Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
Hou-Gang Li, Yan-Hui Chen, Fang Lin, Si-Yu Li, Qing-Hua Liu, Chun-Ge Yin, Xi-Yue Chen,Xin-Jie Zhang, Yue Qu, Yan-Nian Hui
1Ophthalmic Hospital of Tangshan, Tangshan 063000, Hebei Province, China
2Tianjin Jizhou District Tianyi Vision Hospital, Tianjin 300070,China
3Department of Ophthalmology, Xijing Hospital, Fourth Military Medical University, Xi’an 710023, Shaanxi Province,China
Abstract
● KEYWORDS: ocular hypertension; children; non-contact tonometer; Goldmann applanation tonometer; Corvis ST;corneal biomechanics; central corneal thickness; axial length
INTRODUCTION
Ocular hypertension (OHT), defined as intraocular pressure (IOP) of >21 mm Hg and the absence of optic disc damage or glaucomatous visual field results, is common in children ten years old or younger[1-2].Accurate IOP measurement is critical in diagnosing and managing pediatric OHT.Although children share the same range of normal IOP as adults, the physiology and pathology of OHT in children differ markedly from that in adults, resulting in a more complex condition than in adults.Most pediatric OHTs were detected by non-contact tonometer (NCT) during the visual examination or optical correction in outpatient.The disadvantages of NCT included that the accuracy showed a significant decrease in eyes with higher true IOP or thicker central corneal thickness(CCT)[3].Moreover, NCT was vulnerable to the effects of long eyelashes and frequent blinking[4].Consequently, pediatric OHT diagnosed on NCT measured IOP (NCT-IOP) alone can lead to overdiagnosis and overtreatment.
As a gold standard for IOP measurement, Goldmann applanation tonometer (GAT) must touch the eye and requires anesthesia and fluorescein drops.As previously reported,although GAT can achieve accurate IOP values compared with NCT, children often do not cooperate fully with this invasive procedure[5].In addition, CCT, corneal biomechanics, and axial length (AL) could interfere with GAT readings[6-8].
The biomechanically corrected tonometer (Corvis ST, CST) is a noncontact tonometer.CST could provide a biomechanically corrected IOP value, independent of corneal biomechanics and CCT[9].Numerous studies have demonstrated that CSTmeasured IOP (CST-IOP) provides more stable IOP readings in normal eyes[10]and eyes with ‘‘weaker’’ cornea compared with other tonometers[6,11-12].And the CST-IOP showed a high agreement with GAT measured IOP (GAT-IOP) in eyes with healthy corneas[10].Furthermore, anex vivoexperiment indicated no significant difference between CST-IOP and true IOP[13].
Given the limitations of NCT and GAT, it is thus of great importance to assess the accuracy of CST in pediatric OHT.Although GAT, NCT, and CST have been widely used in clinical practice for IOP measurement, little was known about the agreement of the three tonometries in pediatric OHT.We aimed to analyze the agreement of NCT-IOP, GAT-IOP, and CST-IOP in children with an NCT-IOP of 22 mm Hg or more and to evaluate the factors associated with differences in three tonometries.These results may help to explore the utility of CST in pediatric OHT.
SUBJECTS AND METHODS
Ethical ApprovalThis cross-sectional study was performed in the Ophthalmology Hospital of Tangshan from November 2021 to May 2022.A total of 42 children (aged 7 to 14)were enrolled.All participants’ parents signed the informed consent.This study was approved by the Ethics Committee of the Ophthalmology Hospital of Tangshan and complied with the Declaration of Helsinki (approval number: YKYYLL-2022-22).
The inclusion criteria included an untreated NCT-IOP≥22 mm Hg in at least one eye with normal anterior segment structure and best-corrected visual acuity (BCVA) of 20/25 or better, without visual field defects or optic nerve damage.If both eyes were eligible, both were selected.
This study’s exclusion criteria included a history of eye surgery, eye trauma, contact lens wear, corneal astigmatism of 2 D or more, strabismus, congenital eye disease, and topical or systemic corticosteroid application within three months.
All enrolled children underwent comprehensive ophthalmic examinations, including slit-lamp biomicroscopy, BCVA,refractive error, and spherical equivalent (phoropter, VT-10;Topcon, Japan), AL, CCT, and corneal curvature measurement(IOL Master 700, Carl Zeiss Meditec, Jena, Germany), at least two reliable standard automated perimetry with the Octopus(Haag-Streit International, Koeniz, Switzerland; G1 TOP test strategy).Reliable visual field defined as a false-negative rate of <25%, a false-positive rate of <25%, and fixation losses of<20%, and reliability factor not greater than 15%.
IOP Measurement ProceduresAll IOP measurements were performed from 2:00 to 5:00p.m.Children were emotionally stable and avoided blinking.The order of IOP measurement was NCT (Topcon, Tokyo, Japan), CST (Oculus, Wetzlar,Germany), and GAT (AT 20, Carl Zeiss, Germany) with a 10-min interval between three tonometry.NCT was performed with three or more measurements per eye, three values with fluctuation of 3 mm Hg or less were chosen, and the average value was named the NCT-IOP.CST was performed at least twice per eye with an interval of >2min between examinations, and the mean values were named CST-IOP.GAT was performed under topic anesthesia, three consecutive measurements of each eye were taken, and the mean values were named GAT-IOP.Three experienced technicians who were blinded to the patient’s condition performed NCT, CST,and GAT.
Stereo Digital Photographs ExaminationStereo digital photographs of the fundus were acquired with a Kowa Nonmyd WX 3D (2D/3D non-mydriatic retinal camera, Kowa,Japan).Vertical cup-to-disc ratio, optic disc area, rim area,and rim volume were automatically measured with built-in software.Corneal curvature and spherical equivalent were used to adjust the ocular magnification.
Statistical AnalysesSPSS 25.0 and MedCalc(version 19.3.0, Ostend, Belgium) were used for data analysis.The normal distribution of data was assessed using the K-S single sample test.For normal data, data were presented as mean±SD or percentages, and differences between groups were compared using the independent samplet-test or Chi-square test.For nonnormal data, variables were represented as medians (upper quartile, lower quartile), and differences between groups were compared using the Mann-WhitneyUtest.The difference between GAT-IOP, CST-IOP, and NCT-IOP in each group were compared by repeated measurement ANOVA with Bonferroni post hoc test.Bland-Altman plots assessed the agreement between GAT-IOP, CST-IOP, and NCT-IOP.Pearson correlation coefficient (r) analyzed the factors associated with the difference between GAT-IOP, NCT-IOP, and CST-IOP.P<0.05 was considered statistically significant.
RESULTS
Initially, we enrolled 80 eyes (42 children) with NCT-IOP of 22 mm Hg or more.Of them, GAT measurement was performed in 51 eyes.Finally, fifty-one eyes performed GAT,CST, and NCT were divided into two groups: the OHT group(with GAT-IOP≥22 mm Hg) and the non-OHT group (with GAT-IOP<22 mm Hg).
Demographic and Clinical Characteristics of Subjects in Two GroupsFifty-one eyes (30 patients) completed the GAT measurement, with a GAT success rate of 63.75%.Mean age was 9.88±2.01y, median AL 23.81 mm, male 27.45%, right eyes 47.06%.Mean CST-IOP was 21.70±2.75 mm Hg, with median NCT-IOP 24.90 mm Hg, and median GAT-IOP 21.00 mm Hg.The relationship between age and IOP values(values obtained by GAT, CST, and NCT) was nonlinear.Peaks in CST-IOP and GAT-IOP occurred at age 8 years old and NCT-IOP at age 11, followed by the decrease in IOP with the age increasing in all three tonometries (Figures 1, 2).
There was no significant difference in age, AL, sex, disc area,rim area, and the cup-to-disc ratio between the OHT group and non-OHT group (allP>0.05).The rim volume and CCT were significantly lower in the OHT group than in the non-OHT group (P<0.05; Table 1).
Differences of CST-IOP, NCT-IOP and GAT-IOPThe differences between CST-IOP and GAT-IOP were lower than those between NCT-IOP and GAT-IOP in both groups(allP<0.001).The difference between CST-IOP and GATwas insignificant between the OHT and non-OHT groups(P=0.800).The differences between NCT-IOP and GATIOP and the differences between CST-IOP and NCT-IOP significantly differed between both groups (allP<0.05; Table 2).Agreement of IOP Measurement Among Three DevicesThe Bland-Altmann analysis plots illustrated the agreement and the difference in IOP among devices (Figure 3).CST showed better agreement with GAT than NCT did in the OHT group(mean IOP difference: 1.26 and 3.90 mm Hg, respectively,P<0.001), in non-OHT group (mean IOP difference: 1.20 and 6.00 mm Hg, respectively,P<0.001), and in all subjects (mean IOP difference: 1.23 and 5.00 mm Hg, respectively,P<0.001).
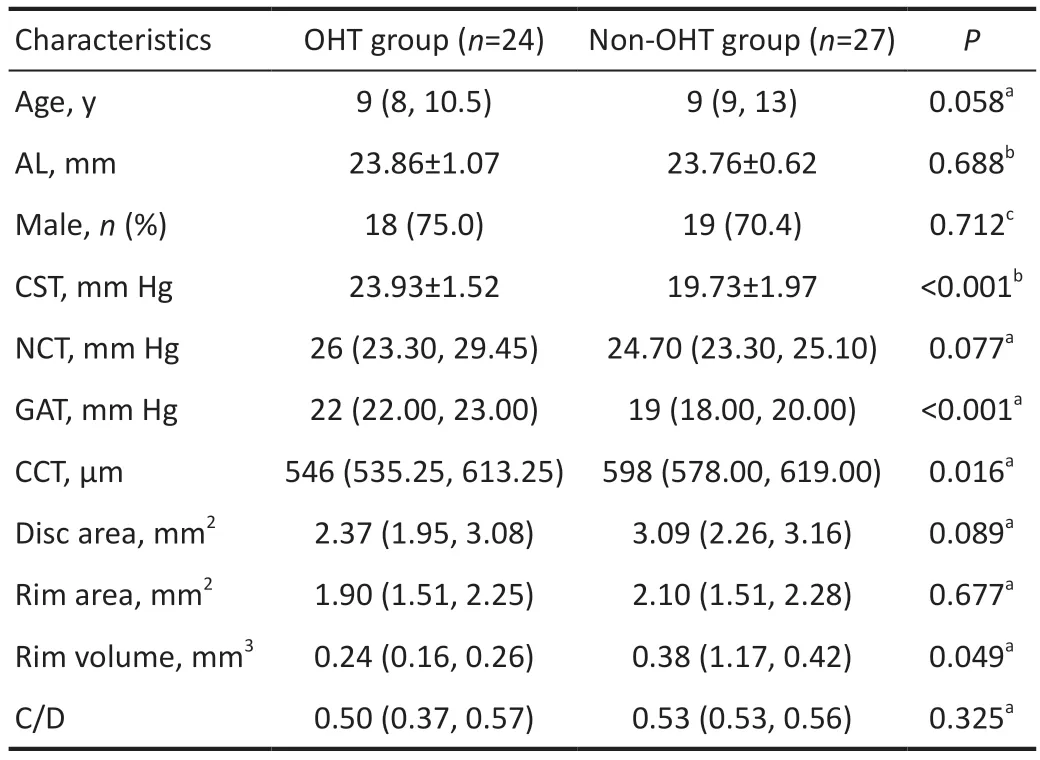
Table 1 Differences of characteristics between the OHT group and non-OHT group
Correlations Between the IOP Difference, CCT, AL, Optic Disc Rim Volume, and AgePearson correlation coefficients evaluated the influence of CCT, AL, optic disc rim volume,and age on the IOP difference between three tonometry reading in each group (Table 3).
The difference between CST-IOP and GAT-IOP was not associated with age, AL, optic disc rim volume, and CCT in all subjects and two groups (allP>0.05).The difference between NCT-IOP and GAT-IOP was positively correlated with CCT in all subjects (r=0.85,P<0.001) and in the OHT group (r=0.93,P<0.001) and associated with CCT (r=0.66,P<0.001),AL (r=-0.81,P<0.001), and optic disc rim volume (r=-0.41,P<0.036) in the non-OHT group.The difference between CSTIOP and NCT-IOP was correlated with CCT in all subjects(r=-0.82,P<0.001) and in the OHT group (r=-0.91,P<0.001)and associated with CCT (r=-0.58,P=0.001) and AL (r=0.69,P<0.001) in the non-OHT group.

Figure 2 Scatter plots of IOP measured by biomechanically corrected tonometry (Corvis ST), non-contact tonometry and Goldmann applanation tonometry in the total children (A), OHT group (B),and non-OHT group (C) OHT: Ocular hypertension group; NCT: Noncontact tonometry; GAT: Goldmann applanation tonometry; CST:Corvis ST.
DISCUSSION
The incidence of OHT is very high in children[2].IOP in children with OHT may be as high as 28 to 36 mm Hg[14-15].In the present study, the maximal NCT, GAT, and CST were 33.00, 26.00, and 28.1 mm Hg, respectively.The peak IOP of CST and GAT occurred at age 8y and NCT at age 11y.IOP measurement is central to the management of glaucoma and OHT in children.Children often do not cooperate fully for GAT due to the need for contact with the cornea, which may hinder its practical application.Compared to GAT, CST measurement is more easily administered in children without contact with the cornea.Similar to previous studies[16], the success rate of GAT measurement in the current research was 63.75% (51 eyes); meanwhile, the success rate of CST measurement was 100%.In all 51 eyes with NCT-IOP≥22 mm Hg, 27 (52.94%) were false OHT, the accuracy of NCT in the diagnosis of pediatric OHT was only 47.06%,using GAT-IOP as a reference.
The result of OHT Treatment Study[17]indicated that OHT patients with thin CCT were more likely to develop open-angle glaucoma.Thin CCT represents an increase in lamina cribrosa compliance, contributing to the deformation of lamina cribrosa under high IOP[18].Our study found that CCT in the OHT group was significantly thinner than in the non-OHT group (546vs578 μm).Compared with the non-OHT group, rim volume was lower in the OHT group, despite the absence of significant glaucomatous optic nerve damage in all enrolled eyes.This result suggests that elevated IOP may impact the structure of optic nerve head[19-20].Glaucoma may result in irreversible visual impairment in children, which is responsible for 5%of blindness in children worldwide[21-22].A decrease in IOP is the only reliable treatment strategy for pediatric glaucoma[23].Accordingly, accurate measurement of IOP and optic nerve assessment should be considered in children, although less than 10% of untreated OHT progress to glaucoma after 5-10y[21,24].In addition, CCT thickening can lead to an increase in eyeball stiffness which might contribute to IOP overestimation,which increases the difference between NCT and GAT[25-26].Consistent with the previous study, our result indicated that the difference between NCT and GAT in the non-OHT group was more significant than in the OHT group (P=0.007).Moreover,the difference between NCT and GAT showed a strong positive correlation with CCT.
Notably, it has also been suggested that elevated IOP can also cause corneal edemaviaa pressure gradient, ultimately resulting in increased CCT[27].Therefore, the relationship between CCT and IOP in children remains uncertain[28].It appears progressively more evident that the true IOP is likely unpredictable with linear correction formulas for CCT.At the same time, the corneal biomechanics might likely contribute, together with CCT, to the tonometric artifact[29].Compared to GAT and NCT, CST adequately accounted for corneal biomechanical properties and provided a more comprehensive performance for IOP assessment[6,11,13].In a study by Halkiadakiset al[30]no correlation was found between CST-IOP and CCT in eyes with OHT, primary open angle glaucoma, or normal eyes.In the present study, CST-IOP and GAT-IOP showed better consistency in the OHT group, non-OHT group, and all subjects compared with NCT-IOP.The difference between CST-IOP and GAT-IOP was not significant between the two groups and was unrelated to CCT.These results were in agreement with Honget al’s study[31].
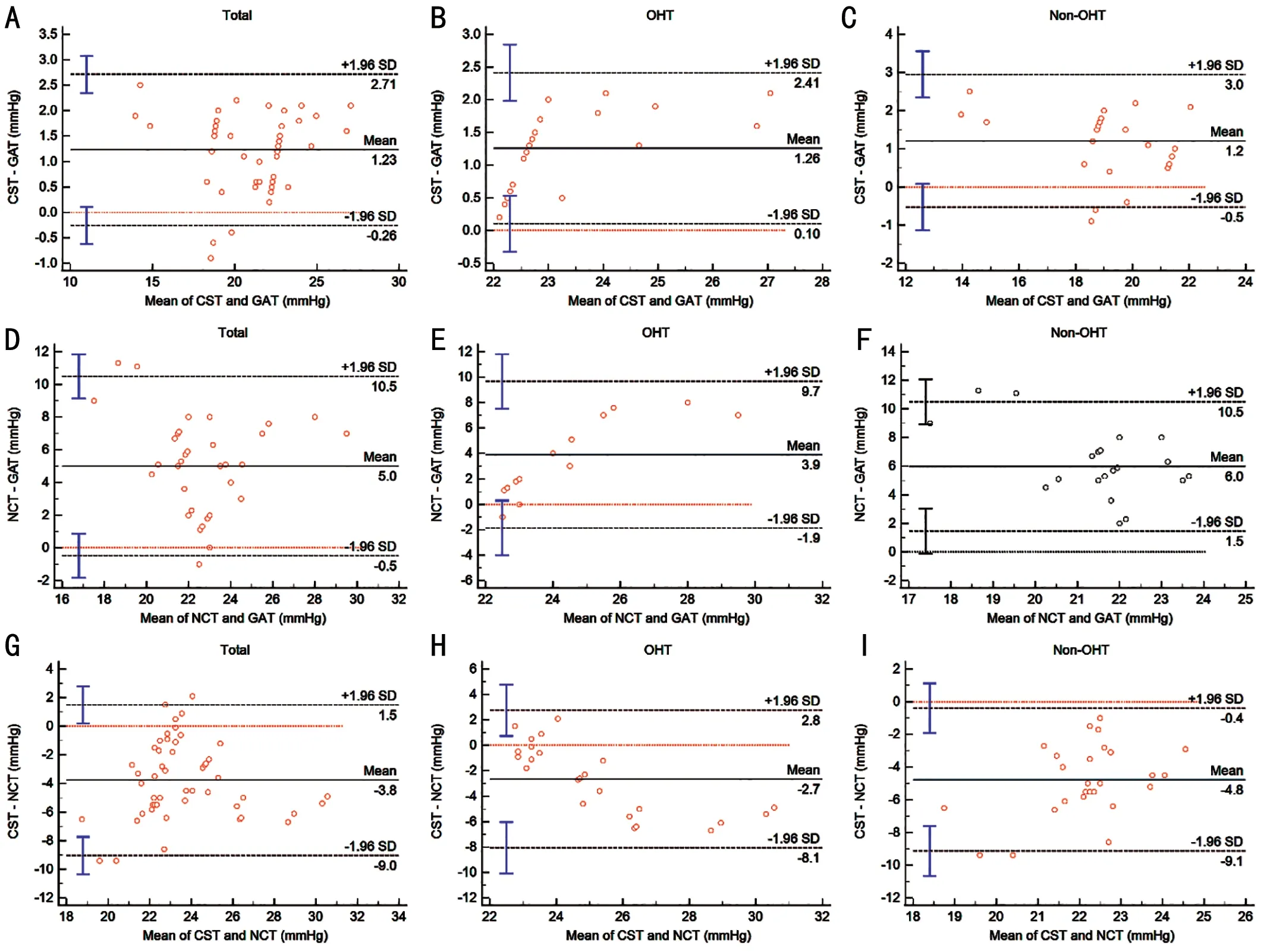
Figure 3 Bland-Altman scatter plot showing the agreement among different IOP measurement devices The Bland-Altmann analysis plots illustrate the agreement of IOP between devices in total groups (A, D, and G), OHT group (B, E, and H), and non-OHT group (C, F, and I).Dotted lines show 95% limits of agreement; IOP: Intraocular pressure; OHT: Ocular hypertension group; CST: Biomechanically corrected tonometry(Corvis ST); NCT: Non-contact tonometry; GAT: Goldmann applanation tonometry.

Table 2 Intra- and intergroup comparisons between the differences in three tonometry readings mean±SD
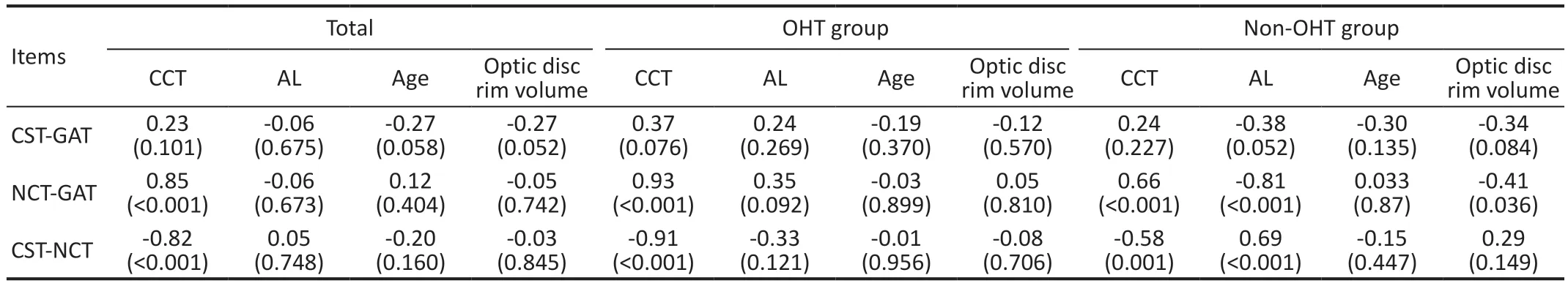
Table 3 Correlation of CCT, AL, optic disc rim volume, and age with the differences in three tonometry readings r (P)
IOP increase may play a critical role in myopia development[32-34].The association of elevated IOP and elongated AL or an increased myopic refractive error was found in children[1,35-36].In the current research, the difference between NCT-IOP and GAT-IOP and the difference between NCT-IOP and CST-IOP negatively correlated with AL in the non-OHT group.This result may be due to a positive correlation between AL and GAT-IOP or CST-IOP, which reduces the difference between NCT-IOP and GAT-IOP or CST-IOP.Interestingly, there was no significant relationship between AL and the difference between NCT-IOP and GAT-IOP in the OHT group.We cannot explain this result.It might be due to a small sample in our study.Several studies indicated that increased AL was associated with elevated IOP[1,35-37], although longitudinal analysis suggested that IOP had essentially no relationship with myopia progression in school children[32-34].Moreover,previous results suggested that increased scleral compliance due to AL prolongation may cause slightly lower IOP due to biased tonometry[34].The relationship between IOP and AL is very confounded and needs further exploration.
There are two significant limitations in this study.First,the relationship between IOP, CCT, AL, and age has been challenging to resolve because of its cross-sectional nature.Although optic nerve structure analysis was performed in the current study, the long-term ocular course of children with OHT may provide additional insight regarding the relationship of IOP, AL, corneal material properties, and optic nerve structure.Second, small sample sizes may lead to selective bias in parameter measurement and incorrect estimation of the association between IOP and other ocular parameters.
In conclusion, the agreement of CST-IOP and GAT-IOP was significantly better than NCT-IOP and GAT-IOP in children with NCT-IOP of 22 mm Hg or more.Moreover, no significant relationship was found between the difference between CSTIOP and GAT-IOP and CCT, AL, and age in all groups.Both CCT thickening and AL shorting might contribute to the overestimation of NCT measurement.For children with NCTIOP≥22 mm Hg, who cannot tolerate GAT, CST measurements can be used as an alternative.
ACKNOWLEDGEMENTS
Authors’ contributions:Chen YH had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.Concept and design:Chen YH and Hui YN.Acquisition, analysis, or interpretation of data: Li HG, Lin F, Li SY, Liu QH, Yin CG, Chen XY,Zhang XJ, Qu Y.
Foundation:Supported by Medical Science Research Project of Hebei Province in 2023 (No.20231818).
Conflicts of Interest: Li HG,None;Chen YH,None;Lin F,None;Li SY, None;Liu QH,None;Yin CG,None;Chen XY,None;Zhang XJ,None;Qu Y,None;Hui YN,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Visual resolution under photopic and mesopic conditions in patients with Sjögren's syndrome
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Three-dimensional bioprinting in ophthalmic care
- A combined treatment for patients with dry eye and associated laryngopharyngeal reflux: a real-life approach
