Supraclavicular artery island flap for reconstruction of hypopharynx and upper esophagus defects: A case report and literature review
Xiorong M, Xioting Sun, Yuexin Shi, Kiyng Lv,*, Wenbin Chen,b,**
a Department of Plastic and Reconstructive Surgery, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200092, China
b Department of Plastic Surgery, Huai’an Second People’s Hospital, Huai’an 223022, Jiangsu, China
Keywords:Pharyngo-esophageal fistula Supraclavicular artery island flap Head and neck reconstruction Pedicled flap Complications
A B S T R A C T
1.Introduction
Hypopharyngeal cancers account for 3%of all head and neck cancers.Simple radiotherapy or chemotherapy offers palliative effect only as it has low survival rate.Surgical resection combined with radiation or chemoradiation is the predominant therapy.However,salvage surgery is accompanied by high complication rates (67.5%),1especially in the irradiated tissue.Pharyngocutaneous or pharyngoesophageal fistula is the most common life-threatening complication with a pooled incidence of 28.9%.Hypopharynx-esophageal defects are very challenging to reconstruct because of limited space.
Reconstructive surgery using skin color and texture similar to the original skin of the recipient site is not only for covering the defect,but also for recreating functional units in three dimensions.2Local,regional,or free flaps are often required to reconstruct hypopharyngeal and esophageal defects.Fritz3reported a free double-paddle posterior tibial artery (PTA) perforator flap for hypopharyngeal and neck reconstructions.The external island of the PTA flap resurfaced the outer neck skin defect and the inner one for the reconstruction of the hypopharynx.An external flap was used to monitor the inner flap survival.The two flaps were completely separated to ensure hypopharyngeal movement.However,free flap requires vessel anastomosis,which results in longer surgery time and high complication rate, especially when vessel anastomosis is performed in the irradiated region.
Owing to the wide arc of rotation and optimum skin texture of the supraclavicular artery island flap(SCAIF),it has been extensively used to cover head, oral, and neck defects after tumor resection.In the present case report, SCAIF was designed to reconstruct hypopharyngeal, esophageal,and neck skin defects simultaneously.
2.Case presentation
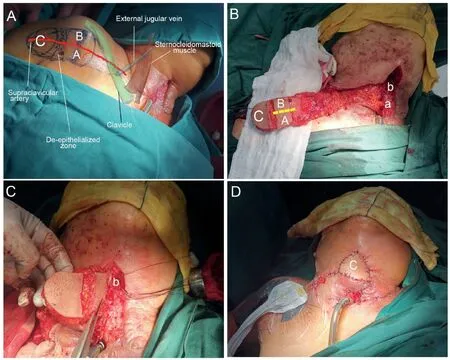
Fig.1.(A)Preoperative drawing of the supraclavicular artery island flap.(B)After flap harvesting,skin de-epithelization was performed on the proximal part of the flap and the zone between part AB and C.b indicates the hypopharynx defect while a indicates the upper esophagus defect.(C)Part AB flap was turned over to repair the upper esophagus (a) and hypopharynx defect (b).(D) Part C flap was turned over again to repair the neck skin defect.

Fig.2.(A)Electronic laryngoscope examination 12 days after operation.The blue dot line indicated part AB of the supraclavicular artery island flap;the red dot line indicated the leakage measuring approximately 0.5 cm×1.0 cm at the hypopharynx.(B)Electronic laryngoscope examination 30 days after operation.The leakage at the hypopharynx has healed without any surgical intervention.(C)Electronic laryngoscope examination 60 days after operation.There was no stricture at the site of repair.(D, E) Postoperative pictures at three and five months follow-up.(F) Panoramic photograph capturing the comprehensive view of both the reconstructed surgical area and the donor site at one year follow-up.

Fig.3.Barium radiography test conducted five months postoperatively confirmed the absence of any leakage or diverticulum at the repair site.(A)Front view.(B,C)Lateral view.
A 74-year-old female patient presented with laryngeal carcinoma(T4aN1M0) and underwent total laryngectomy, left functional neck dissection, partial thyroidectomy, and permanent tracheostomy three months ago.Hypopharyngeal esophageal defectswithskindefectspersisted forthreemonths.Theskindefectmeasuringapproximately4cm×3cmwas discovered on the patient’s neck during physical examination.The gastric tube was exposed,and there was a fistula below the defect that opened into the pharynx and esophagus and was surrounded by necrotic tissue.Upon further investigation, the patient reported no history of chemotherapy or radiation therapy to the neck.However,the patient had a 20-year history of hypertension and diabetes mellitus.She denied any other chronic illnesses or history of smoking or alcohol consumption.
Doppler ultrasound was used to determine the course of the transverse cervical and supraclavicular arteries before the operation to ensure the integrity of the vascular pedicle(Fig.1A).The patient was placed in a supine position with the shoulder pads elevated and the head tilted to the contralateral side.The SCAIF (7 cm × 21 cm) was designed at the supraclavicular and rotator cuff sites (Fig.1A).The integrity of the supraclavicular artery was exposed and carefully protected.The skin,subcutaneous tissue, and deltoid fascia were cut distal to the flap and sharply separated under the fascia.The tissue flap was turned proximally.The external jugular vein was retained and the pedicle was dissected to the starting point of the supraclavicular vessel, which was used as the rotation axis point.
After flap harvesting,skin de-epithelialization was performed on the proximal part of the flap and in the zone between parts AB and C(Fig.1B).The flap was then rotated toward the area of the neck defect.The part A flap repaired the upper esophageal defect(a),and the part B flap repaired the hypopharyngeal defect(b)(Fig.1C).The part C flap was turned over again such that the skin faced outward to repair the neck skin defect.Thus, part C flap could monitor the microcirculation of part AB flap (Fig.1D).The scapular donor site was subcutaneously undermined and closed by primary intention.
Electronic laryngoscopy revealed minor necrosis measuring approximately 0.5 cm×1.0 cm on part B flap at the hypopharynx 12 days after the operation(Fig.2A).It shrank gradually and closed 30 days after the operation without any surgical intervention (Fig.2B and 2C).The skin defect was well reconstructed using the part C flap of the SCAIF(Fig.2D and 2E).Fig.2F shows a panoramic photograph capturing the comprehensive view of both the reconstructed surgical area and the donor site at one year follow-up.Additionally, barium radiography conducted five months postoperatively confirmed the absence of any leakage or diverticulum at the repair site (Fig.3).
3.Discussion
Treatment for laryngeal tumors has changed from surgery to organpreserving nonsurgical modalities in the form of radiotherapy and concurrent chemoradiotherapy.Salvage total laryngectomy is only indicated in cases of recurrent tumors,residual tumors after completion of treatment,or when the toxicities of radiation or chemoradiation have rendered the larynx non-functional.4Radiation impaired the vessels and tissue,causing obliterative endarteritis and fibrosis,resulting in potential complications during wound healing after surgery; and these effects are magnified with the addition of chemotherapy.Hasan1reviewed that 859 of 3 147 patients who had a pharyngocutaneous fistula, with a pooled incidence of 28.9%.Individual series showed a wide variation in the rates of pharyngocutaneous fistula at 5.6%–73.0%.
Owing to the high morbidity of pharyngocutaneous fistulas, several free flaps and pedicled flaps have been described and validated to repair the defects.Some authors have reported that surgical practices have changed during the COVID-19 pandemic.The use of local or regional flaps, instead of free flaps, has become necessary.Some COVID-19 pandemic-related restrictions, such as the use of personal protective equipment including full-body suits and face shields may limit dexterity and visual acuity required for precise vascular anastomosis, lead to increased use of pedicled flaps.Compared with free flaps, pedicle flaps are more time-saving without the need for vascular anastomosis.5Patients can benefit from fewer medical complications, reduced length of hospital stay, and lower total hospital charges.6
SCAIF was first described by Lamberty7in 1979.Pallua et al.8conducted a detailed anatomical study of the flap in 1997 and improved the harvesting technique to confirm its safety and reliability.In 2009, Chiu et al.9proposed that SCAIF was multifunctional and reliable for treating defects after head and neck tumor surgery.SCAIF has the advantages of a short operation time, short intensive care period,less skin flap observation, and less nursing after operation, and can even be used as the first choice for repair of head and neck defects.Hanasono et al.10proposed SCAIF as the first-choice flap for hypopharyngeal reconstruction.Simultaneously,it appears to be a valid alternative for the reconstruction of many other head and neck defects.Spiegel11conducted a survey and found very low shoulder morbidity in patients after SCAIF procedure,with no significant functional impairment on the donor shoulder compared to the contralateral side.
Several perforator flaps have been used for the reconstruction of hypopharynx and upper esophageal defects,including the radial forearm flap and anterolateral thigh flap.Each flap type has advantages and disadvantages that should be carefully considered when selecting a flap for reconstruction.Radial forearm flaps offer larger surface areas and can be used to treat larger defects.However,the radial forearm flap may bethicker than the SCAIF flap and may require additional debulking procedures to achieve adequate contouring.The anterolateral thigh flap is another option for reconstruction in this area, as it offers reliable blood supply and relatively large surface area.However,the donor site may be more morbid than the other flap types,and careful consideration should be given to the patient’s overall health and comorbidities.
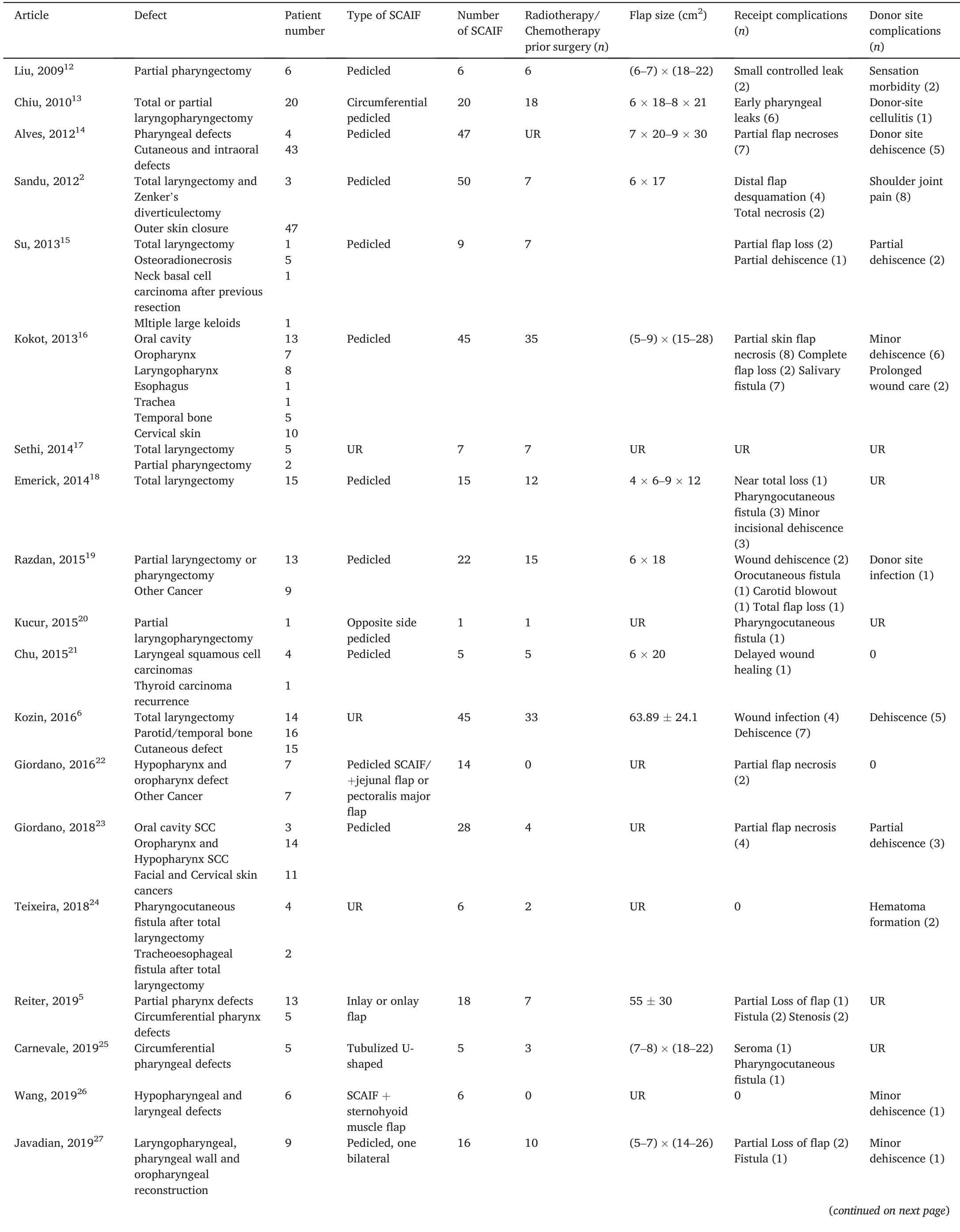
Table 1 Literature review of SCAIF involved in hypopharynx defects reconstruction.
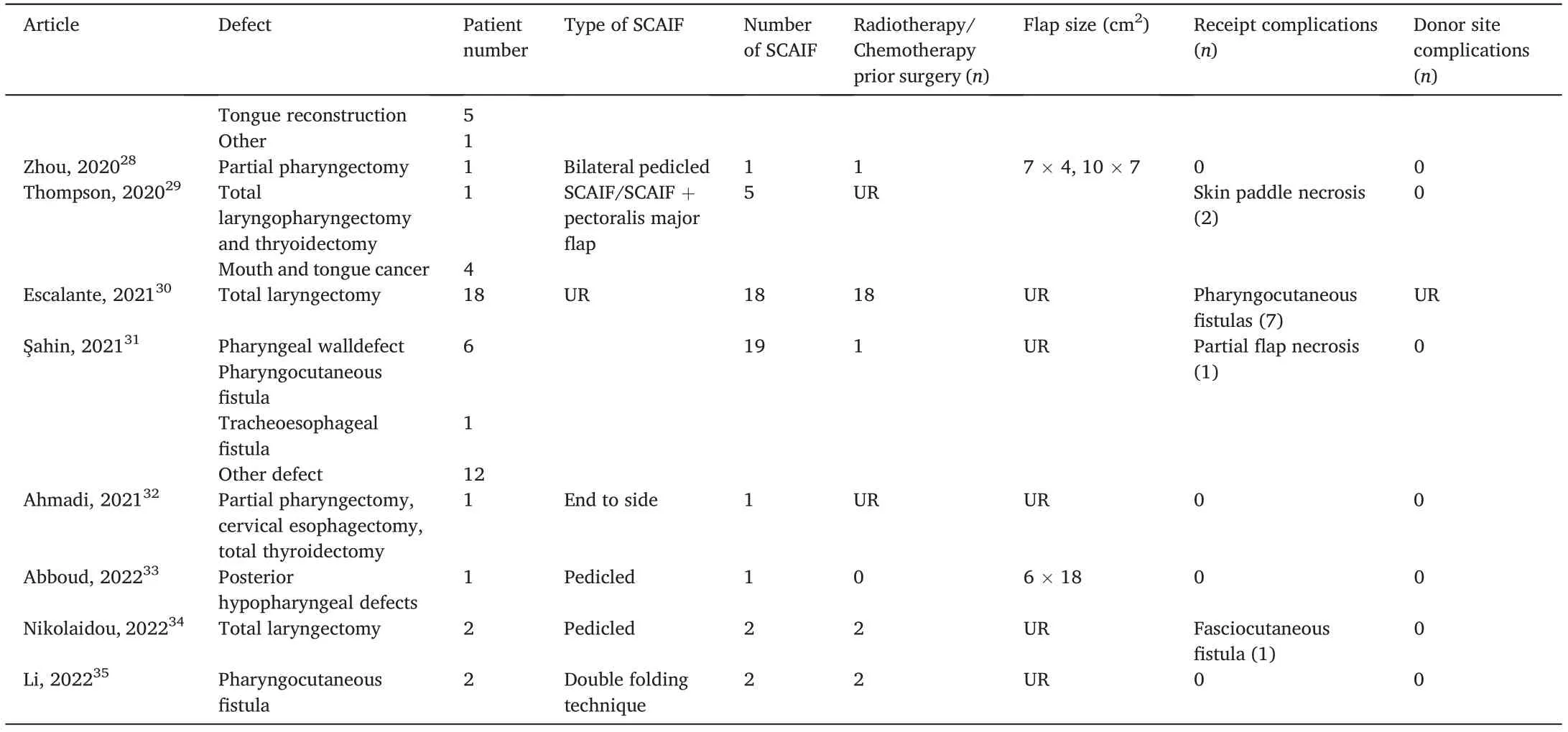
Table 1 (continued)
The present patient had hypopharyngeal and upper esophageal leakage as well as neck skin defects, which made one-stage reconstruction by SCAIF challenging.Fritz3developed a free double PTA flap for hypopharyngeal defects.The inside island of the PTA flap reconstructs the hypopharyngeal defects, and the external island of the PTA flap resurfaces the external neck skin defect.An external flap was used to monitor inner flap survival.The two flaps were completely separated to ensure hypopharyngeal movement.Therefore, we performed SCAIF on this patient.The most distal part C of the flap was used to repair the neck skin defect.Parts A and B at the proximal end of part C were used to repair the hypopharyngeal and upper esophageal defects.Thus, part C can monitor the survival of parts A and B.Once the microcirculation of the entire flap is obstructed, part C will show signs earlier than parts A and B,such as congestion and pallor of the flap or necrosis at the far end of the flap.
Complications of SCAIF have been described over the last decade(Table 1).The primary complication of SCAIF is partial or total skin necrosis, which may develop in the distal portion of the flap.In our review of 414 SCAIFs for reconstruction of neck and head defects, thirtyfive patients (8.45%) developed partial or total skin necrosis.In pharyngoesophageal reconstruction,the distal portion of the flap is critically important and is responsible for repairing the pharyngoesophageal defect.A flap length longer than 22 cm is significantly associated with distal tip necrosis,16,31whereas some authors have reported that the relationship between flap length and flap necrosis is not significant.Tip necrosis leads to leakage and fistula formation at the site of the anastomosis.The rate of leakage and fistula formation was 7.72%.In the present case,tip necrosis was seen in an area of 1.5 cm from the distal end of the flap and was managed conservatively with local wound care.Necrosis of the part B flap may be related to infection of the suture site between the flap and the hypopharyngeal mucosa rather than inadequate blood supply.If inadequate blood supply was the cause of necrosis, the distal end of the flap (part C) would have been affected first.To ensure adequate blood supply, handheld Doppler is necessary to identify the origin of the supraclavicular artery, and cautiously harvest the flap to avoid damaging the vascular pedicle.In the present patient, electronic laryngoscopy revealed minor necrosis of approximately 0.5 cm×1.0 cm in part B flap at the hypopharynx 12 days after the operation.Part A flap epithelium and upper esophageal epithelial mucosa were connected and healed.Thus, the nasogastric canal was inserted again to reduce the pressure during swallowing and avoid tearing of the nascent mucosa.Leakage at the part B flap lasted for 30 days and healed after conservative treatment.
Oropharyngeal and esophageal strictures are other major complications of reconstruction.The causes of stricture include narrow space of the recipient site, small diameter of the cervical esophagus, nonvascularized radiated tissue,scar formation, and improper bulk flap.To avoid stricture,it is important to remove non-vascularized tissue from the radiated neck wound and trim the flap to less than 1 cm, depending on the situation of the receiving area.Placement of a Montgomery salivary drainage tube can also prevent esophageal strictures caused by scar contracture at the anastomosis site.
Although SCAIF is a versatile and reliable option for head and neck reconstruction,it has several limitations that must be considered.These include the risk of partial or total necrosis in the distal portion of the flap,oropharyngeal and esophageal strictures due to the narrow recipient site space, small diameter of the cervical esophagus, and unsuitability for certain defects of the posterior pharyngeal wall or hypopharynx.Therefore, SCAIF should be used selectively in patients with small- to moderate-sized defects and an adequate vascular status.Careful preoperative evaluation and surgical planning are necessary to minimize complications and optimize patient outcomes.Alternative reconstructive options should also be evaluated based on the specific defect characteristics and patient conditions.
4.Conclusion
Our case report demonstrates the efficacy of SCAIF in reconstructing hypopharyngeal and upper esophageal defects with neck skin defects.SCAIF has several advantages including easy harvesting, definite vascular anatomy,and low cost.However, as we observed, it may also cause minor necrosis and leakage at the distal portion of the flap.Careful patient selection and surgical planning are essential to minimize complications.Alternative options should also be considered based on specific defect characteristics and patient condition.Nonetheless,SCAIF remains a versatile and reliable option for head and neck tumor surgery.
Ethics approval and consent to participate
This study received ethical approval from the Ethics Committee at the Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine (approval no.XHEC-D-2023-114).The patient provided written informed consent for this case report.
Consent for publication
The patient included in this study gave written informed consent to the publication of the data contained in this study.
Authors’ contributions
Ma X: Writing-Original draft.Sun X: Writing-Original draft.Shi Y:Data collection.Lv K: Writing-Review and editing.Chen W: Writing-Review and editing.
Declaration of competing interests
The authors declare that they have no competing interests.
 Chinese Journal of Plastic and Reconstructive Surgery2023年3期
Chinese Journal of Plastic and Reconstructive Surgery2023年3期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Application of a jigsaw puzzle flap based on free-style perforator to repair large scalp defects after tumor resection: A case series
- Eight-year follow-up on postoperative improvement protocol in extensive metoidioplasty transgenders: A case series
- Absolute ethanol embolization for treatment of peripheral arteriovenous malformations
- Efficacy of tibial transverse transport combined with platelet-rich plasma versus platelet-rich plasma alone in the treatment of diabetic foot ulcers: A meta-analysis
- Efficacy, effectiveness, and safety of combination laser and tranexamic acid treatment for melasma: A meta-analysis
- A randomized clinical trial assessing the efficacy of single and multiple intralesional collagenase injections for treating contracted scars
