Visual resolution under photopic and mesopic conditions in patients with Sjögren's syndrome
Mosaad Alhassan, Amal Aldarwesh, Issa Alessa, Rafif Alhijji, Reema Alduhayan, Ali Almustanyir
1Department of Optometry, College of Applied Medical Sciences, King Saud University, Riyadh 11433, Saudi Arabia
2Imaging Research Department, King Abdullah International Medical Research Center, King Saud bin Abdelaziz University for Health Sciences, Riyadh 11481, Saudi Arabia
Abstract
● KEYWORDS: Sjögren’s syndrome; dry eye; visual acuity;contrast sensitivity; mesopic; night vision
INTRODUCTION
Primary Sjögren’s syndrome (SS) is a chronic autoimmune disease that progressively destroys the exocrine glands due to lymphocytic cell infiltration.The hallmark symptoms of the disease are xerostomia and xerophthalmia[1].Secondary SS coincides with connective tissue diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA)[1].As with other autoimmune diseases, the prevalence of primary SS has different rates worldwide[2-3].However, middle-aged women remain highly affected compared to men in a ratio of approximately 9:1[2], with a higher reported incidence in RA and SLE patients[4].
Although patients with SS have an increased risk of severe complications such as cardiovascular diseases and non-Hodgkin’s lymphoma, their quality of life is profoundly affected due to the triad of the disease; polyarthritis, xerostomia and xerophthalmia, a well-known as keratoconjunctivitis sicca or dry eye[1].Although most SS patients report complaints about ocular dryness, a common symptom, other eye-threatening manifestations such as corneal ulcer, conjunctivitis, uveitis,optic neuritis, and retinal vasculitis are also reported[5].
Dry eye negatively impacts visual functions including visual acuity and contrast sensitivity, as both depend on pre-corneal tear film stability and quality.If the tear film is degraded,image quality to the retina is distorted and therefore, visual function declines.In secondary SS patients, surface alteration due to dryness has caused deleterious effects on visual acuity more severely than the primary SS ones[6].Moreover, a recent study has shown that the greater tear film instability, the worse contrast sensitivity in dry eye patients[6].Likewise, dry eye can lead to central superficial punctate keratopathy, significantly reducing contrast sensitivity and increasing straylight[7].In primary SS, installing artificial tears with mucoadhesive properties that prolong the residence time moderately improved the contrast sensitivity, reflecting the significance of tear film stability on the health of the ocular surface[8].
Dryness is treated with multiple approaches, including artificial tears for mild dryness and topical steroids to control the ocular surface inflammatory response.Oral secretagogues such as pilocarpine, a parasympathomimetic that stimulates muscarinic receptors in the lacrimal and salivary glands and effectively alleviates the symptoms of dry eye and mouth[9].Furthermore,under low light levels, pilocarpine induces miosis may blur vision, reduce visual functions, and affect day-to-day activities such as driving under streetlights at night[10].The disease has visual sequelae in patients with SS.But this, alongside its treatment, is the least investigated.Very few studies have investigated the visual functions routinely measured among SS patients, and the extent of visual function alteration under low light levels has not been fully addressed.This cross-sectional study examines the clinical visual functions, including visual acuity for high and low contrast letters and contrast sensitivity in daylight (photopic) and dim light (mesopic) conditions.
This cross-sectional study is the first to describe the impact of the xerophthalmia state on different visual resolution tasks in SS patients.The hypothesis is that SS patients have more visual perceptual difficulties than healthy people, especially under low light levels, compared to healthy individuals.This effect may be augmented by parasympathomimetic agents such as pilocarpine.The aim was achieved by examining different visual functions, including the visual acuity for high and low contrast letters and contrast sensitivity function in both daylight (photopic) and dim light (mesopic) conditions.
The results of this study suggest the importance of performing a comprehensive eye examination in patients with SS rather than standardized visual assessment tests.
SUBJECTS AND METHODS
Ethical ApprovalAll research participants were recruited from the rheumatology clinic at King Khalid University Hospital in King Saud University, Riyadh, Saudi Arabia.All subjects were given informed written consent before participation.The study was approved by the Institutional Review Board (IRB) Committee at King Saud University (IRB Approval Project No.E-21-6002).
ParticipantsTwo groups of participants were recruited for this study.The first group was patients with SS (n=21).All patients were clinically diagnosed by a qualified rheumatologist as having primary or secondary SS based on the criteria of the American-European study group[11].The second group was age-matched healthy control participants (n=21) who were free from ocular or systemic diseases.
The exclusion criteria for all participants were a history of diabetes, ocular disease such as corneal infection, cataract,glaucoma, retinal neuropathy, previous refractive surgery, and/or corrected visual acuity worse than 20/30 at a distance in either eye.
ProceduresThe study was started by objectively determining the severity of dry eye in patients and healthy controls by applying Schirmer’s test without local anaesthesia, and then subjectively by filling the standardized Ocular Surface Disease Index (OSDI).The OSDI is a rapid assessment of ocular symptoms due to dryness and their impact on vision-related functioning[12].Then, visual acuity was measured monocularly to determine whether the participants met the eligibility criteria.If they did not meet the acuity requirement, then acuity was reassessed with a pinhole.If the acuity improved, then subjective refraction was performed.Next, high-contrast visual acuity, low-contrast visual acuity (3% contrast), and contrast sensitivity were measured while participants were wearing their habitual distance glasses or with modified refractive power using trial lenses and a frame.High and low contrast visual acuities were measured binocularly at a 4-m distance using Early Treatment Diabetic Retinopathy Study (ETDRS)charts[13].Participants started reading from the largest letter size and continued to read the smaller letter rows.Testing ended when participants read 2 out of 5 letters correctly.Then, visual acuity was recorded using the logMAR system, in which each letter equals 0.02 logMAR.Visual acuity was measured under different conditions by using different versions of letters to avoid the memorizing effect.
Contrast sensitivity and contrast sensitivity function were measured using the CSV-1000E chart.The CSV-1000E provides a full range of contrast sensitivity enabling the examiner to construct a contrast sensitivity function.This test consists of four levels of sine-wave spatial frequencies that increase gradually, and in each level, there are two lines of circles.One of the circles contains vertical sine-waves and the other is blank, so the participant has to determine the circle with a sine-wave pattern.The test is presented at 2.5 m distant which allows measuring contrast sensitivity with spatial frequencies of 3, 6, 12, and 18 cycles per degree.For each level of spatial frequency, there are 8 different levels of contrast that decreased in a systemic way from 0.045 to 2.00, 0.7 to 2.20,0.78 to 2.26, 0.6 to 2.08, and 0.3 to 1.81, respectively.The contrast threshold in log units can be independently defined for each level of spatial frequency as the last level of contrast the participant can correctly identify the sine-wave pattern.The contrast sensitivity function can be constructed by determining the contrast sensitivity for each level of spatial frequency[14].
The visual charts were mounted in an ESV3000 selfilluminated cabinet (Good-Lite, Elgin, IL, USA).The light level of the illuminated cabinet can be automatically calibrated to provide different lighting levels (photopicvsmesopic).The photopic light level is 85 cd/m2, and the mesopic level is 3 cd/m2.These light levels are recommended by the National Academy of Sciences committee for vision testing standards and are required by the FDA for vision evaluation in clinical trials.Visual tests were measured first under high light level(i.e., photopic condition) and then under low light level (i.e.,mesopic condition).For low light level measurements, the room lights were turned offand participants were adapted to the lower dim light for five minutes.The five minutes interval for dark adaptation was selected so that both cone and rod photoreceptors were providing inputs (mesopic condition)[15].

Figure 1 The VA of SS patients and healthy participants under different testing conditions VA: Visual acuity; SS: Sjögren’s syndrome.
Data AnalysisComparison of visual acuity tests under different lighting conditions was analyzed between groups using the repeated measures analysis of variance (RMANOVA)model (IBM SPSS version 24, USA), with the various contrast levels and lighting conditions as the within-subjects factor and the two groups as the between-subjects factor.Similarly,comparison for each spatial frequency of contrast sensitivity level under different lighting conditions was analyzed independently between groups using the RMANOVA model,with the various lighting conditions as the within-subject factors and the two groups as the between-subjects factor.The criterion ofP<0.05 was used to determine a significant effect.
RESULTS
Demographic CharacteristicsPatients with SS were classified as having primary or secondary syndrome disease.There were 14 patients with primary syndrome and 7 with secondary syndrome.The results of comparisons between groups did not show any significant differences in visual acuity or contrast sensitivity measurements at all levels (P>0.05).For this reason, all SS patients were pooled into one group for further analysis.
Different demographic characteristics of the participants SS patients showed significant eye dryness based on Schirmer’s test and OSDI score results compared to healthy controls(Table 1).
Comparisons of Sjögren’s Syndrome Patients with Healthy Controls
High and low contrasts visual acuities under photopic and mesopic conditionsThe visual acuity of the two groups under different lighting conditions is presented in Table 2.In addition, Figure 1 shows the mean values of high and low contrast visual acuity under two light levels.As expected,visual acuities were lower for low contrast letters (F=366.486,P<0.0001), and lower light levels (F=74.25,P<0.0001).There was also a significant interaction in contrast by light levels(F=10.92,P=0.002) confirming that the low contrast acuity was affected more than high contrast acuity by the decrease in the light level.
The difference between groups was not significant (F=1.03,P=0.317).The interactions that included groups were not significant as well.First, there was no significant interaction between groups and contrast levels (F=0.17,P=0.678),and no significant interaction between groups and light levels (F=0.21,P=0.647).The interaction between different contrasts, light levels, and groups was not significant as well(F=1.18,P=0.283).Taken together, the data showed that SS patient group had lower high and low contrast visual acuity by small amount compared to healthy controls.However, the reduction in visual acuities did not reach to significance levels.Nevertheless, the difference between groups in high contrast visual acuity under mesopic condition was more than one line which is considered clinically significant.Lowering light level and/or contrast level reduced visual acuity in both groups by the same amount.
Contrast sensitivity under photopic and mesopic conditionsTable 3 lists the means, standard error of the means (SEMs),and 95% confidence intervals (CI) for four spatial frequencies contrast sensitivity values in log units for both groups.As expected, the contrast sensitivity was significantly lower under low light levels for all spatial frequencies (P<0.0001).The interaction between groups and light levels was statistically significant in 6, 12, and 18 cpd only (P<0.05), and it wasnot significant in 3 cpd spatial frequency (P=0.856).Figure 2 shows the mean of contrast sensitivity for 12 cpd in two lighting conditions for both groups.Between groups comparison showed significant difference in high spatial frequency (i.e., 18 cpd) only (F=4.625,P=0.038).

Table 2 Visual acuity tests under different conditions

Table 3 Contrast sensitivity tests under different conditions in log units
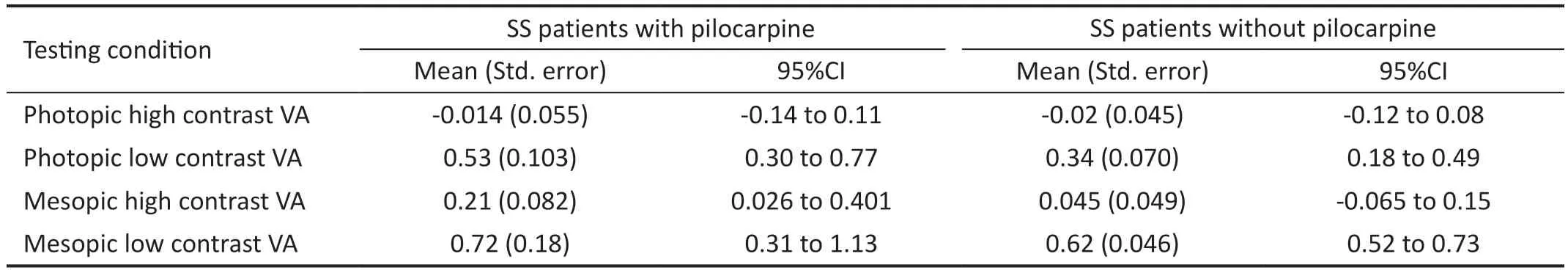
Table 4 Visual acuity tests under different conditions in patients with and without pilocarpine
These results suggest that contrast sensitivity is affected to a greater extent in SS patients than healthy controls in high spatial frequency (i.e., 18 cpd).Also, reducing the light level showed significant effect on contrast sensitivity among SS patients more than healthy controls in medium and high spatial frequencies.Figure 3 shows an example of contrast sensitivity functions for one SS patient and one healthy control.It is obvious that the patient had larger reduction in high spatial frequency targets (i.e., 12 and 18 cpd) more than the healthy control especially in mesopic lighting condition.
Comparisons of Sjögren syndrome patients with and without pilocarpinePatients with SS were classified as taking pilocarpine (on-pilocarpine) and those without (offpilocarpine).There were ten patients on pilocarpine and 11 patients off-pilocarpine treatment.The two groups are agematched and had no significant differences in Schirmer’s test or OSDI score results.The same analysis was carried out to compare these two groups.
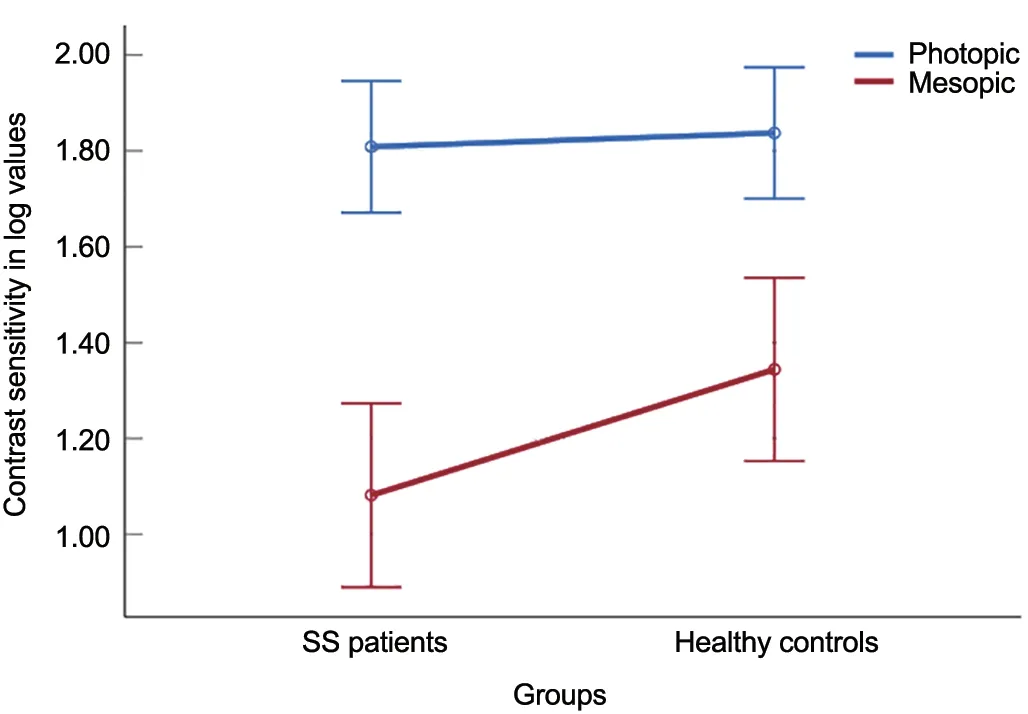
Figure 2 Means plot of contrast sensitivity at 12 cycle per degree for each group SS: Sjögren’s syndrome.

Figure 3 Contrast sensitivity functions under different lighting conditions for one SS patient and one healthy control cpd: Cycle per degree;SS: Sjögren’s syndrome.
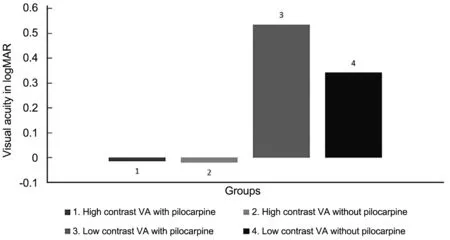
Figure 4 Effect of pilocarpine on the VA under photopic conditions VA: Visual acuity.
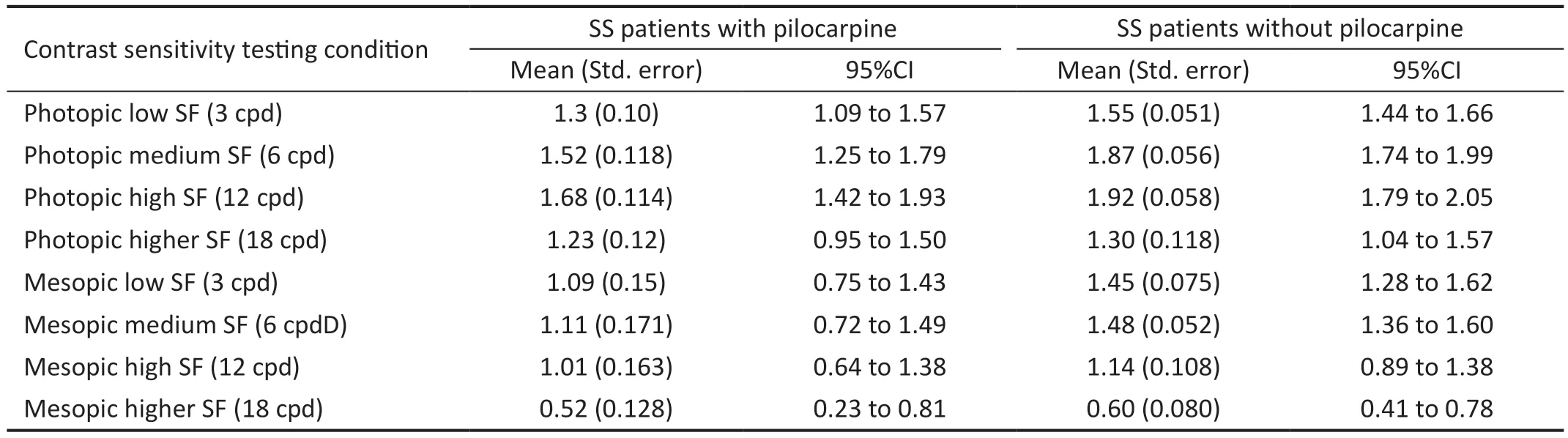
Table 5 Effect of pilocarpine on contrast sensitivity tests under different conditions in log units
High and low contrasts visual acuities under photopic and mesopic conditionsTable 4 lists the means, standard error of the means (SEMs), and 95% confidence intervals for the two groups.The differences between groups were not significant(F=1.29,P=0.269).The interactions that included groups were not significant as well.First, there was no significant interaction between groups and contrast levels (F=0.374,P=0.548), and no significant interaction between groups and light levels (F=0.671,P=0.671).The interaction between different contrasts, light levels, and groups was also not significant, but it was approaching to be significant (F=3.47,P=0.078).Figure 4 shows the bar chart of the mean values for the high and low contrast visual acuity under photopic lighting conditions.The figure shows that the on-pilocarpine SS patients had worse low contrast visual acuity under photopic conditions than off-pilocarpine patients by 0.2 logMAR units,equal to two lines on the visual acuity chart.This difference is considered clinically significant even though statistically is not.
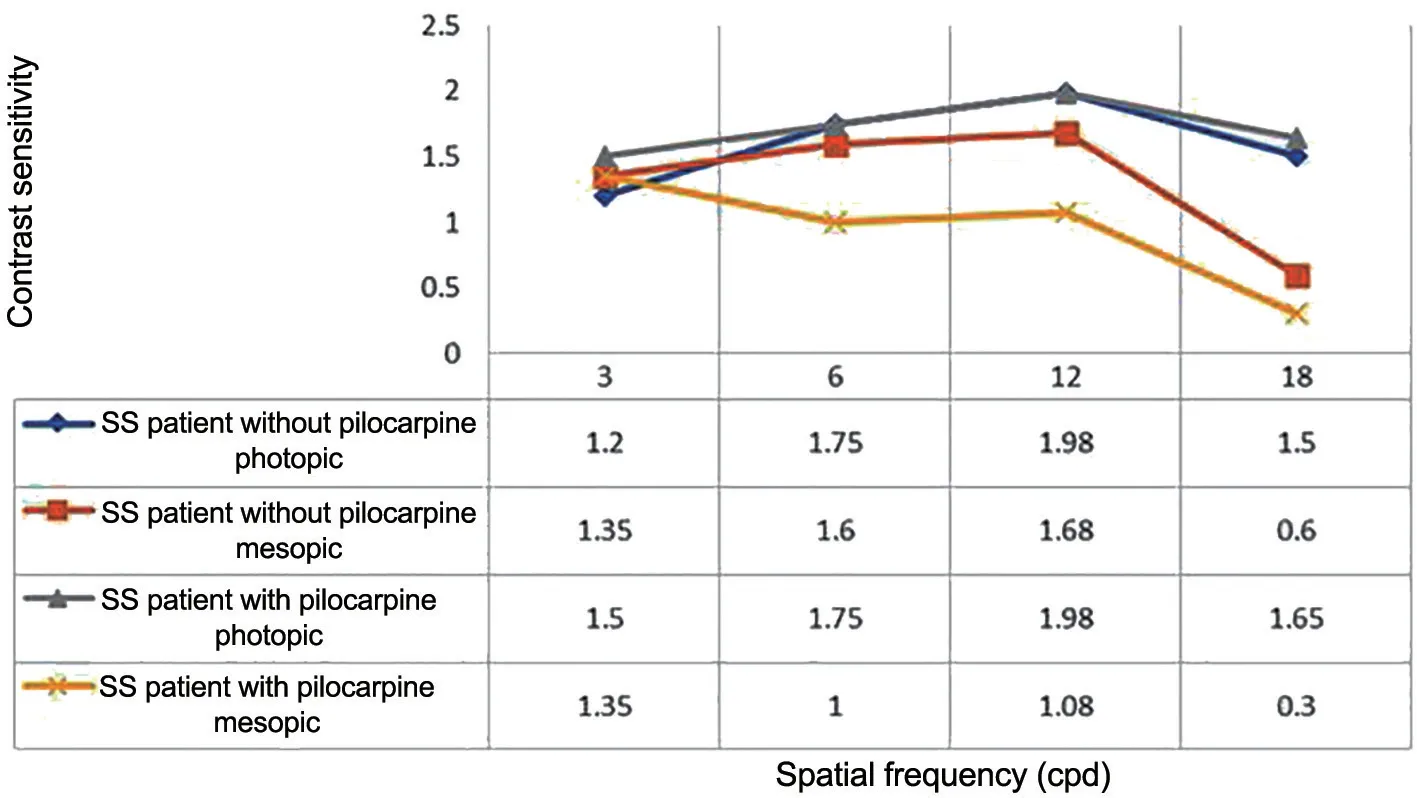
Figure 5 Contrast sensitivity functions under different lighting conditions for one Sjögren’s syndrome (SS) patient on-pilocarpine and one SS patient off-pilocarpine cpd: Cycle per degree.
Effect of pilocarpine on the contrast sensitivity under photopic and mesopic conditionsTable 5 lists the means,SEMs, and 95%CI for 4 spatial frequencies contrast sensitivity values in log units for the two groups.Between groups comparisons showed significant differences in low and medium spatial frequencies (i.e., 3 and 6 cpd), but not high spatial frequency (i.e., 12 and 18 cpd).The statistical test for 3 cpd was (F=5.57,P=0.029), for 6 cpd (F=7,P=0.016), for 12 cpd was (F=1.57,P=0.224), and for 18 cpd was (F=0.372,P=0.549).The interaction of lighting levels and groups were not significant for all spatial frequencies.These results suggest that contrast sensitivity is affected to a greater extent in onpilocarpine SS patients than in off-pilocarpine patients at low and medium spatial frequencies.Reducing light levels affected contrast sensitivity in both groups by the same amount.Figure 5 shows an example of contrast sensitivity functions for one on-pilocarpine patient and one off-pilocarpine patient.It is evident that the on-pilocarpine patient had a larger reduction in low and medium spatial frequency targets (i.e., 3 and 6 cpd)than the off-pilocarpine one.
DISCUSSION
To the best of our knowledge, this is the first study to examine different visual functions of SS patients under different light levels.As SS patients may suffer from varying degrees of eye dryness, those individuals are likely to complain of a visual blur.Approximately 50% of patients with systemic inflammatory diseases including SS patients seek ophthalmic consultation due to dry-eye symptoms or blurred vision[16].Dry eye causes tear film and corneal surface instability, impairing basic visual functions such as visual acuity and contrast sensitivity[17].As visual acuity worsens, the mean score of the vision-related subscale of the standardized OSDI also worsens[17].SS and non-Sjögren’s-related dry eye disease are associated with declining quality of life[18-20].
Using the best optically corrected high-contrast visual acuity under photopic conditions, our study found no significant difference between SS patients and healthy group.These results are in agreement to finding by Arikanet al[21], who reported normal contrast sensitivity at all spatial frequencies in patients with primary SS.Similarly, the best optically corrected high-contrast visual acuity under mesopic condition showed no significant differences between the two groups.Despite having no significant differences, the difference in the mean high contrast acuities under mesopic conditions between groups was more than one line in the logMAR chart, which marked a clinically significant difference.Low contrast visual acuity under photopic and mesopic conditions demonstrated a similar pattern between groups.The small difference between groups can be accounted for by the inclusion criterion restricted to individuals with an acuity of 0.2 logMAR (6/9) or higher.Thus, the range of acuities within the sample was small.
Using the standard visual acuity may not be sensitive enough to detect visual dysfunction in dry-eye patients, thus, may not reveal helpful findings to manage those patients.Contrast sensitivity has proven to be a more effective measure of visual functions[7,22].Thus, it is crucial to evaluate vision in more functional methods by measuring contrast sensitivity at various spatial frequencies.This study found that the two groups are almost identical in contrast sensitivities under photopic conditions at low and medium spatial frequencies.Yet, contrast sensitivity in high spatial frequency (i.e., 18 cpd) was found to be significantly worse in SS patients than the healthy control group.Reducing light level frequency (i.e., mesopic condition)decreased contrast sensitivity to a greater amount in SS patients than healthy controls in medium (6 cpd) and high (12, 18 cpd)spatial frequencies.A previous study by Zhanget al[8](2013)indicated that contrast sensitivity under photopic condition was significantly lower in SS patients compared to the healthy controlled group at middle spatial frequency (i.e., 3 and 6 cpd),and after applying eye lubricants, the loss in contrast sensitivity was improved.Contrary to this, another study reported no significant difference at all spatial frequencies[21].
Pharmacological stimulation with the muscarinic agonist pilocarpine is considered for managing patients with moderate glandular dysfunction to relieve xerostomia and xerophthalmia in SS patients[9].In the current study, a small proportion of patients were placed on pilocarpine in addition to their antiinflammatory regimen.The authors postulated that pilocarpine may have consequences on visual functions.In fact, the reduction of visual acuities of patients with pilocarpine treatment was worse than those not who did not undergo the therapy.The likeable explanation of this could relate to the miotic effect of the drug.Moreover, our study showed that onpilocarpine patients had worse high and low-contrast visual acuity than off-pilocarpine patients.The difference is getting larger under mesopic conditions.The statistical difference between the two groups neared the level of significance.In all conditions, the difference is more than one line on the logMAR chart, which is clinically meaningful.Also, on-pilocarpine patients were two lines lower on the low-contrast visual acuity chart than off-pilocarpine patients and, similarly, lower in low and medium-contrast sensitivity tests under photopic conditions.Particularly under low light conditions, the patients with pilocarpine treatment generally showed a larger effect than the latter group.That is probably due to the miotic effect during dim light[10].
The work of this study has some limitations.First, SS patients who are included in this study are not all considered as having primary SS.Thus, it would be worth in future studies to include only patients with primary SS to investigate the effect of eye dryness solely due to primary SS on visual performance.Second, the reduction in image resolution that is shown in this study is due to multiple factors.It is important take into consideration other factors before making conclusive statements about visual reduction in SS patients.Severe eye dryness is not the only factor that led to reduction in the retinal image quality among SS patients.It is important to evaluate whether reduction in visual acuity and contrast sensitivity is associate with other ocular abnormalities as a result of severe eye dryness.For example, severe eye dryness led to corneal high order aberrations (HOAs) which has greater impact on image quality especially during night[21].Also, it has been reported that SS patients may experience a decline in visual acuity and contrast sensitivity before diagnosis or at the early stage of the disease, which may not be associated with dry eye symptoms.These disturbances could be linked to optic neuropathy, one of the initial ocular manifestations related to SS[23].Performing multiple associations between reduction in visual acuity and/or contrasts sensitivity at various lighting levels with different ocular structures in SS patients may be to consider in future studies.
In conclusion, this study showed that patients with SS have more significant visual function impairment than healthy controls.The impairment was heightened under low light levels.The visual disturbances at early stages may be minimal in which the standard visual acuity is inefficient in detecting these changes.Thus, a clinically meaningful test such as contrast sensitivity function is vital.Given these findings,patients with SS are encouraged to undergo regular eye examinations and ensure their vision is fully corrected to avoid any visual difficulties, especially in dim conditions.
ACKNOWLEDGEMENTS
The authors would like to extend their sincere appreciation to the Deanship of Scientific Research and Research Center,College of Applied Medical Sciences at King Saud University for funding this work.The authors thank the Deanship of Scientific Research and RSSU at King Saud University for their technical support.
Conflicts of Interest:Alhassan M,None;Aldarwesh A,None;Alessa I,None;Alhijji R,None;Alduhayan R,None;Almustanyir A,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Three-dimensional bioprinting in ophthalmic care
- Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
- A combined treatment for patients with dry eye and associated laryngopharyngeal reflux: a real-life approach
