Efficacy of tibial transverse transport combined with platelet-rich plasma versus platelet-rich plasma alone in the treatment of diabetic foot ulcers: A meta-analysis
Ke Chen, Yikng Yu, Jilu Shu, Binin Zhng,*, Gng Wng, Bin Wu
a Department of Orthopedics,Xinhua Hospital of Zhejiang Province,The Second Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou 310003, Zhejiang,China
b School of Pharmaceutical Sciences, Zhejiang Chinese Medical University, Hangzhou 311403, Zhejiang, China
c First Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou 310053, Zhejiang, China
d Department of Emergency Surgery, Xinhua Hospital of Zhejiang Province, The Second Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou 310003,Zhejiang, China
Keywords:Tibial transverse transport Platelet-rich plasma Diabetic foot ulcer Growth factor Meta-analysis
A B S T R A C T
1.Introduction
Foot ulcers are the main complications of diabetes and have a high incidence and mortality rate.This is the main reason for hospitalization and amputation in patients with diabetes.The prevalence rate is as high as 25%,the annual incidence rate is approximately 2%,and the lifetime incidence rate is between 15%–25%.1,2Treatment of foot ulcers is challenging because of the many causes of foot ulcers.This places a heavy burden on patients,healthcare systems,and society.Even when diabetic ulcers are successfully treated, the risk of recurrence remains high.The recurrence rate of ulcers within the first year of healing is reportedly 30%–40%.Therefore,prevention of foot ulcers is of vital importance and has long been regarded as a priority by the International Diabetes Foot Working Group.
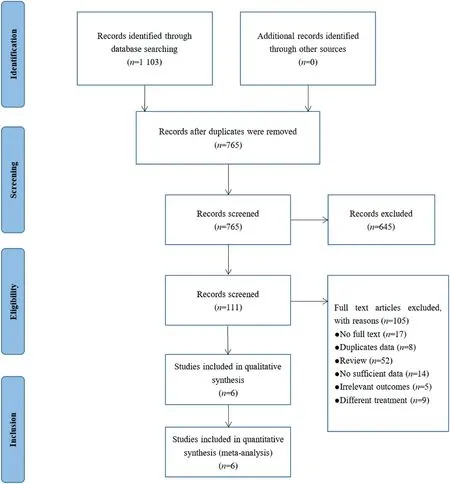
Fig.1.Retrieval process diagram.
Platelets are a rich source of natural growth factors that promote tissue repair and regeneration.Platelet-rich plasma (PRP) gels are increasingly used in almost all surgical fields to treat various soft and hard tissue defects.The most significant role is to accelerate bone formation and treat chronic non healing wounds.3,4The tibial transverse transport (TTT) technique, also referred to as the Ilizarov technique,distinguishes itself from the conventional approach of longitudinally displacing osteotomy segments during limb lengthening.This surgery involves lateral traction of the bone cortex on the tibial shaft.The purpose of TTT is not osteogenesis but the regeneration of local vascular tissue.According to the law of stress-tension,continuous stretching of the tibial cortex can promote cell metabolism,accelerate tissue regeneration,rebuild microcirculation, and restore blood oxygen supply to the lower limbs.This surgical procedure involves applying lateral traction to the bone cortex located on the tibial shaft.The objective of TTT is not osteogenesis but rather the regeneration of vascular tissue in the affected area.In accordance with the principle of stress-tension, persistent stretching of the tibial cortex can enhance cellular metabolism,expedite tissue regeneration, reconstruct microcirculation, and reinstate blood oxygen supply to the lower extremities.Currently, the TTT is primarily used to treat chronic ischemic conditions affecting the lower limbs.By 2021,this technology has been developed in the field of public relations in China for a full 20 years.The scope of its applications has broadened from obliterative thrombovasculitis to chronic ischemic conditions affecting the lower extremities, such as diabetic foot ulcers (DBFUs),obliterative thrombovasculitis, and arteriosclerotic obliteration, with a particular emphasis on DBFUs.5This study aims to gather and analyze data on the effectiveness of TTT and PRP as therapeutic interventions for DBFUs, while also comparing the respective merits and drawbacks of these two technologies in managing this specific condition.
2.Materials and methods
2.1.Search strategy
The PubMed, Cochrane Library, Web of Science, EMBASE, Chinese Biomedical Literature, CNKI, VIP, and Wanfang databases had no language restrictions in their related research from their establishment until December 15, 2022.Abstracts of title and key words used in the paper retrieval were: “tibial transverse transport,” “tibial transverse transport technique,” “Ilizarov technique,” “tibial transverse transport technology,” “platelet rich plasma,” “PRP,” “diabetes foot ulcer,” “diabetes ulcer,”“diabetes”and“ulcer.”
Using PubMed as an example,the retrieval formula was as follows:#1 tibial transverse transport OR #2 tibial transverse transport technique OR #3 Ilizarov technique OR #4 tibial transverse transport technology AND#5 platelet-rich plasma OR#6 PRP AND#7 diabetes foot ulcer OR#8 diabetic ulcer OR#9 ulcer.
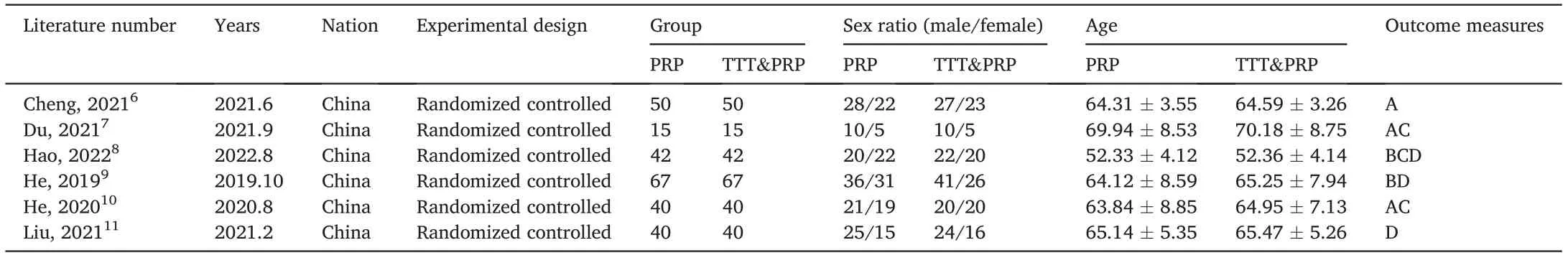
Table 1 Basic information of the included literature.
2.2.Inclusion criteria
(1) Research type: clinical controlled trials, including retrospective cohort studies and randomized controlled studies.(2) The diagnosis of diabetic ulcers does not include a definitively diagnosed traumatic ulcer.(3) The original materials of Chinese and English literature were published in full text.
2.3.Exclusion criteria
(1) Research groups not defined or grouped.(2) Nonrandomized controlled trials, non-cohort studies, non-case-control studies, retrospective studies, and case reports.(3) Repetitive research and animal experimentation.(4) Ulcers caused by other diseases.(5) Conservative treatment or non-invasive treatment.
2.4.Quality evaluation
Two researchers used the RevMan 5.4 software bias assessment tool to evaluate the risk of bias in their articles.The evaluation included the random allocation method, allocation scheme hiding, blinding of research object and implementer, blinding of research result measurement,result data integrity,selective reporting,and other deviations.The evaluations for each project are“low risk,” “high risk,”and“unclear.”
2.5.Observational clinical results
The effective rate, quality of life score before and after treatment(treatment impact, physiological function, psychological function, and social function), serum levels of growth factors (EGF, VEGF, bFGF, and PDGF)before and after treatment,and wound healing(wound reduction rate, bacterial clearance rate, granulation tissue coverage rate, and granulation tissue growth thickness) were assessed.
2.6.Statistic analysis
The extracted data were statistically analyzed using Review Manager software (version 5.3) provided by the Cochrane Library Collaboration Network, and I2heterogeneity of data was included in the value judgment.If I2<50% and Q tests showed P>0.1, they indicated low heterogeneity between the study groups.Therefore, a fixed effects model was used for analysis.If I2≥50% and Q-test showed P≤0.1, they indicated high heterogeneity between the study groups, and a random effects model was used for analysis.The decrypted variable data were analyzed using hazard ratios (HR) and 95% confidence intervals (CIs).For continuous variables, we used the weighted mean difference (MD) and 95% CI to calculate the effect magnitude and 95% confidence interval,respectively.After comparing the various indicators,if P<0.05,there was a significant difference.
3.Results
3.1.Included studies
A preliminary search of 1 103 papers was conducted, and duplicate papers were checked and deleted using EndNote and Noteexpress(n=765).After reading the titles and abstracts according to the exclusion criteria, 654 were excluded and 111 were initially included.After reading the entire text,six studies were included in the meta-analysis,all of which were publicly published clinical controlled studies and randomized controlled studies.The retrieval process is illustrated in Fig.1.There were 283 patients in the TTT&PRP groups:254 in the PRP group and 44 in the TTT group.Basic information on the included studies is presented in Table 1.The results of the bias risk assessment are shown in Fig.2.
3.2.Meta-analysis
3.2.1.Effective rate
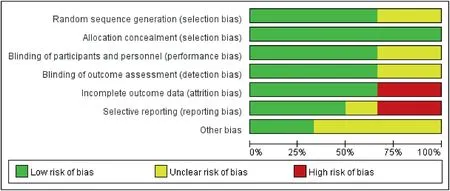
Fig.2.Results of the bias risk assessment.

Fig.3.Comparison of treatment effectiveness.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
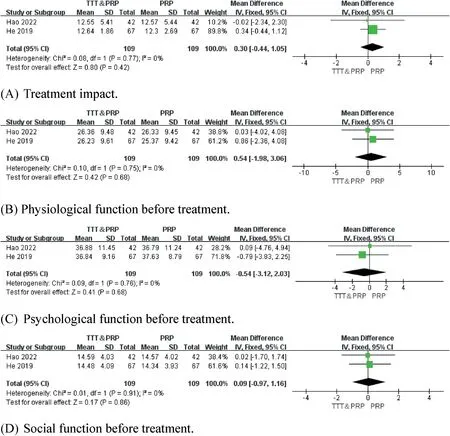
Fig.4.Comparison of quality of life scores before treatment.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
Three of the six articles included, showed a detailed comparison of treatment effectiveness.There was significant heterogeneity among the studies,and a random-effects model was used for the meta-analysis.The efficacy rate in the TTT&PRP group was higher than that in the PRP group(P=0.000 6;Fig.3).
3.2.2.Quality of life score before and after treatment
(1) Quality of life score before treatment
Two of the six articles included showed a detailed comparison of the quality of life scores before treatment.There was little heterogeneity between the studies, and a fixed-effects model was used for metaanalysis.There were no significant differences in the treatment impact,psychological function, physiological function, or social function between the TTT&PRP and PRP groups before treatment(P>0.05;Fig.4).
(2) Quality of life score after treatment

Fig.5.Comparison of quality of life scores after treatment.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
Two of the six articles included, showed a detailed comparison of quality of life scores after treatment.There is a significant heterogeneity in the impact of postoperative treatment in the literature,and a randomeffects model was used for the meta-analysis.As there is little heterogeneity in postoperative psychological, physiological, and social functions in the literature, a fixed-effects model was used for the metaanalysis.The TTT and PRP groups were superior to the PRP group in terms of treatment impact, psychological function, physiological function,and social function after treatment(P<0.05;Fig.5).
3.2.3.Serum levels of growth factors before and after treatment
(1) Serum levels of growth factors before treatment
Three articles presented a detailed comparison of serum growth factors before treatment.There was little heterogeneity among the studies,and a fixed-effects model was used for the meta-analysis.There were no significant differences in serum EGF, VEGF, bFGF, and PDGF levels between the TTT&PRP,and PRP groups(P>0.05;Fig.6).
(2) Serum levels of growth factors after treatment
Three articles presented a detailed comparison of serum growth factors before treatment.There was significant heterogeneity in postoperative EGF levels between the studies, and a random-effects model was used for the meta-analysis.There is little heterogeneity in the postoperative VEGF, bFGF, and PDGF levels in the literature, and a fixedeffects model was used for the meta-analysis.The TTT&PRP group showed a significant increase in serum EGF, VEGF, bFGF, and PDGF levels compared to the PRP group(P<0.05;Fig.7).
3.2.4.Wound healing after treatment
Three articles compared postoperative wound reduction rate, bacterial clearance rate, granulation tissue coverage rate, and granulation tissue growth thickness.There was significant heterogeneity in the wound reduction rate and granulation tissue coverage among the studies,and a random-effects model was used for meta-analysis.There was little heterogeneity in the bacterial clearance rate and granulation tissue growth thickness among the studies,and a fixed-effects model was used for meta-analysis.The TTT&PRP group showed better postoperative wound reduction rate, bacterial clearance rate, granulation tissue coverage rate, and granulation tissue growth thickness than the PRP group(P<0.05;Fig.8).

Fig.6.Comparison of serum growth factors before treatment.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
4.Discussion
The incidence of diabetes is increasing annually owing to the increasing degree of population aging and improvement in living standards.DBFUs are one of the main complications of diabetes,with a high prevalence and recurrence rate.12–14Compared with patients without diabetic ulcers, patients with diabetic ulcers face a higher risk of death.15,16The factors related to the healing of foot ulcers in diabetes are very complex, including reduced perfusion, edema, pain, infection,metabolic disorder,malnutrition,weightlessness,wound treatment,foot surgery, and treatment strategies for complications.Restriction of local blood transport is an important cause of DBFUs.The key to treatment is restoring the blood circulation of the tissue around the DBFUs.It can be seen from this that the key to the treatment is to restore the blood circulation of the tissue around the DBFU.Reconstruction of the microcirculation in the lower limbs relies on vascular reconstruction; therefore,improving the expression of angiogenic factors is key to treating DBFUs.17
Currently, there are various surgical treatments for DBFUs, such as transplanting fat, PRP, and platelet-rich fibrin to repair tissues that are difficult to heal after infection.Lower extremity artery bypass grafting,lumbar sympathetic ganglion destruction, extracorporeal circulation of lower extremity vessels, pressure perfusion therapy, and tibial lateral metastasis technology can be used to reconstruct the microcirculation of the lower extremities of DBFUs and improve blood circulation in the surrounding tissues.18At present, the use of PRP has become a very popular treatment method for DBFUs.In the study of Ullah et al.the effectiveness of PRP in the treatment of DBFUs can reach 80%.19PRP is activated to form platelet-rich gels,platelet α granules release PDGF and other growth factors, participate in tissue repair, and have specific biomolecular functions such as anti-inflammatory, granulation tissue growth, and vascular nerve regeneration.Many studies have analyzed the effectiveness of PRP in the treatment of DBFUss.Through clinical evaluation and observation, Lei et al.concluded that PRP plus conventional treatment for diabetic foot was significantly better than simple treatment through clinical evaluation and observation.20

Fig.7.Comparison of serum growth factors after treatment.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
In recent years, the TTT has become a new treatment for diabetes.Lateral tibial bone transfer surgery stimulates tissue regeneration through the action of tension stress, thereby promoting synchronous growth of muscles, nerves, fascia, and blood vessels.21Sun et al.22followed up 20 patients and concluded that the Ilizarov TTT can promote the regeneration of foot blood vessels and rebuild the microvascular network, thus improving the blood circulation of patients with DBFUs and promoting the healing of ulcers.At present, a combination of TTT&PRP techniques has also been developed.Through clinical comparative analysis,Wu concluded that autologous PRP combined with the Ilizarov TTT bone grafting has a significant effect in the treatment of DBFUs, which can effectively shorten wound healing time, reduce complications, and reduce the pain and discomfort of patients.23Many studies have compared combination therapy of TTT&PRP or PRP alone for DBFUs.This review summarizes and analyzes these comparative studies and concludes that combination therapy can have higher efficacy,especially in terms of wound growth factor content.A combination of these two methods offers significant advantages.However,there are few clinical observational studies on TTT&PRP in the treatment of DBFUs;therefore,the literature included in this article is limited.
The limitations of this meta-analysis are as follows: first, due to the insufficient number of clinical samples, stronger evidence cannot be obtained; second, due to the heterogeneity between studies, we cannot rule out errors caused by subjective factors in these studies; third, this study lacks multicenter randomized experiments and requires more research to support these results.
5.Conclusion
In terms of treatment efficacy, the TTT&PRP treatment group had higher efficacy rates than the PRP group.In terms of quality of life before and after treatment, there were no significant differences between the TTT&PRP and PRP groups in terms of treatment impact, psychological function, physiological function, and social function before treatment.After treatment, the TTT&PRP group was superior to the PRP group in terms of treatment impact, psychological function, physiological function, and social function.Before and after treatment, there were no significant differences in serum EGF,VEGF,bFGF,and PDGF levels between the TTT&PRP, and PRP groups.After treatment, the TTT&PRP group showed a significant increase in serum EGF, VEGF, bFGF, and PDGF levels compared to those in the PRP group.Regarding wound healing after treatment, the TTT&PRP group performed better than the PRP group in terms of postoperative wound reduction, bacterial clearance,and granulation tissue coverage rates, and granulation tissue growth thickness.
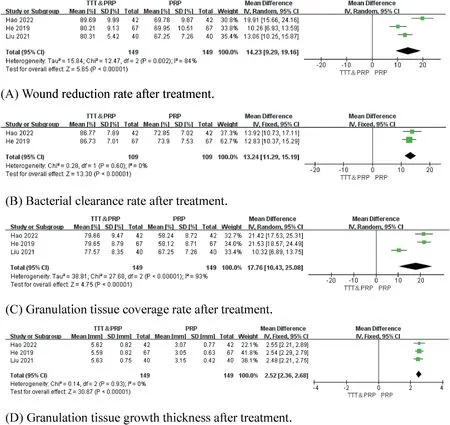
Fig.8.Comparison of wound reduction rate after treatment.PRP, platelet-rich plasma; TTT&PRP, tibial transverse transport and platelet-rich plasma treatment.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All the authors have consented for the publication.
Authors’ contributions
Chen K: Data curation, Writing-Original draft.Yu Y: Investigation,Validation.Shu J:Investigation,Validation.Zhang B:Supervision.Wang G: Visualization.Wu B:Visualization.
Declaration of competing interests
The authors declare that they have no competing interests.
Acknowledgments
This work was supported by the Zhejiang Province Traditional Chinese Medicine Science and Technology Program Project (grant no.:2023ZL429).
 Chinese Journal of Plastic and Reconstructive Surgery2023年3期
Chinese Journal of Plastic and Reconstructive Surgery2023年3期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Application of a jigsaw puzzle flap based on free-style perforator to repair large scalp defects after tumor resection: A case series
- Eight-year follow-up on postoperative improvement protocol in extensive metoidioplasty transgenders: A case series
- Absolute ethanol embolization for treatment of peripheral arteriovenous malformations
- Efficacy, effectiveness, and safety of combination laser and tranexamic acid treatment for melasma: A meta-analysis
- A randomized clinical trial assessing the efficacy of single and multiple intralesional collagenase injections for treating contracted scars
- Integrated percutaneous sclerotherapy and surgical intervention for giant cutaneomucosal venous malformation from TIE2 mutation: A case report
