Predictors of readiness for discharge in mothers of preterm infants: The role of stress,self-efficacy and perceived social support
Sedighe Valipour, Fatemeh Estebsari, Maliheh Nasiri, Parvaneh Vasli✉
1Department of Community Health Nursing, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Department of Basic Sciences, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
ABSTRACT
Objective: To determine the predictive role of stress, self-efficacy,and perceived social support on readiness for discharge in mothers of preterm infants.
Methods: The present cross-sectional, descriptive-analytical study was conducted on 120 mothers of preterm infants admitted to hospitals affiliated to Lorestan University of Medical Sciences,Iran in 2019. Participants were selected by a convenience sampling method and based on inclusion criteria. Data collection tools included the demographic questionnaire of mothers and infants,parent perceptions of their child's hospital discharge, parental stressor scale: neonatal intensive care unit, perceived maternal parenting, and multidimensional scale of perceived social support.Data were analyzed using Pearson correlation and stepwise regression at the significance level of 0.05.
Results: Infant behavior and appearance, situational belief, and family support achieved the highest mean score from parents' stress,self-efficacy, and perceived social support dimensions, respectively.There was a significant relationship between stress, self-efficacy,and perceived social support with readiness for discharge in mothers of preterm infants (P<0.001). The score of mothers' readiness for discharge decreased by 0.07 per 1-point increase in stress score, and the score of readiness for discharge in mothers of preterm infants rose by 0.35 and 0.43, respectively, for a unit increase in the scores of self-efficacy and perceived social support.
Conclusions: Stress, self-efficacy, and perceived social support can be considered as predictors of readiness for discharge in mothers of preterm infants. It is suggested that nurses in neonatal intensive care units provide a better platform for the readiness for discharge in mothers of preterm infants by reducing stressors and increasing maternal self-efficacy and social support.
KEYWORDS: Patient discharge; Stress; Social support; Selfefficacy; Preterm infant; Mother
1. Introduction
Preterm infant refers to a baby who is born before the 37th week of pregnancy or gestation[1]. Preterm infants admitted to the neonatal intensive care unit (NICU) are at risk for chronic medical conditions and often require complex post-discharge care. Such circumstances,most often require emergency visits and readmission. Readiness for discharge is a key factor in discharging infants and families from the hospital as it reduces potential complications[2]. Studies have shown that parental readiness for discharge is significantly associated with infant safety, parental satisfaction, and family physical, emotional,psychological, and social well-being[3]. Readiness for discharge is defined as the acquisition of technical skills, knowledge, emotional comfort, and self-confidence in the care of the infant at the time of discharge[4]. Pre-discharge stress and anxiety are the factors affecting the degree of parental readiness for discharge, which can prevent the safe discharge of the infant and family from the hospital[5].
Parents of infants admitted to the NICU suffer from psychological distress such as anxiety and stress, due to the environmental conditions mentioned above, the monitoring equipment around the infant, and the complexity of care. These distresses contribute to increase in their child's instability and unpredictable health status,impaired parental role, and emotional trauma caused by unexpected and premature birth[6]. In addition, hospital discharge of the infants is also associated with high stress for parents, as they must undertake full responsibility for the care of the infant[3], while they may not yet be ready adequate to identify changes in infant status and medical care[6].
Self-efficacy is another factor that may be related to readiness for discharge. The readiness for discharge contains different variables,one of which is perceived self-efficacy[7]. The more parental selfconfidence and self-efficacy the more cared for the infant and the more prepared they are to discharge, the sooner discharge is made and the better the results will be after discharge[8]. Maternal selfefficacy is defined as parental judgments and beliefs about their ability to play roles in child care[9]. According to Bandura's theory of self-efficacy, mothers with high levels of self-efficacy welcome the new challenge in the process of becoming a mother, and mothers with low self-efficacy and low self-confidence in compliance with the new requirements are experiencing mental and physical fears[10].Parental self-efficacy has two aspects: 1) the specific knowledge of parental behaviors related to child development tasks and 2) the level of parental self-confidence associated with their ability to perform these behaviors[11]. Maternal self-efficacy affects not only the mother's mental health but also the child's mental development[12].Another factor that may be related to maternal readiness for discharge is family stability and social support[5]. Mothers with more social support have reported greater positive feelings and higher self-confidence in infant care[13]. Numerous studies have reported that social support is an important source of adaptation for mothers of preterm infants. Perceived social support is the individual's perception of the love and support of family members, friends, and acquaintances[14].
Due to the importance of concepts such as readiness for discharge,stress, self-efficacy, and perceived social support in mothers of neonates, studies have been conducted on the relationship between these variables. Lutz et al[14] investigated the relationship between parental stress, social support, and mother-child interaction in families with preterm infants. According to the results of this study,information support is a protective and predictive factor in maternal stress[14]. McGowan et al[4] evaluated the relationship between mental health and readiness for mothers of preterm infants. Their results showed that a history of mental disorders, including stress, is a predictor of a mother's perception of her and her infant's health at discharge. Another study reported that maternal stress was associated with her self-efficacy during the one-month postpartum period[10].
The relationship between social support, stress, and postpartum depression was also examined in another study, whose results showed the effect of social support on postpartum depression[15].Schwab-Reese et al[16] examined the leading and mediating role of stress and social support on postpartum maternal mental health symptoms and indicated that the level of postpartum stress and social support was related to depression and anxiety. The results of another study demonstrated that both social support and self-efficacy are significantly related to postpartum depression[17]. Although a number of studies have examined the relationship of some of the variables considered in this study, none have evaluated the relationship of the four variables considered in this study. Therefore, this study was conducted to determine the knowledge gap in Iran and to determine the predictive role of stress, self-efficacy, and perceived social support on readiness for discharge in mothers of preterm infants.
2. Subjects and methods
2.1. Study design
This cross-sectional descriptive-analytical study was performed on mothers of preterm infants admitted to the NICU in 2019 in Iran.
2.2. Participants
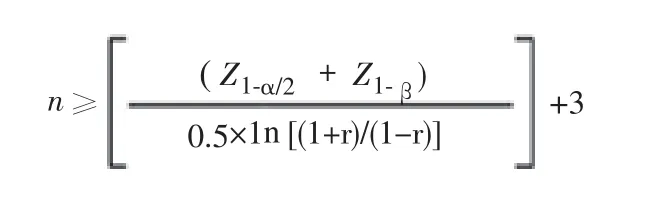
The participants were selected by convenience sampling method from five active NICUs in hospitals affiliated to Lorestan University of Medical Sciences, one of the provinces of Iran. The sample size was estimated to be 120 people considering an error of 5%, test power of 80% and correlation coefficient of 0.3[18], and dropout of 10% according to the following equation:
The inclusion criteria were no specific family life events such as spouse death and divorce, no history of hospitalized infant deaths or previous offspring, no physical illnesses such as hypertension,migraines, severe cardiovascular diseases, multiple sclerosis, etc, no history of infertility and infertility treatments, and vaginal delivery and tendency to get pregnant for a hospitalized newborn.
2.3. Instruments
2.3.1. Demographic characteristics of mothers and infants
The first tool was a questionnaire "demographic characteristics of mothers and infants" with 12 questions including the age of mother and her spouse, educational level of mother and her spouse,occupation of mother and her spouse, number of children, gender of the infant, gestational age, birth weight, parity, and duration of hospitalization.
2.3.2. Parental stressor scale: neonatal intensive care unit
The stress was assessed by the Parental Stressor Scale: Neonatal Intensive Care Unit. The scale consists of 26 items in three categories including infant behavior and appearance, sights, and sounds, and parental role alterations with a 5-point Likert scale ranging from "not stressful" (score 1) to "completely stressful" (score 5). The validity and reliability of this scale in Persian were verified previously[19].
2.3.3. Perceived maternal parenting self-efficacy
Maternal self-efficacy was measured through "Perceived Maternal Parenting Self-Efficacy" consisting of 20 items with a 5-point Likert scale ranging from "never" (score 1) to "always" (score 5). The questionnaire has four subscales including caretaking procedures,evoking behaviors, reading behaviors, and situational beliefs. The validity and reliability of this tool in Persian was verified and validated previously[20].
2.3.4. Multidimensional scale of perceived social support
Multidimensional Scale of Perceived Social Support was used to measure perceived social support. This is a 12-item scale with a 5-point Likert scale ranging from "never" (score 1) to "always"(score 5). The subscales include family support, friends support, and significant others support. Each subscale has 4 items[21].
2.3.5. Parent perceptions of their child's hospital discharge
This tool designed to assess mothers' readiness for discharge was developed by Berry et al[22]. The questionnaire consisted of 17 items with 5-point Likert scales ranging from "strongly disagree" (score 1) to "strongly agree" (score 5). In this study, this questionnaire was used for the first time in Persian version. After obtaining permission from the designer of the questionnaire, the followed processes were forward-backward translation and other psychometric measures such as face validity, qualitative content validity, content validity ration and content validity index. To determine the content validity ratio, 10 nursing faculty members were asked as an expert panel to rate each question based on three options including essential (score 3), useful but not essential (score 2), and not necessary (score 1).The results were put in the formula of content validity ration = (ne -n/2) /n/2 where ne is the number of experts who have confirmed the necessity of the question and n is the total number of experts. Then,the attained results were compared with the Lawshe table. According to the Lawshe table, the minimum acceptable content validity ratio score for 10 experts was 0.62[23], the score above 0.8 for all questions of the questionnaire, and all questions were retained in the questionnaire.
To evaluate the content validity index, the team of experts was asked to rate the "relevancy" of each question to the study objective by 1 to 4. The content validity index was obtained in different parts of the questionnaire between 88.5 and 100 and since the mean score of over 0.7 is acceptable for the questionnaire[24], the relevancy of all questions was confirmed as well.
The reliability of all the above tools was assessed using internal consistency (Cronbach's alpha). All tools were completed by 20 mothers of preterm infants admitted to the eligible NICU who were excluded later. Cronbach's alpha coefficients for Parent Perceptions of Their Child's Hospital Discharge, Parental Stressor Scale:Neonatal Intensive Care Unit, Perceived Maternal Parenting Self-Efficacy, and Multidimensional Perceived Social Support Scale were 0.88, 0.84, 0.86 and 0.86, respectively.
2.4. Data collection
After obtaining ethical approval, the researcher visited the research sites at different times and days of the week for approximately 2 months and started sampling based on the inclusion criteria.
2.5. Statistical analysis
Data were analyzed with IBM SPSS version 20 software using descriptive statistics including frequency, frequency percentage,mean and standard deviation as well as inferential statistics such as Pearson correlation coefficient and stepwise regression at the significance level of 0.05.
2.6. Ethical approval statement
The study was approved by the Ethics Committee of the Faculty of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, with a code of IR.SBMU.PHARMACY.REC.1397.177.The researcher obtained permission to enter the NICU of hospitals affiliated to Lorestan University of Medical Sciences. At the baseline,the study objectives and methodology and the confidentiality of information were explained to the participants, and all participants received the tools if they wished to participate in the study. When the questionnaire was completed by the mother, the researcher was present on site to answer the mother's possible questions. After completion, the questionnaires were collected by the researcher.
3. Results
3.1. General characteristics
Most mothers were in the age group of 25 to 34 years (44.2%)and most fathers were in the age group of 30 to 39 years (45.8%).Moreover, 43.3% of mothers had an educational level of high school and 41.2% of fathers had academic education. Housewives (70.8%)and self-employed fathers (65.8%) had the highest percentage of employment status. The highest percentage of mothers had one child(40%), one para (38.3%), and two gravidas (37.1%). In addition, the highest percentage of infants were boys (61.7%), their gestational age was over 34 weeks (43.3%), their weight was over 2 000 g (54.2%), and their hospitalization period was less than 20 days (56.7%) (Table 1).
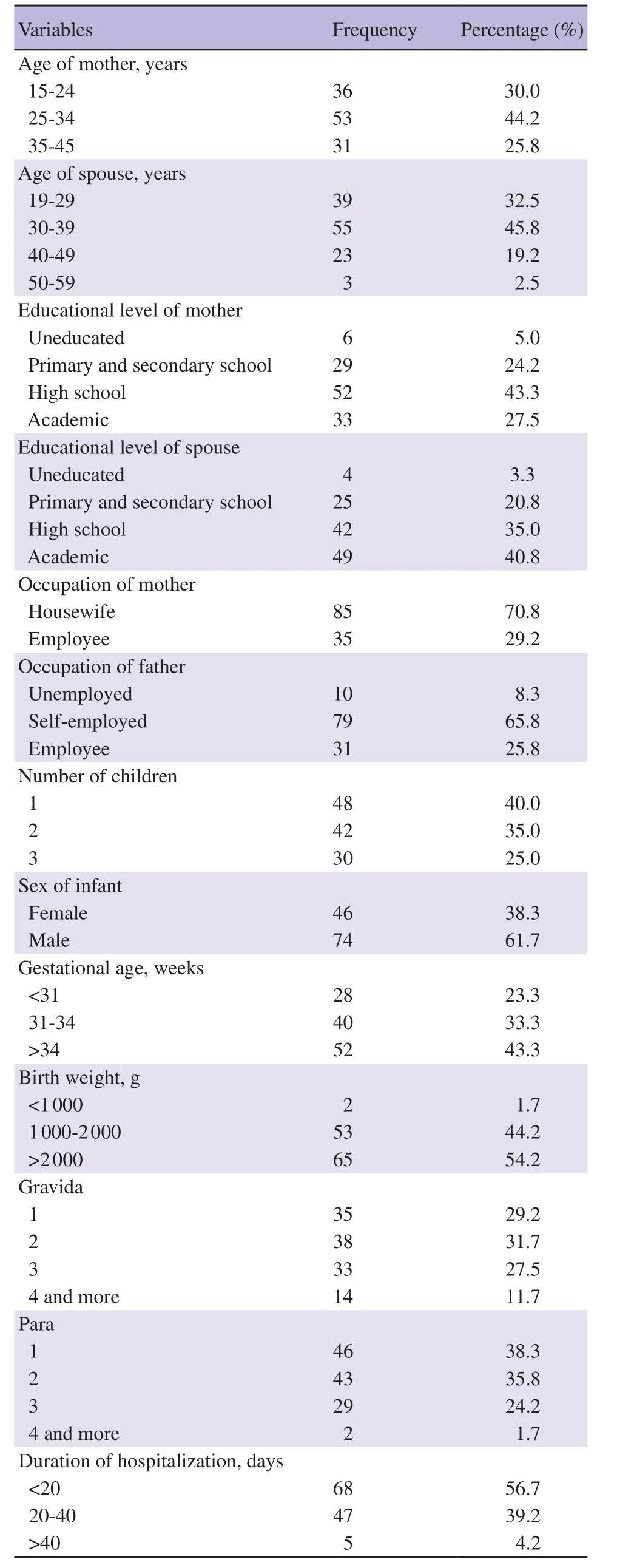
Table 1. Demographic characteristics of mothers of preterm infants.
According to Table 2, among the stressors, infant behavior and appearance achieved the highest mean score (3.25±1.03) and then parental role alterations (3.22±0.99). Among the self-efficacy dimensions, including caretaking procedures, evoking behaviors,reading behaviors, and situational belief, its last dimension,situational belief, achieved the highest mean score (4.28±0.77).Concerning the perceived social support, the family support achieved the highest mean score (4.13±0.90) compared to friends support, and significant others support.
3.2. Correlation between stress, self-efficacy and perceived social support and readiness for discharge
As shown in Table 3, stress and all its dimensions had a relatively strong inverse correlation with readiness for discharge in mothers of preterm infants, meaning the higher the stress of the mother, the lower the readiness for discharge. Among the stress dimensions, the infant behavior and appearance had the highest inverse correlation with the readiness for discharge (r=-0.686, P<0.001). In addition,self-efficacy and perceived social support had a relatively strong and direct correlation with mothers' readiness for discharge (r=0.701 and r=0.770, respectively; P<0.001). The caretaking procedures among self-efficacy and family support among perceived social support were most strongly correlated with readiness for discharge (r=0.609,r=0.724, respectively; P<0.001).
3.3. Predictors of readiness for discharge in mothers of preterm infants
Table 4 presents the stepwise linear regression results to determine the predictors of three variables, including stress, self-efficacy, and perceived social support on readiness for discharge in the mothers of preterm infants. According to the results of the table, contrary to this relationship, perceived social support had the highest relationship with readiness for discharge in mothers of preterm infants. As the other variables are constant, 0.43 is added to readiness for discharge in mothers of preterm infants per 1 unit increase in perceived social support. The self-efficacy also had a significant and direct relationship with readiness for discharge in mothers of preterm infants and provided that other variables were stable, the selfefficacy of the mothers increased by 0.35 for mothers' readiness for discharge. The readiness for discharge had no relationship with stress.
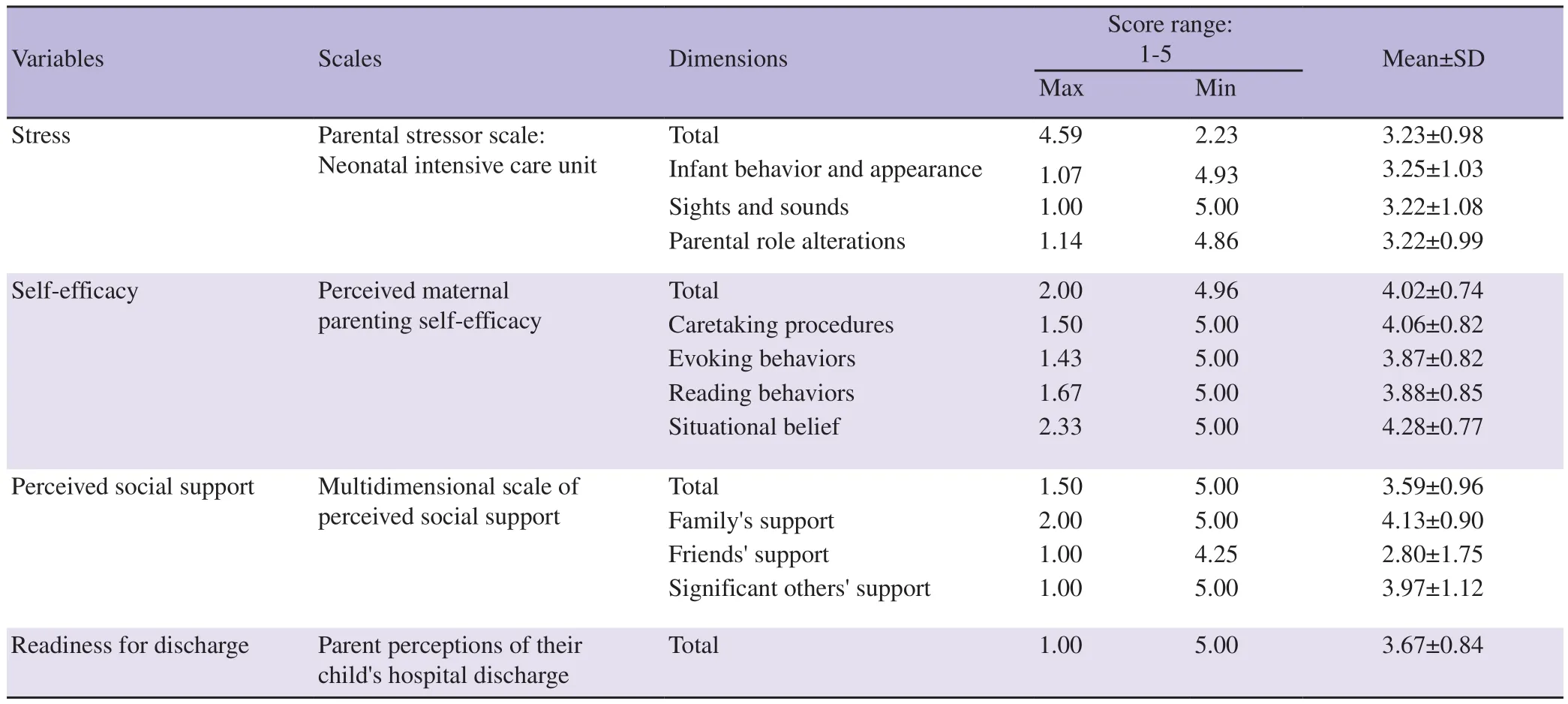
Table 2. Mean and standard deviation (SD) of research variables and their dimensions.

Table 3. Correlation (r) of stress, self-efficacy and perceived social support with readiness for discharge in mothers of preterm infants.
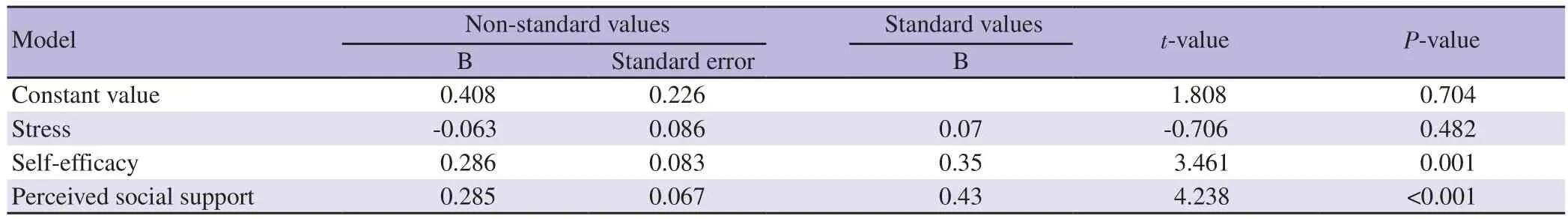
Table 4. Stepwise regression results considering readiness for discharge as dependent variable and stress, perceived social support and self-efficacy of mothers with preterm infants as independent variables.
4. Discussion
The results of this regression model showed that the readiness for discharge was increased in the mothers of preterm infants with increasing perceived social support and self-efficacy.
According to the findings of this study, among the three stressors for infant mothers, including infant behavior and appearance, sights,and sounds, and parental role alterations, infant behavior, and appearance were the most stressful factors for mothers of preterm infants, with a slight difference. Given the various stressors for mothers of preterm infants admitted to the NICU, familiarizing them with newborn conditions or the care and treatment process may bea way to reduce their stress. Consistent with this result, in another study, the infant appearance and behavior were the most stressful factors for mothers[25]. In the study of Baia et al, the most common factor for parental stress was parental role alterations[26].
Of the four dimensions of mothers' self-efficacy, including caretaking procedures, evoking behaviors, reading behaviors,and situational beliefs, the last one, situational belief, scored the highest. Given the results of this study that the situational belief had the highest self-efficacy across different dimensions, it can be interpreted that an Iranian mother will have a greater sense of self-efficacy because her infant understands and responds to her affection, as well as the best way to increase self-efficacy may be that mother-infant attachment and contact should be strengthened.In another study, situational belief had the highest score of maternal self-efficacy[27]. Contrary to this finding, a study by ZareiNezhad et al aimed to determine self-efficacy and its relationship with quality of life in mothers with preterm infants, and the results showed that evoking behaviors had the highest contribution to mothers' selfefficacy[28]. The caretaking procedures imply measures like feeding and changing a diaper. The evoking behaviors imply measures like catching the child's attention and calming the child in his or her mood. The reading behaviors signify measures like the mother's understanding of when the baby is sick or when the baby needs to sleep. The situational belief implies the mother's belief that the child responds to her and she can understand the affection for the child[29].
Concerning the perceived social support, the family support also scored higher than friends' and others' support, suggesting that the family is the strongest contributor to postpartum Iranian women,especially those who have preterm infants. Consistent with this result, in the study of Yanıkkerem et al, who evaluated the factors affecting readiness for discharge and perceived social support after childbirth, the family support had the highest score[30]. In another study, the family among the dimensions of social support received the highest score for supporting Iranian pregnant women who were close to the time of labor[31].
The other main result of the study showed that self-efficacy was a predictor of readiness for discharge in mothers of preterm infants,meaning the mothers' readiness to discharge increased to 0.35 units with a one-unit increase in self-efficacy. This finding showed that readiness for discharge could be enhanced by empowering and enhancing the mother's self-confidence, which is an element of selfefficacy[11]. In a systematic review and meta-analysis, the results suggested that parental training interventions for preterm infants could enhance parental self-efficacy[32]. In a qualitative study by Raffray et al, healthcare providers found maternal skill acquisition and self-confidence in infant care as facilitator of early infant discharge[33].
According to the findings of the study, the perceived social support is a predictor of readiness for discharge in mothers of preterm infants, meaning that the readiness for discharge increased to 0.43 units with one unit increase in perceived social support and this predictability is stronger than self-efficacy. It should be noted that a holistic approach to discharge planning should include social and psychological support[34]. Given the results of this study that the family played the most roles in social support, using approaches such as family-centered care that focus on the whole family can increase perceived social support and thus readiness for discharge mothers.Correspondingly, Nilsson et al identified social support as one of the factors influencing early maternal discharge after childbirth[35]. A review study found that maternal social support is one of the criteria for preterm infant discharge[36].
Some of the major limitations of this study include the large number of study tool questions, and the stress of mothers due to hospitalization of the infant, which may affect their attention and accuracy in completing the questions of the questionnaire. Since this study was conducted in one of the major Iranian cities with a socio-cultural background similar to other cities, its results can be generalized to mothers of infants throughout Iran.
This study is unique in that it was conducted for the first time in Iran to determine the predictors of three variables, including stress,self-efficacy and social support in readiness for discharge in mothers of preterm infants. The results of the regression model in this study showed that self-efficacy and social support had a direct relationship with readiness for discharge in the mothers of preterm infants, and the predictive role of perceived social support is slightly stronger than self-efficacy.
In conclusion, this study shows that stress, self-efficacy, and perceived social support can be considered as predictors of readiness for discharge in mothers of preterm infants. According to the findings of this study, it is suggested that measures should be taken to promote self-efficacy and perceived social support for mothers of preterm infants to improve maternal readiness for discharge. In this regard, we recommend: educating mothers of preterm infants about infant conditions and the process of care and recovery, enhancing mothers' participation in infant care, strengthening motherinfant attachment, encouraging and educating breastfeeding, and reinforcing the presence of family members, especially the father,when training and participating in care. In addition, we suggest that further studies should be conducted on the effects of empowerment programs to increase self-efficacy and perceived social support on readiness for discharge in mothers with preterm infants.
Conflict of interest statement
The authors declared that there is no conflict of interest.
Acknowledgments
The authors would like to thank and appreciate all of mothers with hospitalized preterm infants for participating in the study.
Funding
The study received no extramural funding.
Authors’ contributions
All authors have seen and approved the manuscript and contributed significantly to the study. Parvaneh Vasli and Sedighe Valipour contributed to conceptualization, analysis and interpretation of data,project administration, and writing of the original draft. Maliheh Nasiri contributed to analysis and interpretation of data. Parvaneh Vasli, Fatemeh Estebsari and Maliheh Nasiri contributed to final approval of the manuscript.
Publisher’s Note
The Publisher of the Journal remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
 Asian Pacific Journal of Reproduction2022年6期
Asian Pacific Journal of Reproduction2022年6期
- Asian Pacific Journal of Reproduction的其它文章
- Clinical pregnancy rate of women with unexplained infertility with or without cervical mucus aspiration before intrauterine insemination: A randomized controlled trial
- Prevalence and risks of reproductive tract infections among women of urban slums in North India: A cross-sectional study
- Awareness about transmission and preventive measures of COVID-19 from mother to child: A cross-sectional study among pregnant women
- L-arginine alleviates postmenopausal complications in female rats by stimulating ovarian dopamine beta hydroxylase
- Exogenous gonadotropin releasing hormone (GnRH) modulates scrotal and testicular biometrics, libido, endocrinological and heamatological profiles in Ganjam goat under humid tropical coastal ecosystem of Odisha
- Ovarian hyperstimulation syndrome following the use of GnRH agonist trigger of final oocyte maturation and freeze-all strategy: A case report and review of the literature
