Time trends in myopia and high myopia prevalence in young university adults in China
Hong-Mei Zhang, Bing-Qin Li, Yun Zhu, Sheng-Xin Liu, Rui-Hua Wei
1Tianjin Key Laboratory of Retinal Functions and Diseases,Tianjin Branch of National Clinical Research Center for Ocular Disease, Eye Institute and School of Optometry, Tianjin Medical University Eye Hospital, Tianjin 300384, China
2Department of Epidemiology and Biostatistics, Tianjin Medical University, Tianjin 300070, China
3Tianjin University of Traditional Chinese Medicine, Tianjin 300193, China
Abstract
● KEYWORDS: myopia; high myopia; prevalence; axial length; time trend
INTRODUCTION
Myopia has become a worldwide public health issue[1-4].The prevalence of children’s myopia has reached an epidemic level in certain areas (Eastern Asia) and still progressing exponentially[5-7].A review predicted that 50%of the world’s population will have myopia by 2050, and 10% will be high myopia[8].Those with myopia are at high risk of a range of conditions, including glaucoma, retinal detachment, and myopic macular degeneration, which will cause irreversible blindness[9-10].
The upward trend in myopia and high myopia prevalence was observed more apparent among children in Eastern Asia.Linet al[11]found the mean prevalence of myopia in children increased dramatically in Taiwan, China.The figures were 5.8%, 36.7%, 64.2%, and 74% for children 7, 12, 15, and 16-18 years old in 1983.They soared to 21%, 61%, 81%, and 84%correspondingly in 2000.Meanwhile, the prevalence of high myopia increased from 10.9% to 21% of 18-year-old students.In Japan, the frequencies of myopia in a general Japanese population aged 40y and older increased significantly from 2005 to 2017 (myopia: 37.7% to 45.8%; high myopia: 5.8% to 9.5%)[12].
However, there was a gap in the literature.The study participants were limited to children below 18 years old who had a high prevalence rate of myopia, or elderly individuals who had a high prevalence rate of myopic maculopathy.There have been limited studies examining trends in the prevalence of myopia and high myopia in young adults.To address this issue, the purpose of this study was to investigate time trends in the prevalence of myopia and high myopia, and the ocular biometry parameters over 6y among young adults at a medical university in China.
SUBJECTS AND METHODS
Ethical ApprovalThis study was conducted under the approval of the authorities and ethics committee of Tianjin Medical University Eye Hospital (No.2021KY-16) and adhered to the tenets of the Declaration of Helsinki.Informed consent was obtained from the subjects after an explanation of the nature and possible consequences of the study.
Study ParticipantsTo further protect their health, all freshmen in China were required to take the university admission medical examination.Height, weight, blood pressure, heart rate, visual acuity, ear, nose and throat examination, and general medical examination are all part of the evaluation.Our Tianjin Medical University Eye Study paralleled this medical examination.We conducted this series of cross-sectional studies from 2016 to 2021.The survey was missed in 2019 when we were conducting the follow-up study of students enrolled in 2016.We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)reporting guidelines.
We excluded students who had eye diseases, eye surgeries including refractive surgery, orthokeratology lenses within one month, and other systematic diseases.In total, 1018 students in 2016, 946 students in 2017, 1068 students in 2018, 941 students in 2020, and 937 students in 2021 were enrolled and their data were analyzed.
Eye ExaminationsEye examinations were performed similarly each year.All participants completed a questionnaire concerning age, gender, eye or systematic disease history, and family disease history.Eye examinations were performed by an experienced ophthalmologist using a slit-lamp examination(model YZ5X1; 66 Vision Tech Co., Ltd., Suzhou, China),other examinations including non-cycloplegic autorefraction(model KR 8900; Topcon, Tokyo, Japan), lensmeter (model CL-300; Topcon, Tokyo, Japan) and ocular biometrics measurement [axial length (AL) and cornea radius (CR)] with Lenstar (LS-900; Haag-Streit AG, Switzerland) were done by trained optometry students.All machine results were conducted three times to avoid bias and averaged values were recorded.Our protocol was reported in other published articles[13].
DefinitionRefractive errors were classified according to the spherical equivalent (SE=sphere+0.5×cylinder) of noncycloplegic autorefraction.Myopia was defined as SE ≤-0.5 diopters (D), and high myopia was defined as SE ≤-6.00 D.The mean corneal radius (CR) equals (CRflat+ CRsteep)/2.The ratio of the mean of AL and CR was AL/CR.
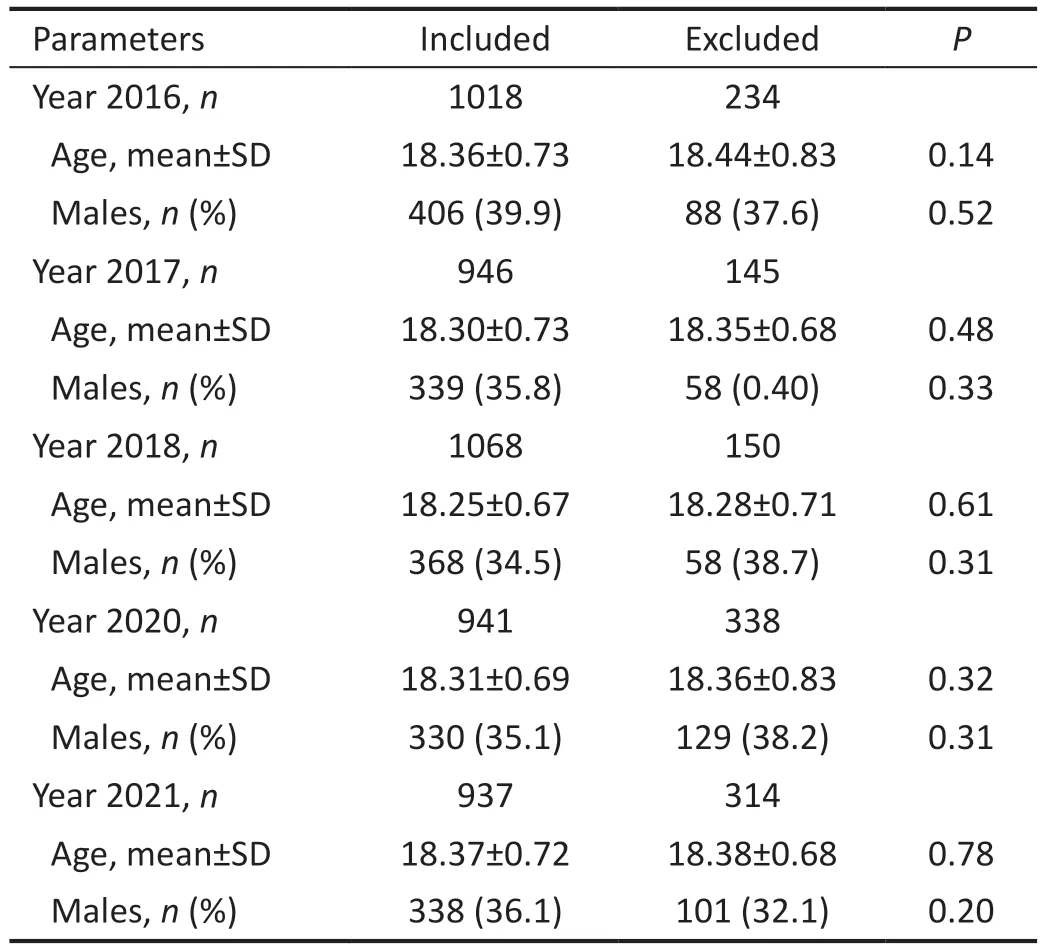
Table 1 Comparison of subjects included in and excluded from data analyses by age, gender
Statistical AnalysisContinuous variables were expressed as means (standard deviation, SD).For categorical variables,counts and proportions were presented.We used independentt-tests to compare quantitative variables andχ2tests to compare categorial.Time trend analyses of the general prevalence of myopia and high myopia were conducted using theχ2trend test, and ANOVA trend tests were conducted for continuous variables.Only the result of the right eye was used to analyze because there was a high correlation coefficient between the two eyes (r≥0.88,P<0.01).The level of significance was set as a 2-sidedP-value less than 0.05.All statistical analyses were conducted with SPSS version 23.0 (SPSS Inc., USA).
RESULTS
In Table 1, we compared the characteristics of included students with excluded students.There were no significant differences in age and gender distribution between students included and excluded (independentt-test orχ2test as appropriate,P≥0.14).
Table 2 shows the changes in characteristics among young university adults from 2016 to 2021.The mean SE of the 4910 eligible participants was -4.37±2.58 D, and the mean AL was 25.29±1.26 mm.There were no significant differences in age(P=0.67 for trend) and gender distribution (P=0.09 for trend)among the 6-year studies.The changes in the mean SE among the 6-year studies were not significant (P=0.59 for trend)neither in males (P=0.60 for trend) nor females (P=0.71 for trend).However, the AL increased significantly among the 6-year studies (P=0.002 for trend), both in males (P=0.001 for trend) and females (P=0.04 for trend).The CR increased significantly among the 6-year studies too (P=0.04 for trend),and in females (P=0.005 for trend), but not significantly inmales (P=0.59 for trend).The changes in AL/CR were not significant among the 6-year studies (P=0.24 for trend), and in females (P=0.91 for trend).However, the AL/CR increased significantly in males (P=0.04 for trend).
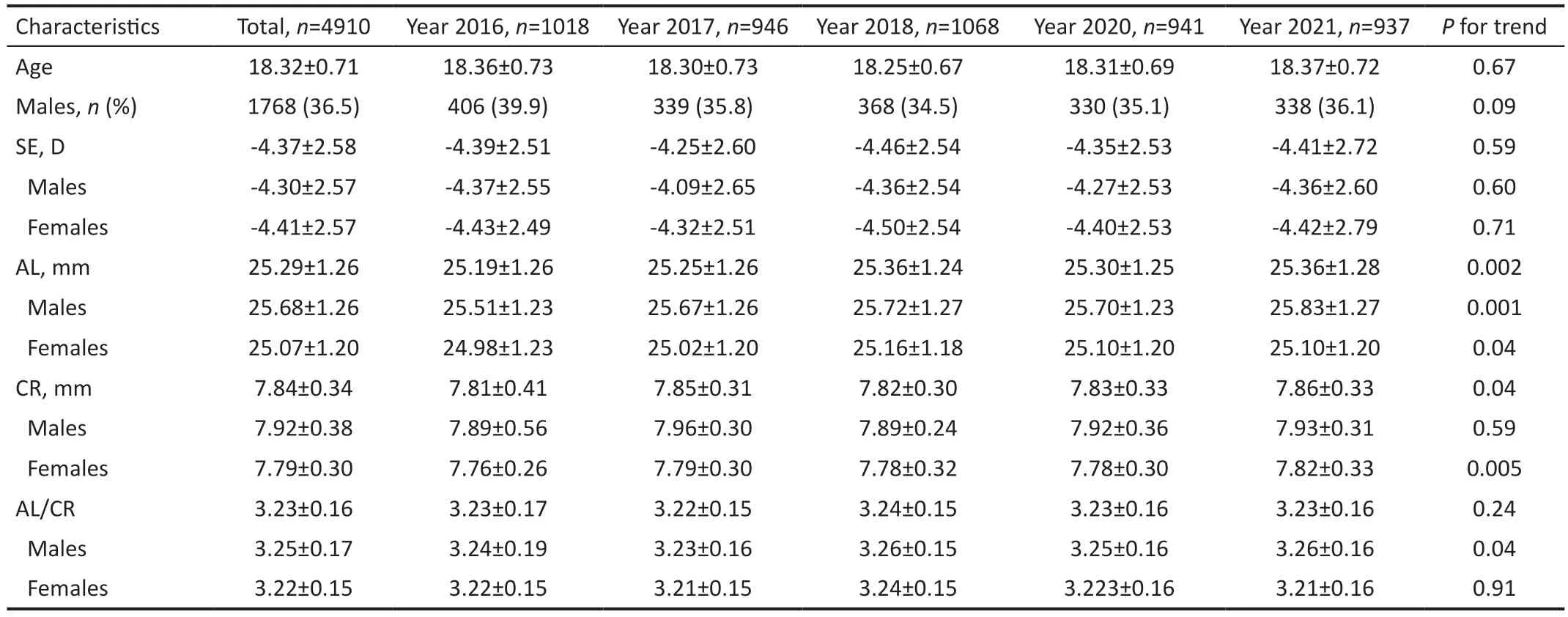
Table 2 The changes in characteristics among young university adults from 2016 to 2021 mean±SD

Table 3 Time trends in myopia and high myopia prevalence from 2016 to 2021 among young university adults n (%)
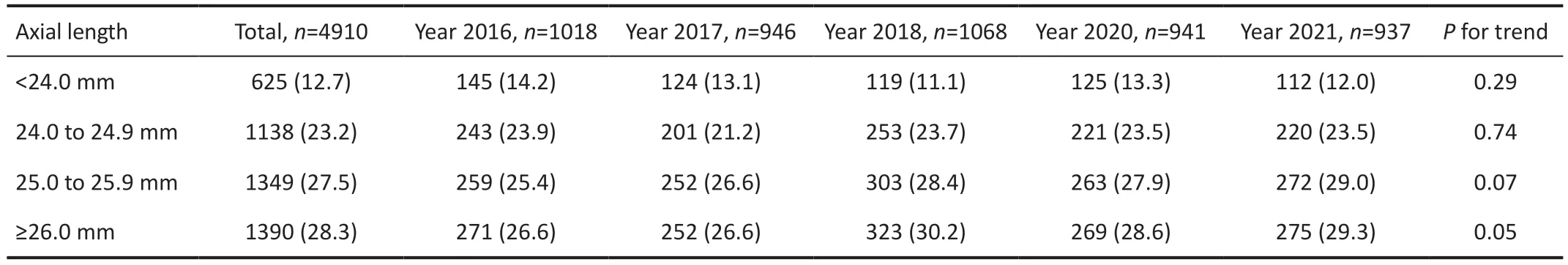
Table 4 Time trends in the frequencies of axial length from 2016 to 2021 among young university adults n (%)
Time trends in myopia and high myopia prevalence from 2016 to 2021 among young university adults are shown in Table 3.The total prevalence of myopia and high myopia was 92.9%,and 25.5%, respectively.The prevalence of myopia and high myopia did not change significantly in total or males from 2016 to 2021 (allP≥0.18 for trend).In females, the prevalence of myopia decreased significantly (P=0.04 for trend); the prevalence of high myopia did not increase significantly(P=0.08 for trend).
Time trends in myopia and high myopia prevalence from 2016 to 2021 among young university adults are shown in Figure 1.
The prevalence of myopia remained steady from 2016 to 2021 overall, in both males and females.
Table 4 shows the time trends in the frequencies of AL from 2016 to 2021.The frequency of AL levels of less than 24 mm, 24.0 to 24.9 mm, and 25.0 to 25.9 mm did not change significantly from 2016 to 2021 (Pfor trend ≥0.07).TheP-value was borderline in the AL≥ 26.0 mm group (P=0.05 for trend), which means the frequencies of the AL≥ 26.0 mm group increased significantly (from 26.6% in 2016 to 29.3% in 2021).

Figure 1 Time trends in myopia and high myopia prevalence from 2016 to 2021 among young university adults.

Table 5 Comparison of the study conducted in 2012 and the current study in 2021
Table 5 shows the comparison of our study to a similar population of university students in 2012 at Donghua University, Shanghai, China.The data were gathered using the same non-cycloplegic auto-refraction, and the same cutoff value for myopia and high myopia.The age distribution D: Diopter; High myopia: SE≤-6.00 D; Myopia: SE≤-0.50 D;n: Sample size; SE: Spherical equivalent.was similar, the proportion of males was lower slightly in our current study compared with the study conducted in 2012(36.1%vs42.3%).The mean SE was higher (-4.41±2.72 Dvs-3.97±2.40 D,P<0.001) in our study.The prevalence of myopia decreased (94.9%vs91.8%,P<0.001).However,the prevalence of high myopia increased largely (18.12%vs27.6%,P<0.001).
DISCUSSION
In our 6-year series cross-sectional study, we found that myopia and high myopia prevalence did not increase significantly in young university adults from 2016 to 2021.But we observed an upward trend in the frequency of AL≥26.0 mm increased over time.Compared with a similar study conducted 10 years ago, the prevalence of high myopia increased largely in young university adults.This upwards trend in young university adults suggested that myopia control treatments are still needed even in young adulthood to prevent high myopia.Multiple cross-sectional studies at different time points in different counties showed that the prevalence of myopia among school children increased over time[6,11,14-15].In school children,from 2006 to 2015, a study reported that the prevalence of myopia in Beijing increased from 55.95% to 65.48%[16].There have been only a few epidemiologic studies addressing the trend in myopia among young adults[17-18].Of these, Bar Dayanet al[19]found the prevalence of myopia increased from 20.3%in 1990 to 28.3% in 2002 among Israeli young adults.The prevalence of myopia over 6 decades (from the 1920s to the 1980s) in Chinese adults in Singapore surged from 36.4% to 85.9%[20].Chenet al[21]reported that the prevalence of myopia increased from 79.5% to 87.7% from 2001 to 2015 among high school students in Fenghua City, eastern China.
In contrast, the prevalence of myopia was relatively steady among our young adults aged 18.37 years old.Someone may say that the 6y of observation time was relatively short in our study.Even so, the prevalence of myopia did not significantly increase (94.9%vs91.8%) when comparing our study with a study of a similar nature after extending the observation period to 10y[22].Similarly, Lamet al[23]reported that the prevalence of myopia for ages 6-12y remained unchanged over the last two decades in Hong Kong.We speculated that there is a small proportion of the population that is genetically incapable of starting on the myopia processes, and others may be protected by their healthy lifestyles that include high levels of outdoor time.The prevalence of myopia may have already reached its highest capacity in young university adults.
The prevalence of high myopia increased from 24.6% to 27.6%, especially in females, from 23.7% to 29.2% in our study, though insignificant.When comparing our study with a study 10y ago, the prevalence of high myopia increased largely (18.12%vs27.6%).The lifestyle changed largely during these 10y in China.The increasing use of electronic products, the COVID-19 pandemic, online teaching,insufficient outdoor activity,etc.These factors may cause young adults with mild myopia or moderate myopia to progress to high myopia.Chenet al[21]reported the prevalence of high myopia increased from 7.9% to 16.6% among 43 858 third-year high school students.The rising frequency of high myopia suggests that preventive and rescue treatments for high myopia are critical for young adults[10,24-25].The government should target different preventive measures for different populations[26], such as increasing outdoor time in children to prevent early-onset myopia; using a low concentration of atropine eye drops or other newly designed contact lenses to slow myopia progression from mild to high myopia; and using measures to treat complications from high to pathologic myopia[9].
The ratio of AL to CR defined the refractive state[27].When compared to AL alone, the AL/CR ratio has a stronger correlation with SE[28].This was also true in our investigation.Despite increasing mean AL and CR, the combination of longer AL and flatter CR resulted in a steady SE.The mean SE changed insignificantly over time.Generally, high myopia was defined as AL≥26.0 mm or SE<-6.00 D[29].In our study,we found the frequency of AL≥26.0 mm increased with time,though theP-value was at the borderline.These findings confirmed the prevalence of high myopia has grown from another angle.
The main strength of this study is that the cross-sectional data at a 5-time point covered 4910 university young adults,resulting in large amounts of data on the changing trend of myopia and high myopia prevalence, as well as the mean SE and AL.Non-cycloplegia in our analysis is a major limitation.Studies reported that non-cycloplegic auto-refraction may result in a slight overestimation of myopia even in young adults[30].So, overestimation of the prevalence of myopia and high myopia is still a concern.However, considering that the same protocol was followed each year, this will not likely markedly affect the trend.Second, these estimates on university young adults cannot be broadly applied to the general population and may have implications for policymaking for young adults.Third, over relatively short periods of study, it showed no statistical difference in the prevalence of myopia and high myopia in young adults.However, comparing our study with others conducted 10 years ago, it was found that the prevalence of high myopia increased.Thus, long-term followup should be conducted in the future.
In conclusion, the prevalence of high myopia increased in young university adults.Myopia control should begin earlier in childhood; However, these treatments are still needed for high myopia even in young adulthood.
ACKNOWLEDGEMENTS
We acknowledge all the subjects who participated in the study.Foundations:Supported by China Scholarship Council (CSC;No.202006945002); Chunhui Project of China Education Ministry (No.HZKY20220587); Tianjin Health Technology Research Project (No.TJWJ2022MS014); Tianjin Municipal Education Commission Scientific Research Program (Mental Health Education; No.2022ZDGX20).
Conflicts of Interest:Zhang HM,None;Li BQ,None;Zhu Y,None;Liu SX,None;Wei RH,None.
 International Journal of Ophthalmology2023年10期
International Journal of Ophthalmology2023年10期
- International Journal of Ophthalmology的其它文章
- A novel approach for 25-gauge transconjunctival sutureless vitrectomy to evaluate vitreous substitutes in rabbits
- Visual resolution under photopic and mesopic conditions in patients with Sjögren's syndrome
- Effects of obstructive sleep apnea on retinal microvasculature
- Bibliometric analysis of research relating to refractive cataract surgery over a 20-year period: from 2003 to 2022
- Three-dimensional bioprinting in ophthalmic care
- Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors
