Efficacy, effectiveness, and safety of combination laser and tranexamic acid treatment for melasma: A meta-analysis
Arik Ltshi Adeli, Sri Adil Nuriniwti, Probo Yudh Prtm Putr,Auli Sit Hpsri
a Medical Faculty, University of Brawijaya, Malang 65145, East Java, Indonesia
b Department of Dermatology and Venereology, Medical Faculty, University of Muhammadiyah Malang, Malang 65144, East Java, Indonesia
c Medical Faculty, University of Muhammadiyah Malang, Malang 65144, East Java, Indonesia
Keywords:Laser Melasma Tranexamic acid
A B S T R A C T
1.Introduction
Melasma is the most common cause of facial melanosis and is characterized by hyperpigmented macules developing on the face.These macules become more pronounced after exposure to sunlight.1,2Melasma commonly presents as irregularly shaped macules and patches symmetrically located on the face.While it can occasionally affect the neck and forearms, it predominantly affects the face.3,4This condition is more prevalent in women and in individuals with darker skin tones,especially in those with Fitzpatrick skin types IV–VI.4
Various studies have estimated that the overall prevalence of melasma in the general population ranges from 1% to 50%.Additionally, a positive family history has been reported in 55%–64% of cases.5Although the exact cause of melasma remains unknown,several common risk factors have been identified, including genetics, exposure to ultraviolet light, pregnancy, and oral contraceptives or medications such as phenytoin.4,5
Melasma substantially affects the quality of life of patients, causing cosmetic concerns and psychological distress.Treatment of melasma is challenging because of its unclear etiology, persistent nature, and tendency to relapse.6,7First-line treatments include photoprotection and the use of topical lightening products.Second-line treatments include lasers,mechanical and chemical peels, and oral tranexamic acid (TXA).These treatments have been associated with substantial side effects, such as post-inflammatory dyspigmentation, scarring, and venous thromboembolism.8Topical treatments have traditionally been the primary approach for treating melasma.9However, the use of hydroquinone, a commonly used topical agent,is limited because of complications such as irritant dermatitis, allergic contact dermatitis, and post-inflammatory hyperpigmentation.10The safety concerns associated with hydroquinone have prompted a search for alternative therapies that are both effective and safe.11
2.Methods
2.1.Literature search
This meta-analysis adhered to the PRISMA guidelines, as shown in Fig.1.12A literature search was conducted across multiple databases,including Cochrane, ScienceDirect, PubMed, and Google Scholar.The keywords used in this search were “tranexamic acid,” “laser,” and“melasma.” This study focused on randomized controlled trials (RCTs)conducted between 2012 and 2021.
2.2.Inclusion and exclusion criteria
The inclusion criteria of the study were (1) RCTs, (2) use of a combination therapy involving laser and TXA, and (3) reporting of at least one of the following outcomes: the Melasma Area and Severity Index(MASI)score and treatment side effects.The exclusion criterion was nonextractable data.
2.3.Outcomes assessed
This study examined and evaluated the following outcomes:the MASI score and side effects.
2.4.Assessment of study quality
The RCT quality was evaluated using the Jadad score, which ranges from 0 to 5.13Scores of >4, 3–4, and <3 indicated high-, medium-, and low-quality studies,respectively.The level of evidence for each study was assessed according to the criteria of the Oxford Center for Evidence-Based Medicine.14
2.5.Statistical analysis
Review Manager version 5.3 was utilized for statistical analysis.The total odds ratio (OR) for each parameter was evaluated and the corresponding 95% confidence interval (CI) and mean difference (MD) were calculated.The Cochrane chi-square test and inconsistency(I2)were used to assess study heterogeneity.Statistical significance was set at a P=0.05,and heterogeneity was deemed considerable when I2was>50%.

Fig.1.PRISMA flow diagram for study selection.
3.Results
3.1.Baseline characteristics
The search parameters identified 1 504 relevant studies from four sources; all the studies were reviewed, and three were selected for analysis.15–17The studies included 140 participants each, with 69 participants in the combination group who received laser and TXA and 71 participants in the control group who received monotherapy.Table 1 provides an overview of the characteristics of each study.The evidence level of these studies was categorized as 1b according to the RCT classification,and the Jadad score was within the range of 3–4.
3.2.MASI score
From the three studies analyzed,data from 140 patients(69 patients in the combination therapy group and 71 patients in the control (monotherapy) group) were included.The findings showed no significant difference in the overall MASI score between the two groups(MD,1.87;95% CI, -0.78–4.52; P=1.39) with high reported heterogeneity(I2=80%) (Fig.2).For the MASI score at 0 weeks (MD, -0.87; 95% CI,-2.49–0.74; P=1.06), there was less heterogeneity (I2=0%).For the MASI score at 4 weeks (MD, 0.15; 95% CI, -2.34–2.64; P=0.12) and 8 weeks(MD,6.78;95%CI,-8.01–21.56;P=0.90),there was substantial heterogeneity(I2=80%and 79%,respectively).Meanwhile,for the MASI score at 12 weeks(MD,10.09;95%CI,-8.84–29.03;P=1.04),there was significant heterogeneity(I2=95%).
3.3.Side effects
There was no significant difference observed in erythema between the two groups (OR=5.38; 95% CI, 0.25–117.25; P=0.28) with less heterogeneity(I2=0%)(Fig.3).Itching was less prevalent in the control group (OR=10.81; 95% CI, 1.31–89.09; P=0.03) with no heterogeneity(I2=0%).However, the overall incidence of side effects in the pooled subgroup was higher in the laser combined with TXA group (OR=8.85;95%CI,1.57–50.01;P=0.01)with no heterogeneity(I2=0%).
4.Discussion
Melasma is a skin condition that predominantly affects areas exposed to sunlight, particularly in women of reproductive age.It significantly impacts the quality of life, leading to low self-esteem,social challenges,and symptoms of anxiety and depression.18,19Treatment of melasma is challenging owing to its unclear pathogenesis and tendency to relapse.Existing treatment options do not provide complete or long-lasting improvement.20The present study found no significant difference in the MASI scores between the combination therapy(laser and TXA)group and monotherapy group.Thus, laser treatment is effective and safe for treating melasma.However, further investigations are needed to evaluate the potential benefits of adding TXA to the treatment regimen.17
No significant difference in the overall incidence of side effects,such as erythema and itching, was observed between the two groups.Laser treatment is a common physical method to treat melasma.21Various types of laser treatments have been used to treat melasma, yielding diverse outcomes.22The most commonly used laser treatment for melasma is the Q-switched Nd:YAG laser, which works by deeply penetrating the skin to target dermal melanin.It utilizes photo-acoustic mechanisms to destroy melanosomes and blood vessels while minimizing damage to keratinocytes and melanocytes, leading to minimal epidermal damage.23,24The Q-switching technique delivers high-energy pulses in a short duration (nanoseconds).25Lower-energy settings are preferred to mitigate the risk of post-inflammatory hyperpigmentation and exacerbation of melasma.26
Immediate complications, including pain, erythema, edema, and blistering, are directly associated with the energy utilized during the procedure.27However,most of these side effects are mild and temporary,typically resolving within 4 days.28While post-laser erythema is expected,prolonged erythema is a frequent and unwanted complication.29The exact mechanism underlying the development of erythema remains unclear.This may involve factors such as increased blood flow as part of the inflammatory response, epidermal immaturity, reduced light absorption by melanin,and altered light dispersion in the dermis.Itching is a secondary response to the physiological healing process.30
In addition to its hemostatic effects,TXA possesses anti-inflammatory and anti-allergic properties.TXA is a synthetic derivative of the amino acid lysine that binds to lysine residues in plasminogen and prevents its conversion to plasmin.This inhibitory effect extends to melanogenesis and it reportedly improves melasma when administered orally or topically.31,32TXA inhibits angiogenesis and basic fibroblast growth factor-induced neovascularization, reducing erythema and pigmentation.33This anti-angiogenic effect is believed to be mediated by a decrease in the expression of vascular endothelial growth factor and endothelin-1, both of which play crucial roles in the vascular theory of melasma pathogenesis.34
Different TXA routes of administration, such as oral intake, intradermal injections,microneedling,iontophoresis,and topical application,have been utilized to treat melasma.35However, several studies have indicated that oral TXA is more effective and better suited for managing melasma than the other routes.36Although oral TXA has shown better results than those of placebo, the differences were not statistically significant.37,38Clinical trials evaluating the use of topical TXA at concentrations of 2%–5%applied twice daily have shown clinical improvement,significantly reducing the MASI score and causing fewer side effects compared with that of other treatments such as hydroquinone with topical steroids.39While there is no universal treatment plan for melasma,the ultimate objective is to decrease pigment production and levels and to enhance pigment clearance to restore pigment equilibrium.40The number of RCTs available for the meta-analysis was limited, and the outcomes and participant demographics varied across studies, which restricted the conclusions that could be drawn from the study.
5.Conclusion
This meta-analysis indicated no significant difference in efficacy and effectiveness between the combination therapy(laser and TXA)therapy and monotherapy.Treatment side effects were higher in the combination group than in the control group.However,notably,the limited number of RCTs in this meta-analysis and the lack of potential outcomes suggest the need for large-scale studies to provide more conclusive evidence.
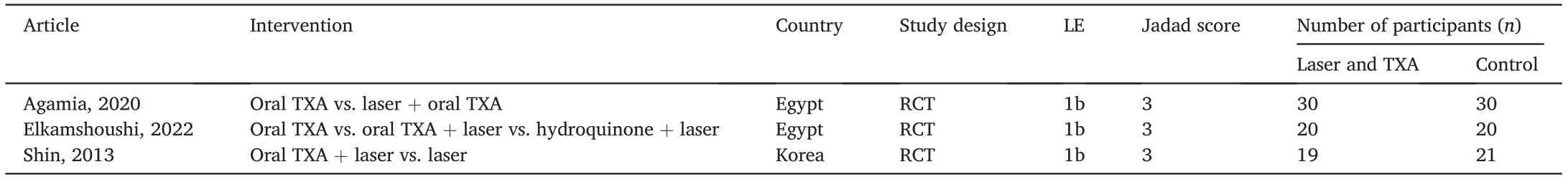
Table 1 Study quality characteristics.

Fig.2.Forest plot comparison of MASI scores.
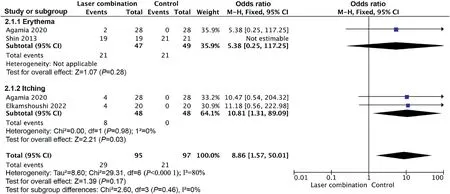
Fig.3.Forest plot comparison of treatment adverse events.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented for the publication.
Authors’ contributions
Sri A: Conceptualization, Validation, Writing-Review and editing,Supervision.Arika L: Methodology, Software, Writing-Original Draft,Data Curation.Probo Y: Project administration, Writing-Review and editing.Aulia S:Formal analysis,Investigation,Visualization.
Declaration of competing interests
The authors declare that they have no competing interests.
 Chinese Journal of Plastic and Reconstructive Surgery2023年3期
Chinese Journal of Plastic and Reconstructive Surgery2023年3期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Application of a jigsaw puzzle flap based on free-style perforator to repair large scalp defects after tumor resection: A case series
- Eight-year follow-up on postoperative improvement protocol in extensive metoidioplasty transgenders: A case series
- Absolute ethanol embolization for treatment of peripheral arteriovenous malformations
- Efficacy of tibial transverse transport combined with platelet-rich plasma versus platelet-rich plasma alone in the treatment of diabetic foot ulcers: A meta-analysis
- A randomized clinical trial assessing the efficacy of single and multiple intralesional collagenase injections for treating contracted scars
- Integrated percutaneous sclerotherapy and surgical intervention for giant cutaneomucosal venous malformation from TIE2 mutation: A case report
