Absolute ethanol embolization for treatment of peripheral arteriovenous malformations
Jingwei Zhou, Chen Hua, Xi Yang, Yuxi Chen, Yunbo Jin, Xiaoxi Lin
Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200011, China
Keywords:Arteriovenous malformation Embolization Ethanol
A B S T R A C T
1.Introduction
Most arteriovenous malformations (AVMs) are congenital high-flow vascular diseases caused by defects in blood vessel formation during embryonic development;however,the exact cause of AVM remains unknown.They comprise feeding arteries, draining veins, and arteriovenous shunts joined by aberrant fistulas that bypass the capillary network.Lesions may be asymptomatic at birth and can progressively grow or rapidly increase in size during puberty or pregnancy.1,2The exact prevalence of sporadic peripheral AVM remains unclear.According to recent research,the 5-year prevalence of peripheral AVM is approximately 2.15–6.60 in 1 000 000 in the Chinese population,with no significant difference in the incidence of AVM between men and women(~1.22:1 ratio).3,4
Most peripheral AVMs occur in the head and neck region.Clinically,they manifest as excessive tissue growth, congestion, redness, and swelling, with elevated skin temperature, pain, and bleeding, and can lead to heart failure in severe cases.5AVM is a highly dangerous type of vascular anomaly that, if left untreated, can lead to critical and potentially life-threatening consequences.6The pathogenesis of AVMs is not yet clear.Although AVMs usually present as sporadic cases, in certain cases, researchers have identified corresponding genetic mutations.Examples include hereditary hemorrhagic telangiectasia (HHT), an autosomal dominant genetic disease associated with mutations in the ENG, ACVRL1, and SMD4 genes; capillary malformation-AVM(CM-AVM), an autosomal dominant genetic disease caused by RASA1 and EPHB4 gene mutations; and PTEN hamartoma tumor syndrome(PHTS),which is associated with PTEN gene mutations.4,7–9
Treating AVMs is challenging and recurrence rates are high.Treatment options include laser,surgery,interventional embolization therapy,and combination therapy.With the development of endovascular treatment techniques and a deeper understanding of the disease itself, interventional embolization therapy has become one of the first-line methods for treating AVMs due to excellent outcomes,relatively low invasiveness,and increased safety.10This article introduces the characteristics and classification of AVMs while focusing on the method, mechanism, and key points of ethanol treatment.
2.Staging, classification, and treatment of AVMs
2.1.Staging and classification of AVMs
In clinical practice, staging of AVMs commonly uses the Schobinger system.Based on disease progression and corresponding clinical symptom characteristics, classification includes four stages(Table 1): stage I:quiescence; stage II: expansion; stage III: destruction; and stage IV:decompensation.2,11The Schobinger clinical staging helps determine the appropriate timing for treatment.Generally, stage I does not require specific treatment; patients in stage II may receive appropriate intervention after evaluation of benefits and drawbacks,while those in stages III and IV require timely treatment.12Considering that AVM lesions may expand without treatment, patients in early stages require regular follow-up screening via Doppler ultrasound or MRI to monitor their condition.
Based on the angioarchitecture of AVMs,different subtypes have been recognized.Currently,two classification systems are commonly used:the Cho and Yakes (Tables 2 and 3).13–16These classifications based on findings from digital subtraction angiography(DSA)provide a systematic reference for the morphological characteristics of different AVMs,hence assisting medical experts to develop individualized treatment options and assess prognosis.Due to the complexity of the disease,prognosis and treatment plans for different types of AVM may differ.If the treatment plan is not appropriate, the lesion may enter a “proliferation state,” in which case the evolution of AVM may accelerate in short time, causing serious complications, such as massive bleeding, that are difficult to handle.6Thus, it is of the utmost importance to select a treatment strategy that is appropriate in light of the current state of the disease.
2.2.Treatment options for AVMs
The treatment goals for AVMs comprise elimination of arterial-venous shunting and symptom relief,including surgical excision,interventional embolization,ablation therapy,and laser therapy.Laser may be useful for superficial lesions,as penetration depth is limited.17Surgery is one of the primary treatment methods for AVMs and can be performed for localized lesions.However, major bleeding resulting from a high-flow fistula can occur during the procedure;in addition,late-stage large or diffuse lesions are challenging to remove completely, leading to a high rate of recurrence and increased likelihood of postoperative complications.Thus,the procedure is preferentially used to improve patient appearance after intervention.Consequently, surgery now mostly serves as a supplementary procedure to embolotherapy to ensure better outcomes regarding patient appearance.2,5,18,19
With the development of interventional techniques and improvement of embolic agents such as Onyx, n-butyl 2-cyanoacrylate (NBCA), and absolute ethanol, intravascular embolization has become the first-line treatment for AVM.20This approach can help control acute bleeding,and preoperative embolization will significantly reduce the risk of bleeding during future surgery.Although the traditional embolic agents Onyx and NBCA can show satisfactory short-term effects,their use often leads to a high recurrence rate in long-term follow-up due to their inability to destroy the vascular endothelial cells in the nidus.Coil embolization is effective for AVMs with massive aneurysms; however,the method has the potential risk of coil migration and is not appropriate for superficial lesions.21–23
In recent years,targeted drug therapy for vascular malformations has made considerable progress.24Medications tested in several clinical trials have shown positive outcomes in patients with HHT or CM-AVM,which feature distinct germline inherited mutations.Rapamycin has been found to be effective for patients with AVMs associated with PTEN gene mutations.25Researchers have also noted improvements in liver lesions,telangiectasis, and refractory gastrointestinal bleeding in patients with HHT treated with the vascular endothelial growth factor (VEGF) inhibitor bevacizumab.26In patients with CM-AVM caused by RASA1 mutation, the mitogen-activated protein kinase (MEK) inhibitor trametinib has been reported to prevent lesion progression.27Currently, targeted therapies are mostly in the research phase and administered to patients in late stages who cannot receive other treatments or as adjunctive therapeutic approaches.The safety and efficacy of targeted therapies for treatment of peripheral vascular malformations require further verification and exploration through clinical studies with larger sample sizes.Thus,interventional treatment remains the first-line therapy for patients with AVM.

Table 1 Schobinger clinical staging of AVMs.
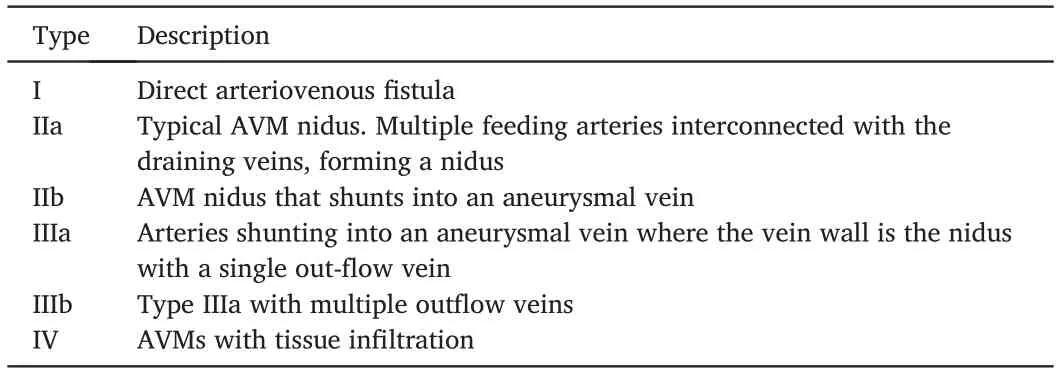
Table 2 Yakes classification of AVMs.
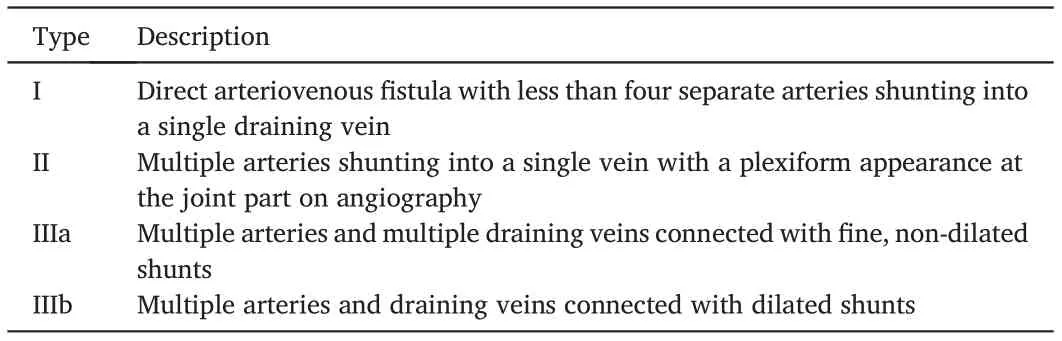
Table 3 Cho classification of AVMs.
3.Absolute ethanol embolization for AVM management
3.1.History and development of ethanol embolization
In 1986,Yakes et al.first reported the use of absolute ethanol for the treatment of extracranial AVM and achieved good treatment outcomes.28Since then, absolute ethanol as an embolic agent has provided a new route for interventional treatment of AVMs.Unlike traditional embolic agents that physically block the vessel for a period of time, injection of ethanol into the vascular malformation nidus can cause endothelial cell damage,shedding,hemoglobin denaturation,rapid platelet aggregation,and thrombosis, effectively occluding the blood vessel.Compared with other embolic agents, ethanol can completely destroy the endothelial cells, preventing endothelial production of chemotactic and angiogenic factors, blocking the process of neovascularization, and achieving excellent treatment results.29,30
Interventional therapy was often utilized as an adjuvant treatment before surgery in the past because it can cut off blood supply to the lesion,thereby lowering the risk of intraoperative hemorrhage.Owing to its unique mechanism of action,absolute ethanol can become a standalone treatment method for AVMs.31,32If performed properly,absolute ethanol interventional therapy can eradicate AVM lesions.For large diffuse lesions, multiple treatments are often required to achieve a cure.For patients with life-threatening conditions,such as massive hemorrhage and hemodynamic symptoms due to extensive lesions, intervention with absolute ethanol can also be used to control acute symptoms or as a palliative treatment.29,33
Previous studies have found that approximately 80% of patients experience symptom improvement after treatment, with ~40%–50%showing full recovery.34–36AVM is a highly recurrent vascular anomaly,with surgical recurrence rates of 81% and interventional embolization recurrence rates of 98%in a follow-up study of 272 individuals.2Owing to the high efficiency of ethanol embolization, the probability of recurrence is expected to decrease.In the study by Kim et al., the recurrence rate of head and neck AVMs among patients treated solely with absolute ethanol embolization was 18.2%.37In a long-term follow-up study,of the 35 patients with auricular AVMs who were treated with ethanol,only one experienced recurrence during the follow-up period.10Although the mechanism of AVM recurrence is currently unclear,residual lesions play an important role and higher clinical staging is associated with a higher recurrence rate after treatment.2,37Precise superselected ethanol embolization, using a microcatheter, allows access to small and distant nidi,enhancing the effectiveness of the procedure and decreasing the chance of recurrence.38Based on these evaluations,ethanol embolotherapy has already become the first-line treatment method for peripheral AVMs.
3.2.Key points in ethanol embolization therapy
Embolization with absolute ethanol plays a key role in the treatment of peripheral AVMs of the head, neck, and limbs.After treatment,symptoms such as pain, swelling, bleeding, and ulceration can be considerably alleviated or even healed, leading to improvement in the patients’ quality of life.Even in cases of complicated vascular malformations, ethanol has demonstrated positive therapeutic results when administered under standardized protocols.It is considered an efficient,reliable,and relatively safe treatment method.39–43
Embolization treatment generally includes three methods, transarterial, transvenous, and direct percutaneous puncture, to inject absolute ethanol into the lesion nidus of AVMs.The transarterial approach is generally suitable for patients with a small number of feeding arteries and lesions that are easily accessible via arterial catheters.When multiple(>3) arteries drain into a single vein, transvenous embolization may be more appropriate.In the presence of an excessive number of small,tortuous, and winding feeding arteries or in patients with unclear anatomical structures surrounding the lesion due to previous treatment,percutaneous puncture may be the preferred technique.40,44,45
To obtain better outcomes, the strategies used to treat AVMs vary depending on angiographic (DSA) classification.14,46A summary of embolization techniques is presented below based on the Cho classification.For type I lesions, direct occlusion of the fistula between artery and vein with embolic agents is recommended.In type II lesions, the arteriovenous shunts are located on the vascular wall of the draining vein.A coil is usually placed in the enlarged draining vein to slow down blood flow, and absolute ethanol is then injected to destroy the remaining lesion.Because the majority of type IIIa lesions contain tiny fistulas and are located superficially, diluted ethanol is used to prevent skin necrosis.Treatment includes delivering a transarterial catheter into the feeding artery of the lesion and injecting diluted ethanol(50%–60%)mixed with a contrast agent.Treatments for type IIIb usually comprise transarterial intervention or percutaneous puncture to inject high-concentration ethanol (80%–100%) into the lesion.For enlarged fistulas, coil occlusion can be used to reduce the amount of ethanol required.Studies have indicated the most favorable outcomes for types I and II, with a cure rate exceeding 80%.The lowest therapeutic efficacy has been recorded for type IIIa, with a cure rate of only 19% and the highest average number of treatment sessions.The cure rate for the most prevalent type IIIb AVMs is approximately 30%.6,36,46In addition, the extent of lesion involvement can affect treatment outcomes, and localized type IIIa AVMs can achieve favorable results in multiple sessions.34
Due to the potential risks associated with ethanol,careful evaluation of the risks of disease progression and iatrogenic complications is crucial,and strict monitoring of indications is required.In addition to the vascular angiographic classification, the choice of treatment methods should also consider the patient’s clinical symptoms and disease staging.Embolism aims to alleviate bleeding,pain,ulceration,and necrosis rather than simply occlude blood vessels.47
Controversy regarding the indications for interventional therapy for AVM is currently ongoing.AVMs do not regress spontaneously, and, as the disease progresses,not only will AVM volume increase but AVMs will also infiltrate surrounding normal tissues, making disease management more difficult and leading to a poor prognosis in later stages.Some physicians believe that, even in the absence of clinical symptoms, early intervention is necessary.Considering that stage III and IV lesions are likely to progress and cause massive hemorrhage,some experts advocate that treatment is necessary.In contrast,patients in stages I or II without obvious clinical symptoms do not require specific treatment but can instead be monitored for changes via regular Doppler ultrasound followup.If patients in stage II present localized lesions and the angiographic morphology is suitable for interventional therapy,treatment may also be considered.2,38,48,49Personalized treatment is important in patients with AVM.Generally, for patients in stage II or above, we recommend early treatment because later treatments have been associated with larger lesions,are less favorable for complete cure,and are often accompanied by sequelae.Patients in early stage, on the other hand, often seek medical treatment for appearance concerns.They can be either followed up or treated depending on their wishes after risk evaluation.Targeted drugs in clinical trials may be an option for patients in late stage when other treatments are not possible.
3.3.Prevention and management of complications
Absolute ethanol as an embolic agent has significant therapeutic effects,but if it enters the non-affected circulatory system due to improper operation, it can cause various complications, such as tissue swelling,blisters,ulcers,pain,and sensory impairment.In severe cases,non-target embolization of normal tissues may result in local tissue necrosis and even pulmonary artery hypertension if large amounts of ethanol are injected into the systemic circulation.6,30The incidence of complications varies in different studies, with recent studies reporting a rate of approximately 6%–26%,of which skin necrosis and blisters are the most common complications.Over 80% of complications recover spontaneously or through conservative treatment without sequelae.Approximately 1.8%–7.0% of patients may experience severe complications,such as skin necrosis requiring skin grafting, paralysis, or other serious complications that require additional treatment.10,14,36,37,46,50The injection technique for absolute ethanol, number and interval of sessions,and classification of lesions can all affect the occurrence of complications.Park et al.discovered that the incidence of complications when using absolute ethanol is higher than that with diluted ethanol and mixed embolic agents.The embolization method, too, can increase the risk of complications, with the highest incidence rates associated with combined transarterial and transvenous catheter embolization.36Additionally,the angiographic classification of AVMs influences the incidence of complications, with Yakes type IV and Cho types IIIa and IIIb being associated with a greater risk.14Moreover, according to one study,recurrent embolization is associated with the incidence of complications,and the larger the number of sessions,the greater the probability.50
Pulmonary arterial hypertension is one of the most severe complications of ethanol sclerotherapy.After injection, some ethanol flows back into the left heart and pulmonary artery through veins,causing spasms of small blood vessels or extensive microthrombi, eventually leading to pulmonary arterial hypertension.Pulmonary arterial hypertension is extremely dangerous and can rapidly develop into cardiopulmonary collapse if not controlled immediately.51,52To prevent such complications,the absolute ethanol dosage used in each session should be strictly limited.The currently recognized maximum dosage is 1 mL/kg.Injecting more than 0.14 mL/kg every 10 min causes significant hemodynamic changes that lead to increased pulmonary artery pressure.Therefore,single ethanol injection volumes should also be restricted to reduce associated risks.20,53,54In addition, when the injected volume reaches 0.5 mL/kg, monitoring of pulmonary artery pressure through a Swan-Ganz catheter is necessary.Vasodilator therapy should be administered to prevent the occurrence of pulmonary arterial hypertension when the pulmonary artery pressure exceeds 25 mmHg.6,10,12
To avoid intense pain caused by the stimulation of the vascular wall nerves during the injection of absolute ethanol, treatment needs to be performed under general anesthesia to alleviate patient discomfort.Selecting the most appropriate embolization method for different types of lesions helps reduce the occurrence of complications.Direct percutaneous puncture has been associated with a reasonably low incidence of complications and good treatment outcomes for AVMs that are difficult to reach using a catheter due to tortuous vessels.Placing coils can lower lumen volume and flow velocity in the nidus and generate turbulence,which improves contact between ethanol and the vascular wall,leading to the destruction of the endothelium.Using diluted ethanol or combined methods, such as flow restriction with coils, can reduce the amount of absolute ethanol used and thus lower the incidence of complications.36,37,55
4.Conclusion
Due to its unique physical and chemical features,absolute ethanol has become one of the most common treatments for AVM.It can cause hemoglobin denaturation, directly destroy the vascular endothelium,leading to formation of aggregates and thrombi to occlude blood vessels,and block vascular recanalization, thereby exhibiting outstanding therapeutic benefits.Despite its extraordinary efficiency,the use of absolute ethanol poses certain risks that necessitate extreme caution and careful preoperative assessment and monitoring by skilled physicians to limit the incidence of associated complications.
Absolute ethanol interventions currently used in the clinical practice have some limitations.For certain types of AVMs, such as extensive diffuse AVMs,a curative effect may be difficult to achieve using ethanol embolization alone.In such cases, individualized treatment plans tailored to different subtypes,phased sessions,or combination therapies may be necessary.These approaches can help reduce adverse events and improve treatment outcomes.Although ethanol is not radiopaque, physicians cannot directly observe its filling range under DSA, which necessitates the development of new embolic agents with similar effects and better visibility in the future.In addition, for certain nidi with excessively high blood flow velocity or nidi connected to an aneurysm,exposure to ethanol is of limited duration,shortening contact time with the vascular endothelium and reducing therapeutic efficacy.Mixed embolic agents consisting of NBCA,iodized oil,and ethanol have shown good embolization effects in in vitro experiments,providing new insights for future embolization choices for AVMs.56
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented for the publication.
Authors’ contributions
Zhou J: Conceptualization, Writing-Original draft.Hua C: Writing-Review and editing.Yang X: Writing-Review and editing.Chen Y:Writing-Review and editing.Jin Y: Writing-Review and editing.Lin X:Funding acquisition, Conceptualization, Supervision, Writing-Review and editing.
Declaration of competing interests
Lin X is an editorial board member for Chinese Journal of Plastic and Reconstructive Surgery and was not involved in the editorial review or the decision to publish this article.All authors declare that there are no competing interests.
Acknowledgments
This work was supported by Rare Disease Registration Platform of Shanghai Ninth People’s Hospital,Shanghai Jiao Tong University School of Medicine (grant no.JYHJB02).
 Chinese Journal of Plastic and Reconstructive Surgery2023年3期
Chinese Journal of Plastic and Reconstructive Surgery2023年3期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Application of a jigsaw puzzle flap based on free-style perforator to repair large scalp defects after tumor resection: A case series
- Eight-year follow-up on postoperative improvement protocol in extensive metoidioplasty transgenders: A case series
- Efficacy of tibial transverse transport combined with platelet-rich plasma versus platelet-rich plasma alone in the treatment of diabetic foot ulcers: A meta-analysis
- Efficacy, effectiveness, and safety of combination laser and tranexamic acid treatment for melasma: A meta-analysis
- A randomized clinical trial assessing the efficacy of single and multiple intralesional collagenase injections for treating contracted scars
- Integrated percutaneous sclerotherapy and surgical intervention for giant cutaneomucosal venous malformation from TIE2 mutation: A case report
