role of combined detection of β-HCG,CRP and TNF-α in intrauterine infection in premature rupture of membranes[J]. Journal of Molecular Diagnostics and Therapy,2022,14(3):483-486. doi:10.3969/j.issn.1674-6929.2022.03.031.
[6] YANG R,SUN L,LI C F,et al. Galectin-9 interacts with PD-1 and TIM-3 to regulate T cell death and is a target for cancer immunotherapy[J]. Nat Commun,2021,12(1):832. doi:10.1038/s41467-021-21099-2.
[7] 陈国华,黄为民,潘志伟,等. 反复喘息婴幼儿外周血单核细胞中T-bet/GATA-3比值与潮气呼吸肺功能及Th1/Th2细胞平衡的关系[J]. 中国医药导报,2021,18(3):26-29,34. CHEN G H,HUANG W M,PAN Z W,et al. Relationship between T-bet/GATA-3 ratio in peripheral blood mononu-clear cells and tidal breathes lung function and Th1/Th2 cell balance in recurrent wheezing infants[J]. Chin Med Herald,2021,18(3):26-29,34.
[8] 谢幸,苟文丽. 妇产科学[M]. 8版. 北京:人民卫生出版社,2013:138-139. XIE X,GOU W L. Obstetrics and gynecology[M]. 8th ed. Beijing:People's Health Publishing House,2013:138-139.
[9] 孙晓霞,张兆波,张玉枝,等. 血清β-HCG,hsCRP及CRP检测对胎膜早破宫内感染的诊断价值[J]. 现代生物医学进展,2016,16(22):4363-4366. SUN X X,ZHANG Z B,ZHANG Y Z,et al. Predictive value of serum β-HCG,hsCRP and CRP levels on intrauterine infection of pregnant women with premature rupture of membranes[J]. Progress in Modern Biomedicine,2016,16(22):4363-4366. doi:10.13241/j.cnki.pmb.2016.22.043.
[10] LI L,YAN Y,QI H,et al. A risk score for the early prediction of postpartum bloodstream infections in patients with premature rupture of membranes:A pilot study[J]. Int J Gynaecol Obstet,2020,150(3):419-420. doi:10.1002/ijgo.13169.
[11] OH K J,ROMERO R,PARK J Y,et al. The earlier the gestational age,the greater the intensity of the intra-amniotic inflammatory response in women with preterm premature rupture of membranes and amniotic fluid infection by Ureaplasma species[J]. J Perinat Med,2019,47(5):516-527. doi:10.1515/jpm-2019-0003.
[12] BONASONI M P,PALICELLI A,DALLA DEA G,et al. Klebsiella pneumoniae chorioamnionitis:An underrecognized cause of preterm premature rupture of membranes in the second trimester[J]. Microorganisms,2021,9(1):96. doi:10.3390/microorganisms9010096.
[13] RONZONI S,STECKLE V,D'SOUZA R,et al. Cytokine changes in maternal peripheral blood correlate with time-to-delivery in pregnancies complicated by premature prelabor rupture of the membranes[J]. Reprod Sci,2019,26(9):1266-1276. doi:10.1177/1933719118815590.
[14] ZILBER E,MARTIN G E,WILLBERG C B,et al. Soluble plasma programmed death 1 (PD-1) and Tim-3 in primary HIV infection[J]. AIDS,2019,33(7):1253-1256. doi:10.1097/QAD.0000000 000002165.
[15] 刘叶,王缚鲲,汤菲. TIM-3抑制对支气管哮喘患者免疫平衡功能的影响[J]. 解放军医药杂志,2019,31(10):43-46. LIU Y,WANG F K,TANG F. Effect of TIM-3 inhibition on immune balance function in patients with bronchial asthma[J]. Medical & Pharmaceutical Journal of Chinese People's Liberation Army,2019,31(10):43-46. doi:10.3969/j.issn.2095-140X.2019.10.010.
[16] 李雪莲,丁华,姜忠训,等. Tim-3在早期自然流产中的作用及与Th17/Treg细胞的关系[J]. 广州医科大学学报,2019,47(1):6-9. LI X L,DING H,JIANG Z X,et al. The role of Tim-3 in early spontaneous abortion and its relationship with Th17/Treg cells[J]. Academic Journal of Guangzhou Medical University,2019,47(1):6-9. doi:10.3969/j.issn.2095-9664.2019.01.02.
[17] 卿吉琳,陈治中,谭卫红. TIM-3-Gal-9信号途径在原因不明复发性流产中的研究进展[J]. 中国免疫学杂志,2018,34(11):1743-1747. QING J L,CHEN Z Z,TAN W H. Research progress of TIM-3-Gal-9 pathway in unexplained recurrent spontaneous abortion[J]. Chinese Journal of Immunology,2018,34(11):1743-1747. doi:10.3969/j.issn.1000-484X.2018.11.031.
[18] XIAO L,MA L,WANG Z,et al. Deciphering a distinct regulatory network of TEAD4, CDX2 and GATA3 in humans for trophoblast transition from embryonic stem cells[J]. Biochim Biophys Acta Mol Cell Res,2020,1867(9):118736. doi:10.1016/j.bbamcr.2020.118736.
[19] HERTWECK A,VILA DE MUCHA M,BARBER P R,et al. The TH1 cell lineage-determining transcription factor T-bet suppresses TH2 gene expression by redistributing GATA3 away from TH2 genes[J]. Nucleic Acids Res,2022,50(8):4557-4573. doi:10.1093/nar/gkac258.
[20] 褚娜利,聂风华,刘玉欣,等. Torch感染与自然流产及Th1/Th2细胞因子水平相关分析[J]. 中国实验诊断学,2021,25(9):1368-1369. CHU N L,NIE F H,LIU Y X,et al. Correlation analysis of Torch infection with spontaneous abortion and Th1/Th2 cytokine level[J]. Chinese Journal of Laboratory Diagnosis,2021,25(9):1368-1369. doi:10.3969/j.issn.1007-4287.2021.09.034.
(2022-08-01收稿 2022-10-11修回)
(本文編辑 李国琪)