Axial length shortening in myopic children with Stickler syndrome after repeated low-level red-light therapy
Xiang-Hua Tang, Meng-Ting Yu, Yin Hu, Ming-Guang He,2,3, Xiao Yang
1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Guangzhou 510060, Guangdong Province,China
2Centre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, Melbourne, Victoria 3004, Australia
3Ophthalmology, Department of Surgery, University of Melbourne, Melbourne, Victoria 3004, Australia
Abstract
● KEYWORDS: Stickler syndrome; axial length shortening;myopia; repeated low-level red-light therapy
INTRODUCTION
Stickler syndrome (STL), also called hereditary progressive arthro-ophthalmopathy, is a progressive connective tissue disorder induced by mutations in the collagen genes.This disease was first reported by Gunnar Stickler in 1965 and the clinical features include ocular abnormalities,craniofacial defects, hearing loss, and Skeletal disorder[1].The ocular abnormalities include myopia, abnormalities of the vitreous, retinal detachment, glaucoma, cataracts, and may even cause blindness[2].
STL was initially considered as a monogenic disorder.Mutations in various collagen genes were reported[3], including COL2A1, COL11A1, COL11A2[4], COL9A1[5], COL9A2[6],and COL9A3[7], which can cause Stickler syndrome type I(STL1) to Stickler syndrome type Ⅵ (STL6), respectively[7].Studies of the mechanism in STL suggest the mutations of collagen genes affect collagen production and lead to abnormalities in tissues and organs that contain corresponding collagens.
Currently, no standard diagnosis criteria for STL have been established.The diagnostic criteria on STL1 suggested by Roseet al[8]in 2005 has been generally used in all subgroups of STL studies but it has not been validated on large scales.To distinguish atypical STL and improve the rate of STL diagnosis and early treatment[9], Zhouet al[10]proposed new criteria for STL diagnosis in 2018, adding early-onset high myopia, posterior vitreous detachment/foveal hypoplasia,and hypermobility of the elbow joint as sore points to the diagnostic criteria.
Treatments for SLT mainly focus on prophylaxis and symptomatic management of its associated abnormalities.Regarding myopia in STL, it is reported that more than 80%of the patients showed moderate to severe myopia[11], and over80% of patients with mutations in COL2A1 or COL11A1 suffered from early-onset high myopia[10].Furthermore, it was suggested that myopia is a risk factor for retinal detachment in STL.However, few studies focused on myopia control in STL patients[11].The suitable treatment for myopia control in STL remains a mystery.

Table 1 Changes of cycloplegic SE refraction and AL before and after RLRL therapy
Repeated low-level red-light (RLRL) therapy is one of the new treatments for myopia control.Animal experiments have proved the efficiency of red light for myopia control in tree shrews[12-13]and rhesus monkeys[14]and proved the safety of RLRL in chicken[15].A prospective, multicenter, randomized clinical trial[16-17]has proved the efficacy and safety of RLRL therapy in myopia control in children.It remained unclear whether RLRL therapy could also retard axial elongation in myopic children with STL.
In this research, we described 3 patients with STL who underwent RLRL therapy, whose progression of myopic shift and ocular axial length (AL) elongation was successfully reduced and even reversed after RLRL therapy without side effects.
SUBJECTS AND METHODS
Ethical ApprovalEthical approval was obtained from the institutional review board of the Zhongshan Ophthalmic Center (No.2020KYPJ107).Written informed consents were provided by their guardians.
Three STL patients having high myopia or progressive myopia were investigated.The patients were comprehensively diagnosed with STL using 2 criteria reported in 2005[8]and 2018[10].Collagen mutations detected using targeted exon resequencing were confirmed in all these patients.
They received RLRL therapy throughout the follow-up period of 17, 3, and 6mo, respectively.The RLRL therapy was provided by a desktop light therapy device (Eyerising, Suzhou Xuanjia Optoelectronics Technology, Jiangsu Province, China),which is certified as a class IIa device by the China National Medical Products Administration (Register No.170808-01039).The device delivers steady 650±10 nm red light with a light power of 0.29 mW through a 4 mm pupil into the user’s eye.STL patients completed treatment twice a day with an interval of at least four hours, with each treatment lasting 3min at home, under the supervision of their parents.The treatment was automatically recorded and sent to the trial manager.The treatment compliance was calculated as previously reported[16].Evaluations were performed before RLRL was prescribed and at each follow-up visit, without cessation of the therapy.These included slit lamp examination, best-corrected visual acuity (BCVA) in decimal notation, intraocular pressure by non-contact applanation tonometry, cycloplegic subjective refraction, AL measurement (IOLMaster®700, Carl Zeiss Meditec AG, Jena, Germany), scanning laser ophthalmoscope(SLO, Daytona®, Optos, United Kingdom), and optical coherence tomography (OCT, VG200D, SVision Imaging,Ltd., China).Data on systemic disease history and family history were also collected.
RESULTS
Three STL patients (2 boys and 1 girl; ages ranged from 3 to 11y) were involved in this study.Spherical equivalent (SE) and AL before (change 1) and after (change 2) RLRL treatment are shown in Table 1 and Figure 1.Cases 1-3 were observed 10, 10, and 2mo respectively before RLRL therapy and were followed up for 17, 3, and 6mo respectively after initiation of RLRL therapy.No significant change of abnormalities was found using SLO and OCT and no side effects were observed in all patients during follow-up periods.
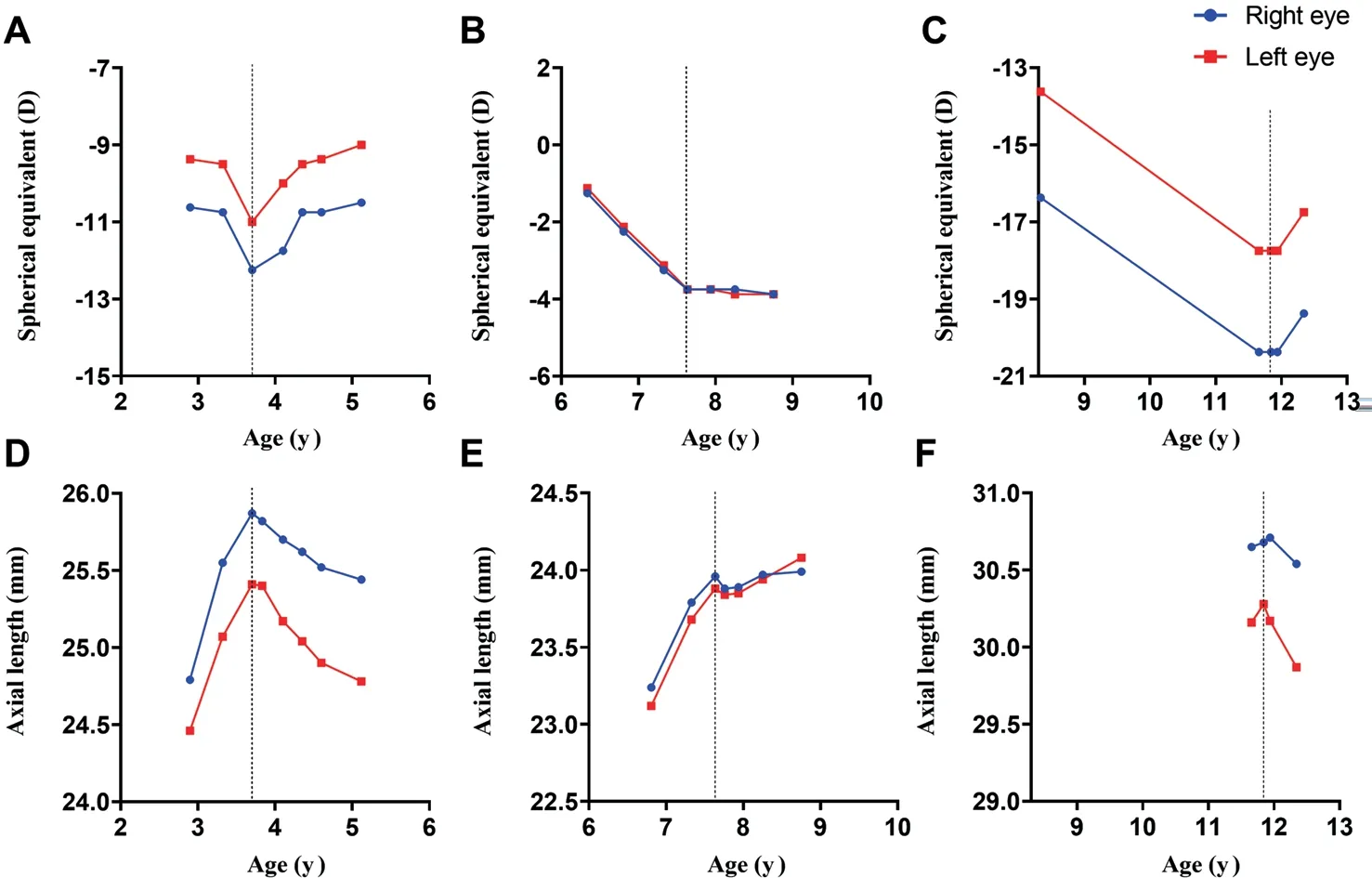
Figure 1 Time course of cycloplegic spherical equivalent refraction and ocular AL Cycloplegic SE refraction of 3 STL patients (Cases 1-3) were shown in A-C, and AL were shown in D-F, respectively.The dotted line showed the time when patients began repeated low-level red-light therapy.STL: Stickler syndrome; SE: Spherical equivalent; AL: Axial length.
Case 1A 3-year-old boy was referred to the Zhongshan Ophthalmic Center with progressive binocular high myopia.He was diagnosed as STL1 based on the clinical features and gene test results.Ten months after the prescription of single-vision spectacle lenses, his myopic SE and AL increased in both eyes.His BCVA in both eyes was 0.4 which didn’t reach the lower limit of normal children[18].Though with rapid myopia progression, he was too young to receive orthokeratology (OK)lens treatment.Therefore, we prescribed him RLRL therapy after excluding fundus abnormalities through SLO and OCT.After RLRL therapy for 17mo, his myopic refractive error decreased and AL shortened in both eyes.Choroidal thickness increased by 24.45 and 39.19 μm in the right and left eyes,respectively.The BCVA of both eyes increased from 0.4 to 0.7.During the observation period, the corneal curvature in the right eye changed from 44.26 to 44.00 D and in the left eye from 44.14 to 44.54 D, while the anterior chamber depth in the right eye decreased from 3.56 to 3.51 mm and in the left eye from 3.52 to 3.48 mm.
Case 2A 7-year-old boy had been diagnosed as STL1 with progressive binocular moderate myopia.His myopia progressed 6mo after the initial visit when single vision spectacle lenses were prescribed (myopic SE increased by 1.00 D in both eyes and AL increased by 0.55 mm in the right eye and 0.56 mm in the left eye).Defocus incorporate multiple segments spectacle lenses were then prescribed, but his myopia continued to progress in the following 4mo (myopic SE increasing by -0.50 D in the right eye and -0.63 D in the left eye; AL increased by 0.17 mm in the right eye and 0.20 mm in the left eye respectively).Therefore, we prescribed RLRL therapy to him.
After RLRL treatment for 3mo, his progression of myopic shift and AL elongation were successfully reduced.Choroidal thickness increased by 34 μm in the right eye and 26 μm in the left.His BCVA in both eyes remained at 1.0 during the followup period.The corneal curvature in the right eye changed from 45.04 to 45.11 D and in the left eye from 45.25 to 45.29 D during the observation period.
Case 3An 11-year-old girl with binocular high myopia and long AL had been diagnosed with Stickler syndrome type Ⅱ(STL2).The myopic SE in the right increased from 16.38 to 20.38 D and that in the left eye increased from 13.63 to 17.75 D since she was 8 years old, according to the medical records.AL in her left eye continued to increase during the following 2mo.Regarding the high myopia and axial elongation in the left eye,RLRL therapy was prescribed.
After RLRL treatment for 6mo, the AL of both eyes shortened.Choroidal thickness decreased by 11.00 μm in the right eye and increased by 11.00 μm in the left eye respectively.The BCVA of her right eye remained 0.7 and that of her left eye increased from 0.7 to 1.0.The corneal curvature in the right eye altered from 43.85 to 43.89 D and in the left eye from 43.92 to 44.37 D,whereas the anterior chamber depth in the right eye fell from 3.79 to 3.77 mm and in the left eye from 3.78 to 3.73 mm over the observation period.
DISCUSSION
In this research, we reported encouraging clinical outcomes of 3 cases of STL with progressive myopia after using RLRL therapy.They all demonstrated reduced progression of myopic shift and AL elongation without side effects, and at least two of them showed myopia reversion, axial shortening, and choroid thickening.
Regarding myopia secondary to STL, previous studies indicated over 80% of patients with mutations in COL2A1 or COL11A1 suffered from early-onset high myopia[10].Some studies suggested the myopia of STL is generally congenital and non-progressive[2,19-20]but some also described STL patients suffering from progressive myopia[21-22].Furthermore, Boysenet al[11]analyzed 37 articles with 2324 STL patients and suggested that myopia is a risk factor for retinal detachment.However, most studies just simply reported the myopia prevalence[10-11]of STL without describing the refraction development of STL.Therefore, more attention should be taken to myopia control in this population.
Current strategies for myopia control includes more time outdoors, OK lens, multisegment spectacle lenses, multifocal design contact lenses, and low-dose atropine.However, limited approaches for myopia control are available for patients with STLs due to their young age, high diopter, and low vision.All the current refractive strategies for myopia control, including OK lens, multisegment spectacle lenses, and multifocal design contact lenses, are based on the peripheral defocus theory.These have a risk of hindering visual development for children who are undergoing the visual experience-dependent critical period of vision.For the OK lens, the total higher order aberration, increases after wearing the OK lens[23]which reduces retinal image quality[24].For low-dose atropine, besides the side effects of reducing the amplitude of accommodation and slight mydriasis[25], it dilates the pupil[26]and increases higher order aberration[27]and reduction of visual quality.In this research, RLRL therapy, an emerging method to inhibit myopia progression, was adopted for myopia control in patients with STLs in this study.
It is generally thought that myopia is an irreversible disease.However, in this research, we described 3 cases of STL with AL shortening and myopia reversed after RLRL therapy.The AL of 5 eyes from 3 cases shortened by over 0.05 mm after RLRL therapy, exceeding the measurement error of optical low-coherence interferometry[28].We also measured choroid thickness of the subjects.The values of AL shortening of 5 eyes were 0.43, 0.63, 0.07, 0.14, and 0.41 mm while the corresponding values of choroid thickening were 24.45, 39.19,34.00, -11.00, 11.00 μm.The shortening of AL could not be completely explained by the thickening of choroid.The changes of corneal curvature were -0.26, 0.40, 0.07, 0.04, and 0.45 D, which could not completely explain the reversion of refraction.
Clinical trials about the effect of RLRL therapy on normal children also reported the phenomenon of AL shortening.A multicenter randomized controlled trial in 2021 found 70.1%of myopic children achieved AL shortening over 0.05 mm after RLRL therapy at 1-month follow-up[16]and later they found nearly a quarter of children had AL shortening after 12mo and the averaged shortening is -0.156 mm in RLRL group[29-30].Two other studies similarly found the AL of myopic children decreased by about 0.06 mm after 6-month or 9-month RLRL therapy respectively[31-32].AL shortening of all these three trials couldn’t be completely explained by the thickening of choroid.In our study, we found a similar phenomenon of AL shortening in children with STL after RLRL therapy compared with normal children in previous studies.
AL shortening has also been reported in a handful of studies of other myopia control strategies.An OK-lens study found shortening of AL in the early phase due to the OK-induced central corneal thinning[33-34].As for atropine, ATOM1 found that high-dose (1%) atropine shortened the AL by about -0.14 mm in the first year.Since high-dose atropine led to cycloplegia and photophobia, it was seldom used[35-36].Two classic lowdose atropine studies (ATOM2, LAMP)[37-38]had not found the shortening of AL in the 0.01% dose atropine group.The AL shortening has been found neither in multisegment spectacle lenses[39]nor in multifocal design contact lenses[40].
The mechanism of refraction regress and AL shortening is not clear.In this study, thickened choroid and changes in corneal curvature could not fully explain the changes.Scleral collagen remodeling would potentially explain the change but needs future verification.
The reason why BCVA increased in Cases 1 and 3 is not clear,which age effect might partly explain so do RLRL therapy.Red light flicker has been used to treat amblyopia since the 20thcentury, and it has been shown to improve the vision of half of the patients with amblyopia by 0.2 logMAR[41-42], though, its underlying mechanisms were still unexplained.Therefore, the improvement of BCVA in this study might benefit from age effect as well as the RLRL therapy.It is necessary to conduct further research to better understand the relationship between them.
The present study is limited by the lack of long-term followup, although some studies have assessed the two-year efficacy and safety of RLRL therapy for myopia control in children[17]without ocular conditions other than refractive errors.The current short-term study provides preliminary baseline data for further studies.Besides, due to the limited sample size, the 3 cases mentioned in this study might not completely represent all myopic children with STL.
In this research, 3 patients with STL underwent RLRL therapy and reduced myopic shift and AL elongation successfully without side effects observed during the follow-up period,and even some of whom showed AL shortening and refractive reversion.
ACKNOWLEDGEMENTS
Conflicts of Interest: Tang XH,None;Yu MT,None;Hu Y,None;He MGis inventor for the RLRL technology mentioned in the study patented as “A method to increase retinal blood flow and metabolism” (CN201910490186.6) and director in Eyerising Ltd.and Eyerising International Pty Ltd.;Yang X,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Visual resolution under photopic and mesopic conditions in patients with Sjögren's syndrome
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Three-dimensional bioprinting in ophthalmic care
- Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
