冠状动脉搭桥术后患者认知功能障碍的发生现况及其相关影响因素探讨
马宁 张伟华 孙晓柯 张亮 郭瑞明 徐昊 张新 乔晨晖
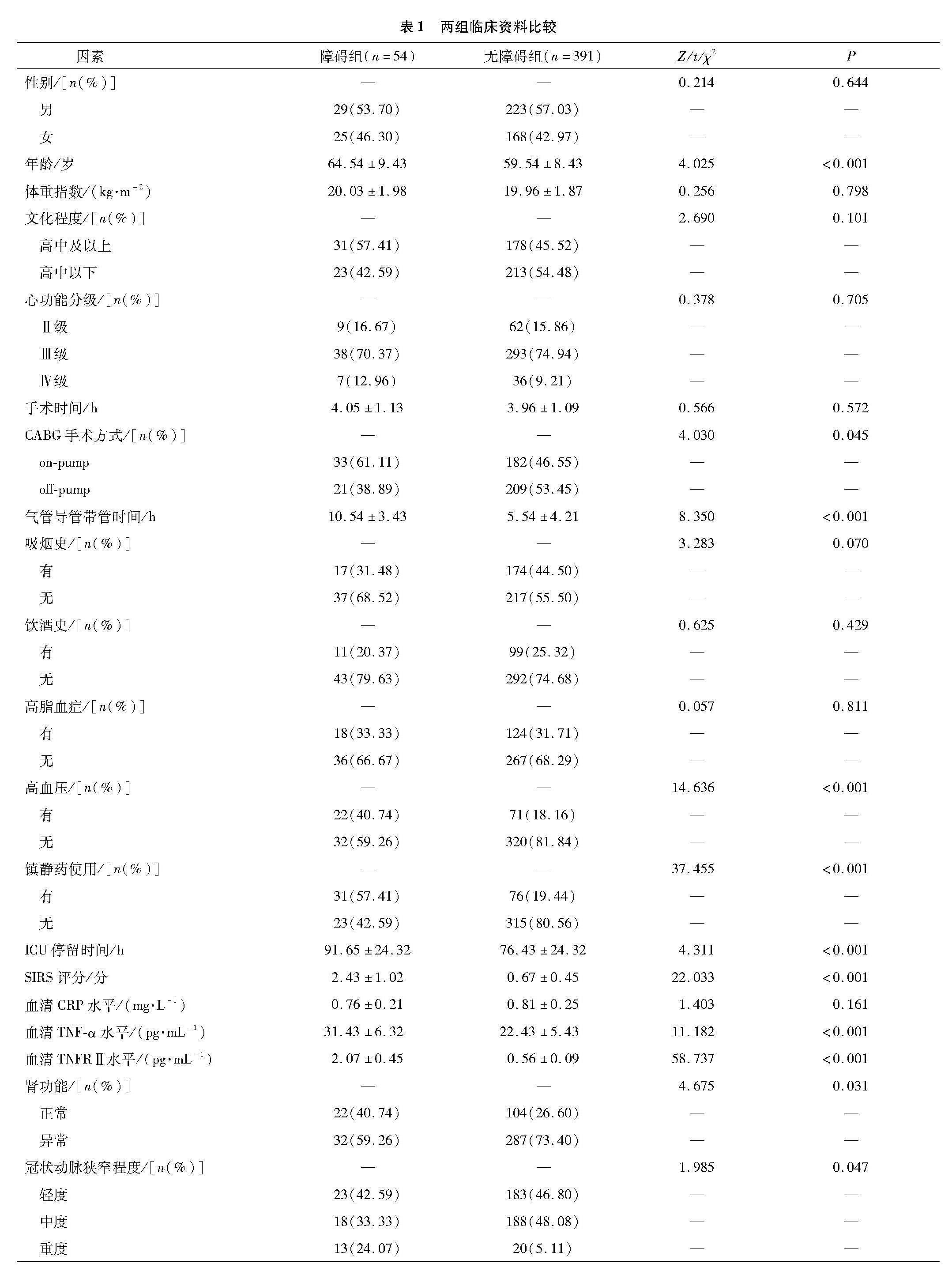
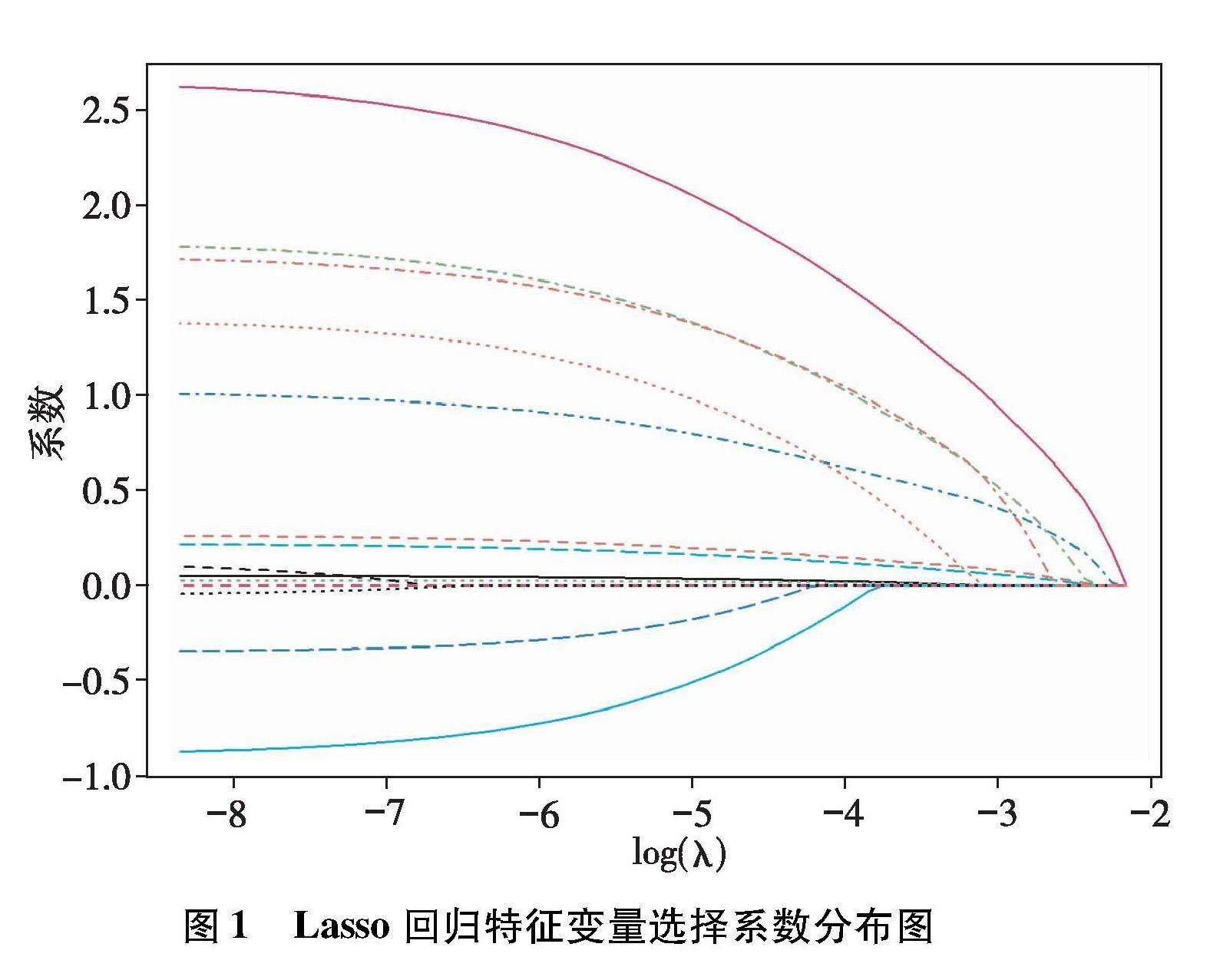

【摘要】目的 探討冠状动脉搭桥术后患者认知功能障碍的发生现况及其相关影响因素。方法 对于2021年1月—2022年12月在郑州大学第一附属医院接受治疗的445例冠状动脉搭桥术后患者临床资料进行回顾性分析,将发生认知功能障碍的患者纳入障碍组[术后第7天采用简易精神状态评价量表评估认知功能,显示评分<27分],无认知功能障碍的患者纳入无障碍组。统计冠状动脉搭桥术后患者认知功能障碍的发生现况,比较两组临床资料,予以Lasso回归分析法分析冠状动脉搭桥术术后患者认知功能障碍的危险因素,并构建预测模型,绘制受试者操作特征曲线分析其对冠状动脉搭桥术后患者认知功能障碍的预测价值。结果 445例冠状动脉搭桥术后患者中有54例简易精神状态评价量表评分<27分,认知功能障碍发生率为12.13%。障碍组年龄大于无障碍组;气管导管带管时间、加强监护病房停留时间长于无障碍组;On-pump术、有高血压、镇静药物使用、肾功能异常、重度冠状动脉狭窄的患者占比分别为61.11%、40.74%、57.41%、59.26%、24.07%,均高于无障碍组的46.55%、18.16%、19.44%、26.60%、5.11%;全身炎症反应综合征评分、血清肿瘤坏死因子-α、肿瘤坏死因子受体Ⅱ水平高于无障碍组(P<0.05)。Lasso回归分析结果显示,年龄大、加强监护病房停留时间长、有高血压、全身炎症反应综合征评分高、血清肿瘤坏死因子-α水平高以及冠状动脉狭窄程度为重度均是冠状动脉搭桥术后患者认知功能障碍的独立危险因素。回归方程模型:logit(P)=-15.827+年龄×0.07+加强监护病房停留时间×0.024+有无高血压×1.586+全身炎症反应综合征评分×1.126+血清肿瘤坏死因子-α水平×0.16-冠状动脉狭窄程度中度×0.238+冠状动脉狭窄程度重度×1.631。受试者操作特征曲线分析显示,当logit(P)>0.16时,曲线下面积为0.873,95%CI为0.814~0.933,诊断敏感度为74.07%,特异度为88.00%。结论 冠状动脉搭桥术术后患者认知功能障碍的风险较高,其独立危险因素包括年龄大、加强监护病房停留时间长、有高血压、全身炎症反应综合征评分高、血清肿瘤坏死因子-α水平高以及冠状动脉狭窄程度为重度,根据其构建回归模型的预测价值较高,临床可据此给予针对性的预防及治疗措施。
【关键词】冠状动脉搭桥术;认知功能障碍;影响因素;预测模型
【DOI】10.16806/j.cnki.issn.1004-3934.2023.12.000
Current Status and Related Influencing Factors of Cognitive Impairment in Patients After Coronary Artery Bypass Grafting Surgery
MA Ning,ZHANG Weihua,SUN Xiaoke,ZHANG Liang,GUO Ruiming,XU Hao,ZHANG Xin,QIAO Chenhui
(Department of Cardiovascular Surgery,The First Affiliated Hospital of Zhengzhou University,Zhengzhou 450052,Henan,China)
【Abstract】Objective To explore the current status and related influencing factors of cognitive impairment in patients after coronary artery bypass grafting. Methods The clinical data of 445 patients after coronary artery bypass grafting admitted to The First Affiliated Hospital of Zhengzhou University from January 2021 to December 2022 were retrospectively analyzed. Patients with cognitive impairment were included in the obstacle group [on the 7 th postoperative day,cognitive function was evaluated using the simplified mental state assessment scale ,with a score of<27 points],while patients without cognitive impairment were included in the non obstacle group. The current status of cognitive dysfunction in patients after coronary artery bypass grafting was analyzed,the clinical data of two groups were compared,the risk factors of cognitive dysfunction in patients after coronary artery bypass grafting was analyzed by Lasso regression analysis,and constructed a predictive model,and its predictive value for cognitive dysfunction in patients after coronary artery bypass grafting analyzed by the receiver operating characteristic curve. Results Among 445 patients after coronary artery bypass grafting,54 had a score of simplified mental state assessment scale<27,and the incidence of cognitive impairment was 12.13%. The age of the disabled group was greater than that of the non obstacle group; The times of duration of tracheal intubation and intensive care unit stay were longer than those in the non obstacle group; The proportion of patients with on pump surgery,hypertension,sedative drug use,renal dysfunction,and severe coronary stenosis was 61.11%,40.74%,57.41%,59.26% and 24.07%,respectively,which were higher than 46.55%,18.16%,19.44%,26.60% and 5.11% in the non obstacle group; the score of postoperative systemic inflammatory response syndrome,levels of serum tumor necrosis factor-α,tumor necrosis factor receptor Ⅱ were higher than that of the non obstacle group (P<0.05). The results of Lasso regression analysis showed that older age,longer intensive care unit stay,hypertension,high score of systemic inflammatory response syndrome,high levels of serum tumor necrosis factor-α and severity of coronary stenosis were independent risk factors for cognitive impairment in patients after coronary artery bypass grafting surgery. The regression equation model:logit (P)=﹣15.827+age × 0.07+time of intensive care unit stay × 0.024+with or without hypertension × 1.586+score of systemic inflammatory response syndrome × 1.126+level of serum tumor necrosis factor-α × 0.16-moderate degree of coronary stenosis × 0.238+severe degree of coronary stenosis × 1.631. receiver operating characteristic curve analysis showed that when logit(P)>0.16,the AUC value was 0.873,with a 95% CI of 0.814~0.933,the diagnostic sensitivity was 74.07%,and the specificity was 88.00%. Conclusion The risk of cognitive impairment in patients after coronary artery bypass grafting was higher,and the independent risk factors included older age,longer stay in intensive care unit, high blood pressure,high score of systemic inflammatory response syndrome, high level of serum tumor necrosis factor-α, and severe coronary stenosis, the predictive value of constructing regression models based on it was high, and targeted prevention and treatment measures could be given in clinical practice.
【Key words】Coronary artery bypass graft; Cognitive impairment; Influencing factors; Prediction model
冠状动脉搭桥术(coronary artery bypass graft,CABG)可以為缺血的心肌组织重新构建血液通道,使血氧供给得以恢复,能够有效缓解相关临床症状[1]。随着生物-心理-社会医学模式的深入研究,对认知、心理状态的重视度逐渐提高,研究[2]发现认知功能障碍是CABG常见的并发症,主要表现为注意力降低、记忆减退等,会延长CABG术后患者住院时间,增加治疗费用,且会增加手术死亡率。因此有效分析CABG术后患者认知功能障碍的相关影响因素对改善患者生活质量具有重要意义。目前临床研究[3-4]认为认知功能障碍是多因素引起的疾病,但目前国内外关于认知功能障碍在CABG术后发生的危险因素尚无统一定论。基于此,本研究对445例CABG术后患者临床资料进行回顾性分析,旨在探讨CABG术后认知功能障碍的有效防治措施,现将本研究整理如下。
1 资料与方法
1.1 一般资料
对2021年1月—2022年12月在郑州大学第一附属医院接受治疗的445例CABG术后患者临床资料进行回顾性分析,将发生认知功能障碍的54例患者纳入障碍组,无认知功能障碍的391例患者纳入无障碍组,表1为两组具体的一般资料。郑州大学第一附属医院医学研究伦理委员会已对本研究试验设计进行审核(编号:2020-KS-HNSR163),并予以批准。
1.2 纳入、排除及剔除标准
1.2.1 纳入标准
符合CABG指征者;术前认知功能正常者;经CABG治疗后心绞痛、心功能障碍等得到有效缓解,血管狭窄程度有明显改善者;临床资料完整者等。
1.2.2 排除标准
合并其他心血管疾病需要同期手术治疗者;既往有脑部疾病史者;服用抗抑郁药物或镇静药物者;既往有脑血管意外或短暂性脑缺血者;同时参与其他试验研究者等。
1.2.3 剔除标准 误纳入者。
1.3 研究方法与观察指标
1.3.1 CABG术后患者认知功能障碍的发生现况
术后第7天采用简易精神状态评价量表评分[5]对患者认知功能进行评估,该量表共30题,每题0~1分,总分为30分,小于27分为认知功能障碍,统计认知功能障碍的发生率。
1.3.2 临床资料收集
根据郑州大学第一附属医院门诊及电子病历系统,收集两组基本情况[年龄、性别、体重指数及文化程度]、心功能分级[6]、手术时间、CABG手术方式(on-pump,off-pump)、气管导管带管时间、有无吸烟史、饮酒史、高脂血症、高血压、镇静药物使用、加强监护病房(intensive care unit,ICU)停留时间、术后全身炎症反应综合征(systemic inflammatory response syndrome,SIRS)评分[7](总分4分,分值越高,机体炎症反应越重)、血清C反应蛋白(C-reactive protein,CRP)、肿瘤坏死因子-α(tumor necrosis factor-α,TNF-α)、肿瘤坏死因子受体Ⅱ(tumor necrosis factor receptor Ⅱ,TNFRⅡ)水平、肾功能、冠状动脉狭窄程度(轻度:狭窄程度<50%;中度:狭窄程度为50%~75%;重度:狭窄程度>75%)等临床资料。所有患者入组后,抽取空腹静脉血3 mL,分离血清后(3 500 r/min,10 min),采用全自动生化分析仪[长沙芯生医疗科技有限公司(全自动生化分析仪,BI60)]检测血清CRP、TNF-α、TNFRⅡ水平。
1.4 统计学方法
本研究统计数据使用软件为SPSS 21.0。计数资料及符合正态分布的计量资料分别以n(%)、(±s)表示,组间比较分别予以χ2检验及独立样本t检验,采用秩和检验对等级资料进行比较。采用R4.3.1软件“glmnet”软件包构建lasso回归进行变量筛选。lasso回归引入了L1范数正则化构建一个惩罚项,通过控制调节系数λ的变化对回归系数进行惩罚,将不重要的回归系数压缩到0,可缓解模型过拟合的问题。通过10折交叉验证选择最优λ值,lambda.min或者lambda.1se。在lasso回归的基础上,采用“rms”软件包进行多因素logistic回归对CABG术后患者认知功能障碍的危险因素进行分析。采用Hosmer-Lemeshow检验模型拟合度,当P>0.05,则说明模型的准确度好;采用“pROC”软件包绘制受试者操作特征(receiver operator characteristic,ROC)曲线获取曲线下面积(area under the curve,AUC),评估预测模型的区分度,应用校准曲线分析CABG术后患者认知功能障碍的校准度。差异有统计学意义用P<0.05进行表示。认知功能障碍及可能影响因素赋值为1,无认知功能障碍及其他因素赋值为0。
2 结果
2.1 CABG术后患者认知功能障碍的发生现况
445例CABG术后患者中有54例简易精神状态评价量表评分<27分,认知功能障碍发生率为12.13%。
2.2 两组临床资料比较
障碍组年龄大于无障碍组,气管导管带管时间、ICU停留时间长于无障碍组;on-pump术、有高血压、镇静药物使用、肾功能异常、重度冠状动脉狭窄的患者占比分别为61.11%、40.74%、57.41%、59.26%、24.07%,均高于无障碍组的46.55%、18.16%、19.44%、26.60%、5.11%;SIRS评分、血清TNF-α、TNFRⅡ水平高于无障碍组(P<0.05),而比较两组性别、体重指数、文化程度、心功能分级、手术时间、有无吸烟史、饮酒史、高脂血症、血清CRP水平等结果显示,P>0.05,显示无统计学差异。见表1。
2.3 lasso回归筛选预测变量
将表1中障碍组和无障碍组比较P<0.1的12个变量纳入lasso回归模型,将冠状动脉狭窄程度进行亚组分析,共纳入14个变量进入lasso回归模型。lasso回歸系数分布图显示,随着横坐标惩罚系数λ的增加,纵坐标变量系数在惩罚项下不断被压缩为0(图1);结合lasso回归10折交叉验证图,本次模型选择lambda.min=0.0044为最佳λ值,共筛选出11个非零系数特征的变量(图2),即年龄、气管导管带管时间、ICU停留时间、SIRS评分、血清TNF-α水平、血清TNFRⅡ水平、有无高血压、有无镇静药物使用、GABG手术方式、肾功能、冠状动脉狭窄程度中度和冠状动脉狭窄程度重度。
2.4 CABG术后患者认知功能障碍的危险因素分析
将lasso回归筛选出来的11个变量作为自变量,以是否发生认知功能障碍为因变量进行向前极大似然法,结果显示,年龄大、ICU停留时间长、有高血压、SIRS评分高、血清TNF-α水平高以及冠状动脉狭窄程度为重度均是CABG术后患者认知功能障碍的独立危险因素。见表2。
2.5 预测模型的构建及评价
logistic回归方程模型:logit(P)=-15.827+年龄×0.07+ICU停留时间×0.024+有无高血压×1.586+SIRS评分×1.126+血清TNF-α水平×0.16-冠状动脉狭窄程度中度×0.238+冠状动脉狭窄程度重度×1.631。采用Hosmer-Lemeshow拟合优度检验显示模型拟合效果较好,DF=11,Chi-Square=7.616,P=0.482,模型拟合的准确度较好。通过校准曲线显示,认知功能障碍预测概率与实际概率接近,提示该预测模型具有良好的区分、校准和预测能力(图3)。模型的内部验证采用ROC曲线进行检验。当logit(P)>0.16时,AUC值为0.873,95%CI为0.814~0.933,诊断敏感度为74.07%,特异度为88.00%。见图4。
3 讨论
接受CABG的患者多为中老年患者,且手术时间较长,术后并发认知功能障碍的风险较高[8]。本研究发现,CABG术后患者认知功能障碍的发生率为12.13%,略低于其他学者的研究结果(23.64%)[9],分析其原因可能为,目前CABG治疗的患者越来越年轻化,而年龄小的患者认知功能障碍的风险相对较小,故而导致本研究中认知功能障碍发生风险相对较低。研究[10]显示,认知功能障碍患者病情好转后仍有部分会遗留精神障碍,而目前其发病机制尚无统一定论,故而分析其危险因素,有助于预测认知功能障碍发生的风险性。
本研究结果提示了CABG术后患者认知功能障碍的发生可能与年龄、气管导管带管时间、ICU停留时间、手术方式、有无高血压、镇静药物使用、SIRS评分及血清TNF-α、TNFRⅡ水平、肾功能及冠状动脉狭窄程度等因素有关。分析其原因可能为,随着年龄升高,CABG术后患者脑组织逐渐退化,神经元能量供给减少,且手术治疗会给机体造成较大的损伤,诱发认知功能障碍的风险较高[11]。气管插管、呼吸机等刺激会给患者带来一定的精神压力,且ICU患者普遍存在睡眠-觉醒节律紊乱,因此,气管导管带管时间、ICU停留时间长的CABG术后患者认知功能障碍的风险较高[12]。而on-pump手术中体外循环心肺转流的应用会导致CABG术后患者大脑氧代谢异常、微栓塞及全身炎症反应等,进一步会对患者中枢神经系统造成损害,增加了认知功能障碍的风险,但与其他学者[13]的研究结果有所差异,可能与样本量、个体差异等因素有关。有高血压的CABG术后患者往往伴有脑血管硬化及颈动脉粥样斑块,而脑供血更依赖于较高灌注压,手术治疗过程中低血压易引起脑供血不足而引发脑神经功能障碍,增加了认知功能障碍的风险[14]。有镇静药物使用的CABG术后患者在药物的作用下,会出现记忆力下降、反应迟钝等情况,会影响患者的认知功能[15-16]。SIRS评分、血清TNF-α、TNFRⅡ水平均高的CABG术后患者全身性炎症反应较重,而炎症反应释放的多种因子与认知功能障碍的发生具有密切关系[17-18]。肾功能与冠状动脉狭窄程度对CABG术后患者认知功能障碍的影响的相关研究仍较少,分析可能为,肾功能异常可能导致毒素和水分聚集在患者体内,引起各个系统和组织的功能异常,若聚集在神经系统时,容易导致脑部器官、细胞异常,从而增加了认知功能障碍的风险。重度冠状动脉狭窄的患者CABG术后病情较严重,而心血管疾病是认知功能障碍的危险因素。
本研究还发现,年龄大、ICU停留时间长、有高血压、SIRS评分高、血清TNF-α水平高以及冠状动脉狭窄程度为重度均是CABG术后患者认知功能障碍的独立危险因素,据此构建回归方程模型,预测CABG术后患者认知功能障碍的ROC曲线AUC值为0.873,诊断敏感度为74.07%,特异度为88.00%。因此,临床可据此给予相关高危患者针对性的干预措施以减少认知功能障碍的发生,针对年龄大的患者在术前要加强治疗,积极改善心肺功能,且在术中要注意保护器官功能状态[19];ICU停留时间长的患者可通过非药物干预的方式为患者建立昼夜节律,并为患者营造一个舒适的睡眠环境[20];同时对于有高血压的患者严格,要积极通过药物治疗控制血压;密切监测炎症指标变化情况,SIRS评分、血清TNF-α水平均高提示机体炎症反应的患者要积极控制炎症反应,进一步减少或避免CABG术后认知功能障碍的发生。
综上,CABG术后患者认知功能障碍的风险较高,其独立危险因素包括年龄大、ICU停留时间长、有高血压、SIRS评分高、血清TNF-α水平高以及冠状动脉狭窄程度为重度,根据其构建回归模型的预测价值较高,临床可据此给予针对性的预防及治疗措施。但本研究结果可能因研究样本量少、仅为单中心研究等不足之处而有一定的偏倚存在,故而进一步提高研究结果的可靠性,以期临床进一步纳入更多样本量,进行多中心研究。
參 考 文 献
[1]Mortensen M,Sandvik RKNM,Svendsen ?S,et al. Return to work after coronary artery bypass grafting and aortic valve replacement surgery:a scoping review[J]. Scand J Caring Sci,2022,36(4):893-909.
[2]Shaefi S,Mittel A,Loberman D,et al. Off-pump versus on-pump coronary artery bypass grafting-a systematic review and analysis of clinical outcomes[J]. J Cardiothorac Vasc Anesth,2019,33(1):232-244.
[3]Une D,Sakaguchi T. Initiation and modification of minimally invasive coronary artery bypass grafting[J]. Gen Thorac Cardiovasc Surg,2019,67(4):349-354.
[4]Song W,Peng D,Lu L,et al. Effect of cognitive dysfunction on the outcome of coronary artery bypass grafting in patients[J]. Panminerva Med,2023,65(2):267-268.
[5]Aiello EN,Pasotti F,Appollonio I,et al. Trajectories of MMSE and MoCA scores across the healthy adult lifespan in the Italian population[J]. Aging Clin Exp Res,2022,34(10):2417-2420.
[6]Gong Z,Li J,Zhong Y,et al. Effects of dexmedetomidine on postoperative cognitive function in patients undergoing coronary artery bypass grafting[J]. Exp Ther Med,2018,16(6):4685-4689.
[7]Oldham MA,Hawkins KA,Lin IH,et al. Depression predicts delirium after coronary artery bypass graft surgery independent of cognitive impairment and cerebrovascular disease:an analysis of the neuropsychiatric outcomes after heart surgery study[J]. Am J Geriatr Psychiatry,2019,27(5):476-486.
[8]Tarasova IV,Trubnikova OA,Syrova ID,et al. Long-term neurophysiological outcomes in patients undergoing coronary artery bypass grafting[J]. Braz J Cardiovasc Surg,2021,36(5):629-638.
[9]Sokolova NY,Golukhova EZ,Savelyeva EA,et al. The state of cognitive function in patients with stable coronary artery disease after coronary artery bypass grafting[J]. Kardiologiia,2021,61(9):40-46.
[10]Kehler DS,Arora RC. Commentary:does a "less is more" approach reduce delirium in patients undergoing coronary artery bypass grafting[J]. J Thorac Cardiovasc Surg,2021,161(4):1285-1286.
[11]Whitlock EL,Diaz-Ramirez LG,Smith AK,et al. Association of coronary artery bypass grafting vs percutaneous coronary intervention with memory decline in older adults undergoing coronary revascularization[J]. JAMA,2021,325(19):1955-1964.
[12]Zhao E,Lowres N,Woolaston A,et al. Prevalence and patterns of cognitive impairment in acute coronary syndrome patients:a systematic review[J]. Eur J Prev Cardiol,2020,27(3):284-293.
[13]Yuan SM,Lin H. Postoperative cognitive dysfunction after coronary artery bypass grafting[J]. Braz J Cardiovasc Surg,2019,34(1):76-84.
[14]Wiberg S,Holmgaard F,Zetterberg H,et al. Biomarkers of cerebral injury for prediction of postoperative cognitive dysfunction in patients undergoing cardiac surgery[J]. J Cardiothorac Vasc Anesth,2022,36(1):125-132.
[15]Pérez-Belmonte LM,Florido-Santiago M,Osuna-Sánchez J,et al. Screening versus brief domain-specific tests to assess long-term postoperative cognitive dysfunction after concomitant aortic valve replacement and coronary artery bypass grafting[J]. J Cardiovasc Nurs,2019,34(6):511-516.
[16]Soliman R,Saad D,Abukhudair W,et al. The neurocognitive outcomes of hemodilution in adult patients undergoing coronary artery bypass grafting using cardiopulmonary bypass[J]. Ann Card Anaesth,2022,25(2):133-140.
[17]Shi Y,Wang W. Application of different anesthetic methods in coronary artery bypass grafting and the effect on postoperative outcome[J]. Exp Ther Med,2019,17(1):695-700.
[18]Chan CK,Neufeld KJ. Commentary on "depression predicts delirium after coronary artery bypass graft surgery independent of cognitive impairment and cerebrovascular disease:an analysis of the neuropsychiatric outcomes after heart surgery study"[J]. Am J Geriatr Psychiatry,2019,27(5):487-489.
[19]Szwed K,Pawliszak W,Szwed M,et al. Reducing delirium and cognitive dysfunction after off-pump coronary bypass:a randomized trial[J]. J Thorac Cardiovasc Surg,2021,161(4):1275-1282.
[20]Semrau JS,Scott SH,Hamilton AG,et al. Quantified pre-operative neurological dysfunction predicts outcome after coronary artery bypass surgery[J]. Aging Clin Exp Res,2020,32(2):289-297.
收稿日期:2023-09-18