Three-dimensional bioprinting in ophthalmic care
Saleha Al-Atawi
Al-baha University, Applied Medical Science, Al-Aqiaq,AlBaha 4781, Saudi Arabia
Abstract
● KEYWORDS: ophthalmologic bioprinting; bioprinting;bioinks; ocular bioprinting; 3D bioprinting
INTRODUCTION
Additive manufacturing or three-dimensional (3D)printing refers to a range of methods that employ virtual 3D computer-aided design files encoded into stereolithography(using Standard Triangle Language and G-Code) to create 3D/physical structures by depositing layer-by-layer (i.e., fused deposition modelling) within micrometre precision[1-6].Other techniques include selective laser sintering and powder bedinkjet[7-9].Bioprinting involves the deposition of layers of living differentiated cells, crosslinkers, biomaterials/structural components, functional elements and growth factors onto synthetic scaffolds to form 3D living structures containing basic vascular structures capable of generating additional tissues/organs with natural tissue/organ characteristics effectively supporting adhesion and proliferation as well as differentiation of cells)[3].The use of autologous materials and advancements in biocompatible materials have substantially minimised rejection and irritation risk.While 3D printing has found substantial application in other medical fields, it’s only recently finding use in ophthalmology[6].This is in spite the easy accessibility of the inner eye, the eye’s immune privilege,and the availability of multiple diagnostic tools[3].This is an isolated, but complex organ with diverse specifically organised tissue structures that embrace both anatomically simple multilayer structures like the cornea and complex structures enclosing the central nervous system.
SEARCH AND SELECTION CRITERIA
Ethical ApprovalThe researcher sought approval from the Institutional Review Board at Al Baha University (No.1443-21-43110073).
Using PubMed, ProQuest, Scopus, and Google Scholar,combinations of the following phases and Boolean operators were searched 3D printing OR 3D printing OR additive manufacturing OR bioprinting AND ophthalmology OR eye OR ocular.The searches were subsequently to include eye anatomies or diseases, including retina, cornea, iris, lens,keratoplasty, cataract, and glaucoma.The results were, where possible, filtered to include only English language, peerreviewed articles published 2011-2022.Searches were mostly restricted to abstracts, titles, and key words (Figure 1).
PRINTING METHODS
The current 3D bioprinting technologies fall into four main categories: inkjet, micro-extrusion, stereolithography, and laserassisted[6,9-10].The inkjet technique was the earliest bioprinting technique[4,6].Heating units at the inkjet nozzles form bubbles that expand to generate a driving force that squeezes out the bio-ink[6].It works by way of Fused deposition modelling,comprising a thermoplastic polymer filament that is heated into a semi-liquid state before being extruded onto a panel to generate layers[6,9,11].By controlling nozzle movement within a space, it’s possible to order the extruded droplets to create a designed structure[12].It offers single cell positioning by spraying nano-sized cell droplets similar to two-dimensional printing.The printing quality is affected by parameters such as layer thickness and width, printing direction, and air gaps in filament layers[6].This technique is cost effective, simple and fast, but achieves low resolution and poor mechanical properties[3,12-15].Thermoplastic materials are also hard to access[14].Its high cell deposition throughput can still attain 80%-90% cell viability and resolution of 0.5-40 µm[6].However, microelectromechanical systems result in mild nozzle deformations that render it difficult to extrude highly viscose or dense materials[14].
(Micro)extrusion printing involved pressurized deposition of biomaterials and hydrogels, by way of either mechanical piston/screw or pneumatic dispensing systems[16-17].Printed structures are chemically or physically fixed[9].It’s a medium cost technique that permits a broader choice of biomaterials,including highly dense materials through micro nozzles [and viscosities of 30 millipascal-seconds (mPa/s) to more than 6107 mPa/s] and can attain 40%-98% cell visibility[9,18].It also allows high throughput, medium single-cell printing, higher gelation speed, and moderate resolution (200 µm)[6,16].Laserassisted printing uses laser stimulation to induce light or heat evaporation and deposition[19].It accommodates droplets of up to 107 mPa/s and offers low mechanical/structural integrity, but delivers more than 95% cell visibility and high resolution[16,20].Examples of applications of laser jet printing in ophthalmic tissue printing are listed in studies[21-24](Figure 2).
Digital light processing (DLP) differs from laser-based stereolithography as it projects ultraviolet light from a digital projector to create a single image of a layer across a whole resin at once[10,25-26].It photopolymerizes liquid photo-initiated curable ink layer after layer[26], effectively offering comparably superior fabrication speed, tissue integrity and resolution[10,27-29].Lastly, stereolithography involves polymerisation of lightsensitive polymers by finely controlled light projected from digital nano-mirrors[29].It offers low-cost but high quality(resolution of 100 µm), speed, and 90% cell viability[30-31].It’s unlimited by viscosity (1-300 mPa/s)[32], but its use of ultraviolet light has been shown to damage cell DNA[30-31].It similarly cannot print multi-cell layers and its curing process results in further cell damage[3,29-31].Visible light stereolithography averts this limitation[29].Wanget al[33]for example, used a beam projector and blended gelatin methacrylate (GelMA),poly(ethylene glycol) diacrylate (PEGDA), and erosin Y-based photo initiator.These resulted non-toxic effect on the cells during printing and curin (Table 1)[4,12,24,30,34-36].
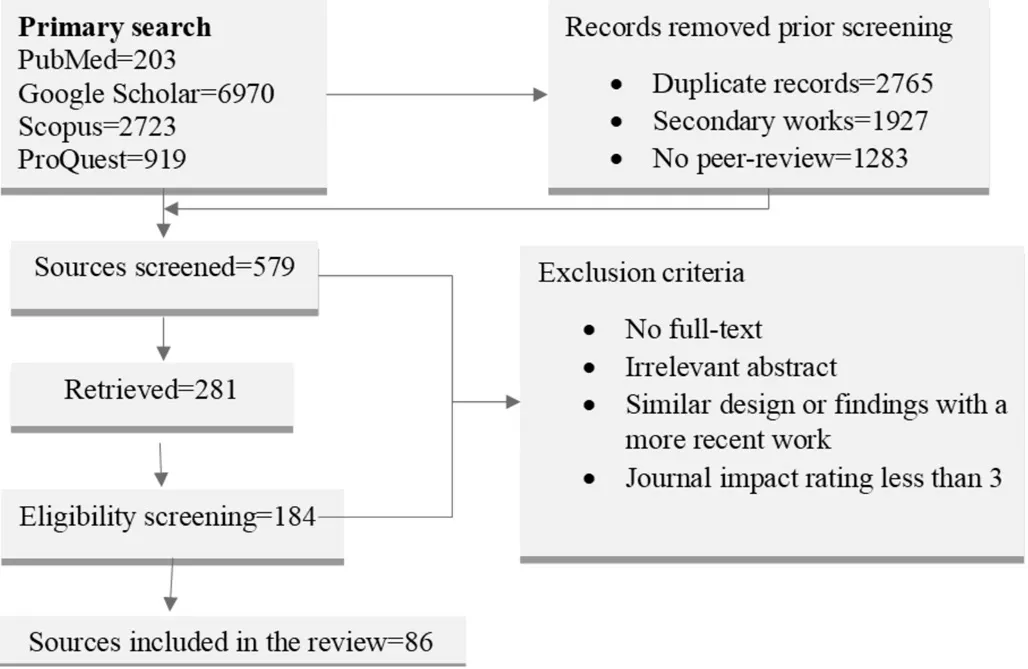
Figure 1 Search and selection criteria.

Figure 2 Printing techniques[24].
BIOINKS
Tissue engineering hinges in the development of bioinks with not just the right rheological properties, but also with mechanical strength necessary to withstand sheer extrusion stress and preserve the cell viability, ensure nutrient/oxygen diffusion and adequate transparency[13,18,34].Different approaches have been tried successfully, but the challenge remains creating a multi-layered and replicative structure[18].Thus far, stromal equivalents have been created by including keratocytes in type I collagen bioinks with multiple combinations of alginate, gelatin, methacrylate, and agarose[4,13,35].GelMA hydrogel bioinks have shown substantial promise[19,29,33,36], even though its brittleness hinders its surgical handling[26].Kilic Bektas and Hasirci[36]used GelMA hydrogelsto produce a stroma equivalent by optimising printing conditions to achieve 98% cell viability in 21d and 80%transparency compared to native tissue.The resulting tissue exhibited acceptable mechanical properties that doubled during the incubation period to close to the native tissue.Collagens type I/V and proteoglycan expression in keratocytes points to the maintenance of phenotype in hydrogels.
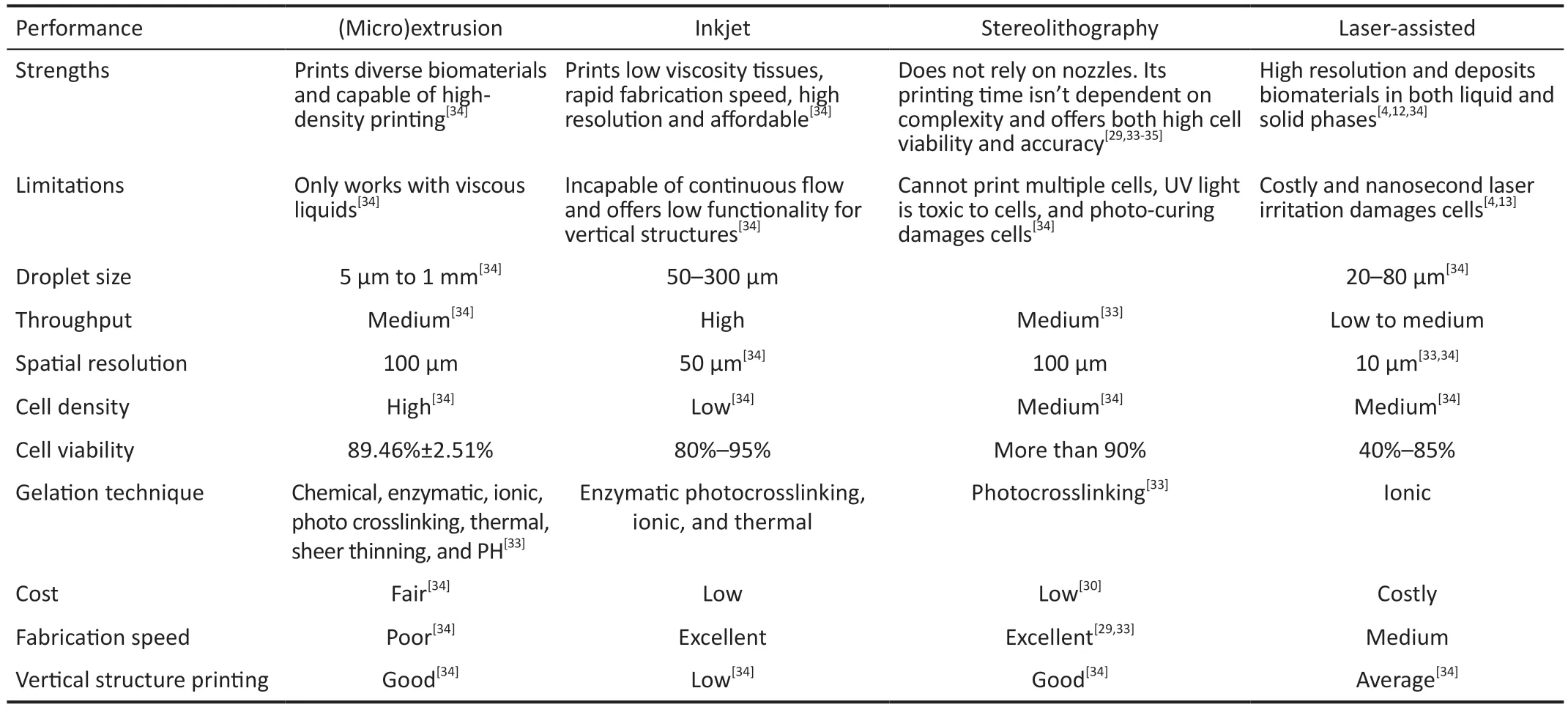
Table 1 The current 3D bioprinting technologies
Wanget al[33]developed visible-light-crosslinkable and cellattachable bioinks based on photocrosslinkable GelMA with eosin Y photoinitiation for 3D bioprinting.GelMA has high cytocompatibility, economical, elicits lower immune response,and can form scaffolds with both simple and complex geometry.The study showed microscale bioprinting with visible light laser diode in under 10s with higher than 90%cell viability[33].The study found that compressive Young’s modulus as well as pore size are positively affected by eosin Y concentration, while cell viability and mass swelling ratio are inversely affected[6,33].
Mahdaviet al[29]used visible light-based stereolithography technique and two concentrations of GelMA macromer(12.5% and 7.5%) to print stromal tissue and investigate gene/protein expression, and cell proliferation.The 12.55 GelMA scaffold concentration was stiffer, easier to handle and the scaffolds had both optical transmittance and water content similar to native tissues.This scaffold did not only exhibit superior cytocompatibility of 81.9% and 156% at days 1 and 7, respectfully, they also exhibited elongated stromal cells on day 7, consistent with growth, attachment and integration.The expression of collagen type I, Lumigan and keratan sulphate improved over time[29].
CORNEA
Bioengineering attempts at developing corneal scaffolds founded on amniotic membrane, collagen, decellularized cornea, hyaluronate, GelMA, alginate, or synthetic, poly(2-hydroxyethyl methacrylate) polymers have yielded tissues that exhibited the same attributes as the natural cornea[6,28,37-38].At present, the need for transplantable substitutes is high due to the shortage of full structure corneain vitromodels for testing drugs and toxicological studies[6,27].Corneas are avascular and innervated tissues comprising thick collagenous structures with three tightly parked cellular layers and two interface layers[6,39].Keratoplasty is a critical treatment for severe corneal diseases,but low survival rates of explanted tissues, keratocytefibroblast transformation, immune rejection, high cost, lack of corneal banks/donors, and scarce accessibility make it cumbersome[6,26-27,29].Bioprinting holds promise in fabricating highly functional acellular membranes for cell therapy and achieving near-natural corneal transparency, biomechanical properties, and curvature[6,12,40].Empirical studies into 3D corneal tissue engineering, which have primarily focused on the stroma[4,36], epithelium[6,41], retina[42], and conjunctiva[12,27],show bioprinting to be feasible albeit without any evidence of clinical translation[4].
Perhaps one of the greatest hindrances to developing clinically implantable corneal bioequivalent lies in bioengineering stromal tissues[40].This is not least because, unlike the epithelium and endothelium that are cellular and backed by basement membranes, the stromal tissue is highly organised,keratocyte-filled collagenous connective (Figure 3).

Figure 3 Corneal structure[6].
It’s critical for the cornea’s mechanical strength, refraction,and transparency[43], and there is very little empirical evidence of bioengineered biomimetic corneal stroma[44].Studies into FDA-approved polymers like hydroxymethylacrylate and poly(lactide-co-glycolide have not shown successful translation beyondin-vitro[45-48], with rabbit models showing severe inflammation, ulceration, and haze[45].Isaacsonet al[4]demonstrated that keratocyte-loaded corneal stromal equivalent is ches3D-printable using low viscosity bioinks at high resolutions.The study used rotational Scheimpflug camera to develop models specific to each patient and used collagen-based bio-ink with encapsulated corneal keratocytes to print stroma.The study reproduced corneal curvature, with near-natural transparency and biomechanics of the scaffolds.The keratocytes showed 90% and 83% cell viability at days 1 and 7 after printing, respectfully, but the cells in bio-printed scaffolds were elongated and exhibited dendritic morphology,resulting in low protein expression and metabolic activity.
Kimet al[49]built a biomimetic corneal stromal tissue with decellularized extracellular matrix and cells.The study used rheometric expansion system to evaluate rheological properties of 0.5% to 2% of decellularized extracellular matrix gels,which analysis showed shear thinning behaviours in gels of different concentration in 1-1000/s shear stress range.On their part, Kutlehriaet al[50]3D-printed corneal stroma using combined sodium alginate, type I collagen and gelatin type B.The rheological evaluation established that at printing temperatures higher than 37 degrees Celsius, the gelatin melted at and the bioink storage modulus diminished, while temperatures lower than 20 degrees Celsius necessitated higher extrusion pressure.
Chenet al[44]used support primary human stromal cells and collagen fibrils to develop an orthogonally-oriented bioprinted corneal stroma model.The study offered the first published demonstration of transparent, nutrient-permeable pure collagen-based 3D corneal stroma model developed from pure electro-compacted collagen.Collagen fibrils of 3D corneal stromal model are aligned and arranged orthogonally to mimic native corneal stroma.Such alignment correlates with the direction of electrical current applied for electro-compaction and influences human stromal cells orientation.The 3D corneal stromal model constructs bear out a corneal keratocyte phenotype, which is a critical requirement in modelling healthy corneal stroma.
Kilic Bektasand Hasirci[36]found that GelMA hydrogels 3D-printed with keratocytes are capable of mimicking physical and biological properties of native stroma, including cell viability, transparency (~5% at ultraviolet B wavelength;85% at 700 nm for an eight-year-old cornea), and mechanical strength.Using a blend of GelMA and long-chain PEGDA with a DLP printing technology, Heet al[26]proposed a 3D-printed biomimetic epithelium/stroma bilayer implant.Bioprinted PEGDA-GelMA hydrogels supported cell adhesion,proliferation and migration, while at once achieving high light transmittance, nutrient/oxygen permeation, appropriate inflammation degree, and an acceptable rate of degradation.It is possible to print a bi-layer corneal scaffold comprising rabbit epithelial cells-packed epithelial layer and a rabbit adipose-derived mesenchymal stem cells-packed orthogonal aligned fibrous stromal layer.The printed tissue demonstrated robust surgical handling capacity and high fidelity.The postoperative outcome from applying the resulting corneal scaffold was applied in rabbit keratoplasty demonstrated efficient sealing of defects in the cornea, stromal regeneration, and reepithelialization[26].Further, Heet al[26]show that bioprinted corneal scaffold and accurately located cells within the epithelial and stromal layer offer an excellent biological and topographical microenvironment for regenerating the cornea.At present, engineered corneal tissues that are widely accepted for routine clinical treatment are unavailable[12], but recentin vitrostudies have demonstrated comparably higher biocompatibility and regenerative capabilities of bioengineered hydrogels than traditional tissue engineering techniques[14].
EPITHELIUM AND ENDOTHELIUM
The human amniotic membrane is still employed as a biological matrix on account of the growth factor content,low immunogenicity, antifibrotic and antimicrobial/antiviral properties[50-51].It, however, presents with a risk of disease transmission, varied growth factor content and demanding processing[52].Synthetic polymers offer greater purity because their chemical composition is knowable, along with their physical properties, degradation times and structure[50-51].Studies[22-23,53]that attempted to develop epithelium and endothelium cells using bioprinting.
Using cultured human corneal endothelial cells, Kimet al[23]fabricated an endothelium tissue that survivedin vivoand showed that engineering human corneal endothelial cells to over-express RNase 5 could be an option to create higher graft cellularity as well as improve the function of transplanted grafts.On their part, Sorkioet al[22]developed a lamellar corneal stroma and a stratified corneal epithelium using a lesser bioprinter with limbal epithelial stem cells and human adipose tissue derived stem cells, before printing epithelial and stromal tissues.The same were analysed for cell viability, proliferation,microstructure, and key protein expression, before subsequent implantation in porcine corneal organ cultures.The printed epithelial stem cells created a stratified epithelium that expressed CK3 and progenitor markers, while stromal human adipose tissue derived stem cells mimicked native horizontal structure with positive collagen I labelling.Porcine cultures successfully attached to host tissues and human adipose tissue derived stem cells migrated from the printout.This study was first to show feasibility of 3D laser-assisted bioprinting for epithelial tissue applications using stem cells and successful development of stratified 3D bioprinted tissue that mimicked native corneal tissue structure[22].
CONJUNCTIVA
While human conjunctival stem cells (hCjSCs) are bipotent stem cells that may give rise to conjunctival keratocytes and conjunctival goblet cells, their applications in tissue engineering have been hindered by little knowledge about their microenvironment and viablein vitroexpansion techniques[27].In a first-reported 3Din vitrodisease model for pterygium that integrated 3D bioprinting and stem cell technology,Zhonget al[27]explored DLP-based 3D bioprinting platform and hCjSCs to create a 3D multicellularin vitropterygium model.The study obtained hCjSCs from donor tissues before expanding them using a feeder-free culture system and expanded primary hCjSCs without affecting their stemness,homogeneity, and differentiation potency[27].
The DLP-based printing technique capably fabricated hydrogel scaffolds and supported viability as well as biological integrity of encapsulated hCjSCs.The resulting pterygium model comprised of hCjSCs, vascular cells and immune cells to recapitulate the disease’s microenvironment.A transcriptome analysis (using RNA sequencing) showed a distinct profile that was consistent with inflammation response, epithelial mesenchymal transition and angiogenesis in the bio-printed model.Further, the pterygium signatures as well as the disease relevance of the resulting model were validated using public RNA sequencing data drawn from patient pterygium tissues[27].Despite the need for hCjSCs, there are no publicly reported protocols for developing hCjSCs models.Thus, this study’s protocols and findings could be combined with clinical cytology for clinical studies, particularly given the DLP-based 3D printing potential for producing clinically translatable tissues[10].Compared to 2D cell monolayer, 3D printed models with control geometry, extracellular matrix composition,and cell distribution was found to be more scalable and reproducible as well as better able of mimicking physiological/pathological microenvironment[9,28,49].The model developed in this study may potentially support the development of highthroughput drug screening[28].
RETINA
Retinal dystrophies like retinitis pigmentosa, age-related degeneration, and Stargardt disease currently lack effective therapies and for which bioprinting holds immense promise[7,54].The retinal architecture does not only vary greatly with more than 60 different cell types, varied diseases affect different components that have different bioengineering needs[7].Predictably, there is no evidence that 3D bioprinting can provide a safe and functional retinal tissue for clinical implantation[3,6], particularly as pertains developing an adequate amount of cells with sufficient post-printing viability,phenotype, vascularisation, and functionality[21,55-56].
Lorberet al[56]successfully created viable retinal ganglia cells and glia using a piezoelectric inkjet bioprinter, but the resulting tissue couldn’t replicate the complex cellular structure in multiple layers.Some other studies[6,8,21,55]demonstrated that mice glial and ganglion cells are printable onto an electrospun scaffold of cells with neurotrophic factor drawn from the brain and ciliary neurotrophic factor with retained electrophysiologic function and radially aligned growing axons[6,21,50].It’s also possible to print scaffolds to support the proliferation of infused retinal cells[6,57-58].Models with photoreceptor layers and retinal pigment epithelium may be printed using hydrogels and supporting extracellular matrix[6,57-58].Masaeli and Marquette[8]suggest a hydrogel-free alternative that uses dense cell suspensions that secrete own supporting matrix.
Using electrohydrodynamic jet printing, Liuet al[59]replicated scaffolds resembling Bruch’s membrane by bolstering retinal pigment epithelium cells to mature into polarized and functioning single-layered epithelium that could potentially comprisein vitromodels to study retinal diseases/treatments.Further, 3D can be used to improve existing retinal imaging techniques and visualisation of optical coherence tomography (OCT)[3].According to Sommer and Blumenthal[3]ophthalmologists are currently limited to two-dimensional retinal imagining.3D models can offer finer details for patients and physicians[3,6,51,60-62].Similarly, 3D retinal models can be used to train ophthalmologists in order to improve the trainees’perspective by triangulating 3D models with two-dimensional images[3,62].Pugalendhiet al[63]printed eye models that closely assimilates natural eyes by focusing on the optimum viewing area, before the eye model was designed and re-engineered for retina laser was fabricated using 3D bioprinting.The reengineered model increased the viewing angle and viewing area by 6.14% and 16.66%, respectfully.
Choiet al[62]on the other hand, showed that 3D bioprinted models offer accurate pre-operative data in respect to both the surface and shape of the epiretinal membrane (including vitreoretinal traction and adhesion points).The customisability of such models to each patient is helpful in determining beginning points for epiretinal membrane peeling[3,13,62].Malocaet al[58]bioprinted OCT angiography scans to attain higher resolution and speckle-less visualisation of choroidal and retinal vasculature as well as choroidal tumours.By processing OCT angiography data, the study obtained printable versions of the model to depict a 3D arrangement if vasculature of the inner retinal surface with branches linking to the inner retinal vascular networks[58].Other studies[7-8,29,42,56,64], printed retinal pigment epithelium and photoreceptors, using, among others, human retinoblastoma cell line, human retinal pigment epithelia cell line drawn from normal eyes of a 19-year-old,and human foetal retinal progenitor cells.
OCULAR DRUG TESTING AND DELIVERY
While animal models are routinely used to test drugs,physiological, genetic, and pharmacokinetic differences reduce reliability of such models[65-66].Even animals that share genes with humans like mice have different genetic regulation mechanisms[10].Conventional ocular drug delivery continues to struggle with the nearly impregnable barriers, particularly to the posterior region[67].Topical drug delivery remains the primary means for the vast majority of treatments, despite its substantial inefficiency[5,10,39].Other than multiple successful studies in developing kidney and liver models owing to their central role in drug targeting, absorption, distribution, plasma protein binding, and elimination, particularly in drug testing[68]a promising number of works more specific to the eye are increasing.
Melochhiet al[65]and Samykanoet al[69]found that 3D-mold technology is a comparably effective alternative to injection moulding technology for delivering drugs with formulations comprising hydrophilic polymers, polyvinlpyrrolidone polymers and triethylcitrate plasticizer, hydroxypropyl cellulose, povidone, graft polymers were used as polymers,and hydroxypropylmethylcellulose.Further, 90% of drugs dissolved rapidly under 10 percent applied load[69].Fused deposition modelling has particularly shown promise for its compatibility with many polymer-based hybrids for, among others, improving drug delivery, modifying release kinetics,and protecting thermolabile drugs[5,70-73].This is despite the low dissolution speed of printouts compared to compression-based tablets[74].To enhance the dissolution rate of poorly soluble medications, Parulskiet al[70]and Omariet al[72]employed hotmelt extrusion with fused deposition modelling.Parulskiet al[70]printed four formulations of Affinisol 15LV and Kollidon VA64, with amounts of itraconazole 25% in forms of 20%,50%, and 80% infill densities.The bioprinted formulations were shown to enhance drug release compared to crystalline drug formulations.The infill density as well as the polymer composition influenced by the rate of dissolution.On their part Omaret al[72]developed 10 formulations that were fully soluble in polymeric carriers and achieved in vitro release rate of up to 97% in 30min.
Like Parulskiet al[70]and Omariet al[72], Kempinet al[73]tried five water-soluble polymers (PEG 6000, PVP K12, PEG 20 000, Kollidon®VA64 and poloxamer 407) to develop immediate release tablets of a thermosensitive drug.While introducing disintegrants in printed tablets showed no improvement on drug release as fused deposition modeling inhibits water imbibition and swelling[73-74], reducing the infill percentage by half in the PVP K12 tablet, cutting dissolution time by three minutes[73,75].Using gelatin methacryloly as a base, as well as conjunctival epithelial cells and antibiotics as bio-inks, Parket al[75]developed a drug delivery system for treating dry eye.The method could control the rate of degradation, effectively easing treatment, protecting the cornea, and regenerating the epithelium.
EDUCATION
The available evidence supports the use of 3D printing to supplement anatomical learning/instruction in under/postgraduate education and even in pre-operative planning practice.Other than the fact that donor tissues and cadavers are limited due to social stigma, cost, and availability,ocular anatomical complexity, the difficulty involved in conceptualising it externally, and variations from patient to patient renders it difficult to train students[12].3D orbital modelling drawn from cadaver prosections and/or patient magnetic resonance imaging and computerized tomography scans have been demonstrated in some studies[76-78], for example, used patient computerized tomography scans to generate 3D orbital models that achieved more anatomical representations and realistic soft tissue attributes for orbital surgery.
Creating realistic, comfortable and accurate ocular and orbital prostheses currently require highly skilled and experienced prosthetists.3D modelling permits the introduction of anatomical variations to overcome declining cadaveric dissections as well as the limitations of idealised atlases[76,79].Modelling also adds an additional dimension to pathology instruction[6,36].Obtaining shareable data from volunteers and pre-operative models between institutions/museums serve to provide students with access to rare conditions[76,80].3D models offer multi-sensory anatomy learning experience.Experimental research points to the potential of 3D models replacing cadaveric dissection and attaining at least comparable learning outcomes, particularly when integrated with patient-specific models[79-83].Surgeons can undergo realistic simulations of individualised operative procedures to better plan operations, create realistic scenarios, and predict intra-operative complications[80].
For pre-operative preparations, Shyuet al[83]used an orbital volume calculation technique based on 3D volume renderingassisted region of interest to ascertain the normal orbital volume in patients after re-orienting to the Frankfurt plane.The computations were acceptably accurate for unilateral orbital reconstructions[83].Other studies[84-85]bioprinted silicone eye models that simulated diverse strabismus surgeries.The models were shown to have comparably better anatomical accuracy, with sclera and conjunctiva that mimicked native tissues[84-85].Fameryet a[85]simulated the anterior chamber in a wet-lab model used to teach descemet membrane endothelial keratoplasty.The model allowed students to simulate diverse surgical procedures.
CHALLENGES AND OPPORTUNITIES/FUTURE RESEARCH DIRECTIONS
The shortage of donors and difficulties involved in donorprovided tissues are such that bio-engineered cornea and other eye tissues is an increasingly promising alternative[6,13,15,36,85].Patient-derived cells reduce the risk of aggressive immune responses, there are few studies into the immune responses elicited by bioprinted tissues/cells[86].It’s notable that bioprintingbased regenerative medicine is still in its nascent stages and many technological, practical, ethical, and even regulatory concerns that need to be addressed to bring its promise to fruition[19].
The available research on bioinks shows that copolymerization of GelMA with long-chain PEGDA can help form a less brittle PEGDA-GelMA hydrogel as PEGDA chain’s crystalline crosslinking has a toughening effect[6,15].The resulting hydrogels are not only cytocompatibility, they are also consistent with the requirements for corneal implantation as they support cell adhesion, proliferation, and migration, while achieving acceptable transparency, inflammation degree and nutrient permeation[15].
While the eye is complex and highly evolved, the cornea’s simple five-layer structural deposition easily renders itself to bioprinting even though the hydrophobic permeability of the layers and tightly interconnected junctions in epithelial cells[5].Research along the lines of Isaacsonet al[4]are required to facilitate translating bioprinted ocular materials and components as well as the entire eye for research and clinical application.By improving biometric methodologies for culturing cells, it would be possible to explore translational effect of existing studies, including possible therapeutics.With respect to the stromal tissue bioengineering, the studies included have considerable strengths and limitations that could be minimised in future research by combining their techniques/protocols[14].
Retinal bioprinting (as well as other more complex parts of the eye), is yet to progress to a level where it can create safe and adequately functional tissue[7].It’s, however, arguable that increasing research and knowledge about the other parts of the eye would ultimately translate into more breakthroughs for other areas.Critically, this review found no compelling evidence of overcoming issues such poorin vivotranslation,vascularisation, and manufacturing difficulties.More research is certainly required, particularly in respect to multi-material bioinks[13,15], scaffolding, more accurate printing techniques,and potential of combining different techniques to build on their individual strengths[32-33].
CONCLUSION
The available literature offers proof-of-concept that 3D bioprinting can fabricate structurally and functionally effective cells and tissues that mimic and integrate well with certain native cells/tissues fairly rapidly, even though the costs and that translation to clinical application remains tenuous[4].There is immense promise in the technology’s application to ophthalmology, but for this promise to be realised, morein vitroandin vivoresearch is patently required to clinically validate the findings[15,30,32,71].Clearly, the potential varies for different parts of the eye and applications, and further research is needed to move these technologies to clinical settings[72].Similarly, while it is expected that technical progress would eventual lower the costs of printing technologies to expand accessibility of the same for research and clinical application,the best available techniques remain costly[9].
This present work differs from the extant works in two respects[6,36,68].The extant works are primarily empirical or theoretical works covering different aspects of ophthalmologic applications of bioprinting, while this study offers a bird’s eye view of these works, and others.In addition, this work primarily summarises the status and research progress of bioprinting in ophthalmology.It places an emphasis on the understanding of bioprinting technologies and highlights the latest research progress (ex vivo,in vivo) on multiple fronts as well as the extent to which these diverse research directions are closer to actual clinical or practical applications.It shows that the progress in research and the closeness to clinical applications is differs greatly for different parts of the eye,on account of their complexity and function.Accordingly,the evidence suggests that the greatest promise of imminent clinical applications is likely to be highest for less complex,avascular, and innervated parts of the eye, particularly parts of the cornea, but the more complex ocular parts such as the retina still presents substantial difficulties[45-48].
ACKNOWLEDGEMENTS
Conflicts of Interest: Alatawi SK,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Visual resolution under photopic and mesopic conditions in patients with Sjögren's syndrome
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
- A combined treatment for patients with dry eye and associated laryngopharyngeal reflux: a real-life approach
