Clinical pregnancy rate of women with unexplained infertility with or without cervical mucus aspiration before intrauterine insemination: A randomized controlled trial
Richa Vatsa, Vanita Suri, Shalini Gainder, Aashima Arora, Japleen Kaur,3✉, Neelam Choudhary, Shruti Sharma
1Department of Obstetrics and Gynaecology, Postgraduate Institute of Medical Education and Research, Chandigarh 120012, India
2Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi 110029, India
3Department of Obstetrics and Gynaecology, Dr B R Ambedkar Institute of Medical Sciences, 56 A, Sector 56, SAS Nagar, Punjab 160055, India
ABSTRACT
Objective: To detect effect of removing cervical mucus before performing intrauterine insemination (IUI) on pregnancy rate in patients with unexplained infertility.
Methods: The randomized controlled trial was conducted in Infertility Division of Department of Obstetrics and Gynaecology of a tertiary care hospital. Totally 80 patients of unexplained infertility were recruited. By computer generated block randomization in block size of 4 and 6, patients were randomly allocated at time of starting ovarian stimulation into the cervical mucus removal group or the non-removal of cervical mucus group before IUI, 40 in each group. Ovarian stimulation with clomiphene 100 mg from day 2-6 of menstrual cycle along with human menopausal gonadotropin 150 IU was given alternate day starting from day 7. Follicular monitoring was done and further doses given as per response; trigger was planned when 1-3 follicle reach a diameter of >18 mm. IUI was planned after trigger. IUI was done as per the group allocated. Mucus cleaning was done in the cervical mucus removal group by aspirating mucus with IUI syringe and sterile cotton swab before IUI. The primary outcome was clinical pregnancy rate. Number of difficult IUIs and cycle cancellation due to ovarian hyperstimulation were also noted.
Results: IUI was not done in 4 patients due to hyperstimulation.Pregnancies per IUI cycle occurred in 7.9% (3/38) in the cervical mucus removal group and 21.1% (8/38) in the non-removal of cervical mucus group. There was no statistically significant difference in clinical pregnancy rate between two groups (P=0.19).
Conclusions: There is a trend towards a lower clinical pregnancy rate with removal of cervical mucus before IUI in women of unexplained infertility though the difference is not statistically significant. Further studies with large sample size need to be done on this intervention.
Trial registration: The trial registration was done with Clinical Trial Registry-India (Registration number: CTRI/2019/03/018326).
KEYWORDS: Unexplained infertility; Intrauterine insemination; Cervical mucus removal; Pregnancy outcome;Randomized controlled trial
1. Introduction
Unexplained infertility accounts for approximately one third of cases of infertility[1,2]. In the absence of an identifiable anomaly,treatment of unexplained infertility is largely empirical. The most widely used treatment for unexplained infertility is controlled ovarian stimulation with intrauterine insemination (IUI) and in vitro fertilization (IVF)[3]. Before shifting to invasive and expensive fertility procedures, the physician should always provide couples with treatment options that may achieve higher success rates than ordinary intercourse and demand low cost and less monitoring than IVF. IUI can be easily performed, is relatively inexpensive and can be done in low-resource clinics. The reported pregnancy rates per IUI cycle range from 8% to 33%[4-8]. Various modalities have been tried to improve success rate of IUI in unexplained infertility like doing double IUI, changing medication for ovarian stimulation,none of these have proven efficacy.
Hostile cervical mucus can be one of the reasons behind unexplained infertility. While IUI can avoid cervical mucus and its undesirable properties, some of its effects may still be present. Our hypothesis is that this hostile cervical mucus can get inside uterus while doing IUI, and might have negative impact on outcome of IUI by affecting sperm-ovum interaction. Effect of cervical mucus removal before embryo transfer in IVF/intracytoplasmic sperm injection (ICSI) cycle has been extensively studied[9-12]. But effect of this procedure on outcome of IUI requires further investigation.Therefore, this study was planned to evaluate effect of cervical mucus cleaning on outcome of IUI.
The primary objective of the study was clinical pregnancy rate(defined as ultrasound evidence of pregnancy) per IUI cycle.Secondary objectives were biochemical pregnancy rate, multiple pregnancy rates (>1 gestational sac seen at 6 weeks) and cycle cancellation rate due to risk of ovarian hyperstimulation syndrome.
2. Materials and methods
2.1. Trial design
It was a prospective randomized trial conducted in the Infertility Outpatient Department of the Department of Obstetrics and Gynecology of a tertiary care hospital. The patients were recruited between April 2019 and July 2019 and followed from one to three cycles. The patients were explained about the study design in detail after which consent for the participation in the trial was obtained.
2.2. Participants
History was taken in detail. Coital history was taken to rule out sexual dysfunction, menstrual history (as surrogate for ovulatory dysfunction), and obstetric history. All females underwent thorough examination. Husband semen analysis was done as per the World Health Organization 2010 criteria[13]. A baseline ultrasound was done to rule out structural abnormalities of uterus (fibroids or endometrial polyps) and ovaries (endometriomas or polycystic ovaries). Assessment of ovarian reserve was done by serum anti Mullerian hormone (AMH) and day-3 follicle stimulating hormone(FSH). Further ovarian reserve was tested by antral follicle count(AFC). Tubal patency was assessed by hysterosalpingogrphy (HSG)using water soluble dye. Intraoperative findings of laparoscopy and hysteroscopy (if performed) were duly recorded.
Infertile couples with normal semen analysis (WHO 2010 standards), age of female partner <37 years, FSH <10 IU/L, day 2/3 AFC of 10-24 (combined two ovaries), prolactin <24 ng/mL, bilateral patent tubes on HSG and no evidence of ovulatory dysfunction were considered to have unexplained infertility. Both primary and secondary infertility cases were included. Patients who had more than three previous IUI attempts, patients with unilateral tubal block,chronic liver or renal disease, endocrinological conditions (diabetes mellitus, and hypoyhyroidism) and history of breast or gynecological malignancy were excluded from the study.
2.3. Randomisation
A total of 80 patients were included in the study and divided into two groups, with 40 in each group. The same clinician enrolled all the participants and those meeting the eligibility criteria were randomized by a computer-generated trial sequence (block randomization in the block size of 4 and 6) into one of the two study groups, after obtaining informed consent. The sequence was generated by statistician, kept confidential by him and was asked about the same at time of allocation of treatment arm to the patient.
2.4. Sample size calculation
As per study conducted by Abdallah et al, the pregnancy rate was 18% in patients where cervical mucus was removed and 8% when the intervention was not done[14]. At a study power of 80% with an α-error of 0.05, a sample size of 176 cycles was needed for both groups. As this was time bound project during fellowship, sample size of 40 in each group was taken as per IUI load of our clinic.
2.5. Intervention
Each couple in the study was involved for maximum first three cycles of IUIs, as our institute protocol was to offer 3-4 cycles of IUI in couples with unexplained infertility and after that we switched to IVF. The trial was non blinded. In both the groups, in all the cycles, controlled ovarian stimulation was done by combination of clomiphene citrate and human menopausal gonadotropin (hMG).Starting from day 2/3 of menstrual cycle, tablet clomiphene citrate 100 mg once a day was given for 5 days. Starting from day 7/8,intramuscular injection of hMG 150 IU was given alternate day until one to two dominant follicles of ≥18 mm were detected.
Follicular monitoring was done in both groups by transvaginal ultrasonography, daily or alternate day depending on size of dominant follicles, starting from day 11, till the leading follicle reaches a size of 18 mm (average of diameter measured in three dimensions). At the same time, the endometrial thickness was noted.Ovulation was triggered with intramuscular injection of highly purified human chorionic gonadotropin (hCG,10 000 IU) followed by IUI 36-40 h later. If there were 4 or more follicles of >15 mm,patients were counseled about risk of ovarian hyperstimulation syndrome (OHSS) and multiple pregnancy; cycle was cancelled.Semen sample was produced by masturbation. Semen was prepared by swim up technique in modified Human Tubal Fluid (HTF)solution media (Hi-Tech solutions).
Patients were allocated into two groups depending on removal(group A) or non-removal (group B) of cervical mucus before IUI.In group A, cervical mucus was removed with IUI catheter attached to 1 mL syringe (Infer Tech Fertile Solutions) by repeatedly moving catheter in cervical canal from the internal to external os maintaining negative suction with it, until mucus stopped coming. This was followed by saline wet cotton swab stick to ensure complete removal. In group B, cervical mucus was not removed. After this,all the patients were inseminated with 0.5-0.8 mL prepared semen in 1 mL syringe attached to a new IUI catheter (Infer Tech Fertile Solutions). IUI catheter was carefully passed into uterine cavity well above internal cervical os and insemination done over 20-30 s. Patients were advised to remain in dorsal position for 10-15 min. It was ensured that IUI is being done within 60-90 min of semen collection. All the inseminations were performed by a single clinician. Patients were also advised to have intercourse for following 2 days. Micronized vaginal progesterone 200 mg twice a day for 14 days was given to all patients for luteal phase support,following which urine pregnancy test was done. The procedure was repeated for up to three cycles in both the groups. No changes in trial were done after trial commencement.
2.6. Primary and secondary outcomes
The primary outcome was the clinical pregnancy rate per IUI cycle. The patient where pregnancy was visible on ultrasonography was defined as clinical pregnancy. The secondary outcomes were biochemical pregnancy rate, multiple pregnancy rates (>1 gestational sac seen at 6 weeks) and cycle cancellation rate.
2.7. Statistical analysis
Statistical analysis was performed using STATA (StataCrop)software version 16.0. Descriptive statistics such as mean±standard deviation (mean±SD) was calculated for continuous variables such as age of patients and duration of symptoms. The comparison of continuous variables with normal distribution, between cases and controls was done by t-test. Frequencies of outcomes across the categories were represented as frequency and percentage values. To compare the frequency of occurrences of outcomes across categories,Chi-square/Fisher’s exact tests were used as appropriate. For all tests, a two-tailed probability of P<0.05 was considered statistically significant.
2.8. Ethics statement and trial registration
This study was approved by Institute Ethics Committee (Letter No. INT/IEC/2019/00413). The study trial registration was done with Clinical Trial Registry- India (Registration number:CTRI/2019/03/018326).
3. Results
3.1. Comparison of baseline characteristics between the two groups
We randomized 80 patients with unexplained infertility into two groups. Out of them, 4 cycles in 4 patients, two in each group (5%)were cancelled due to multifollicular development. The number of participants who were randomly assigned, received intended treatment, and were analysed for the primary outcome is provided in Figure 1.
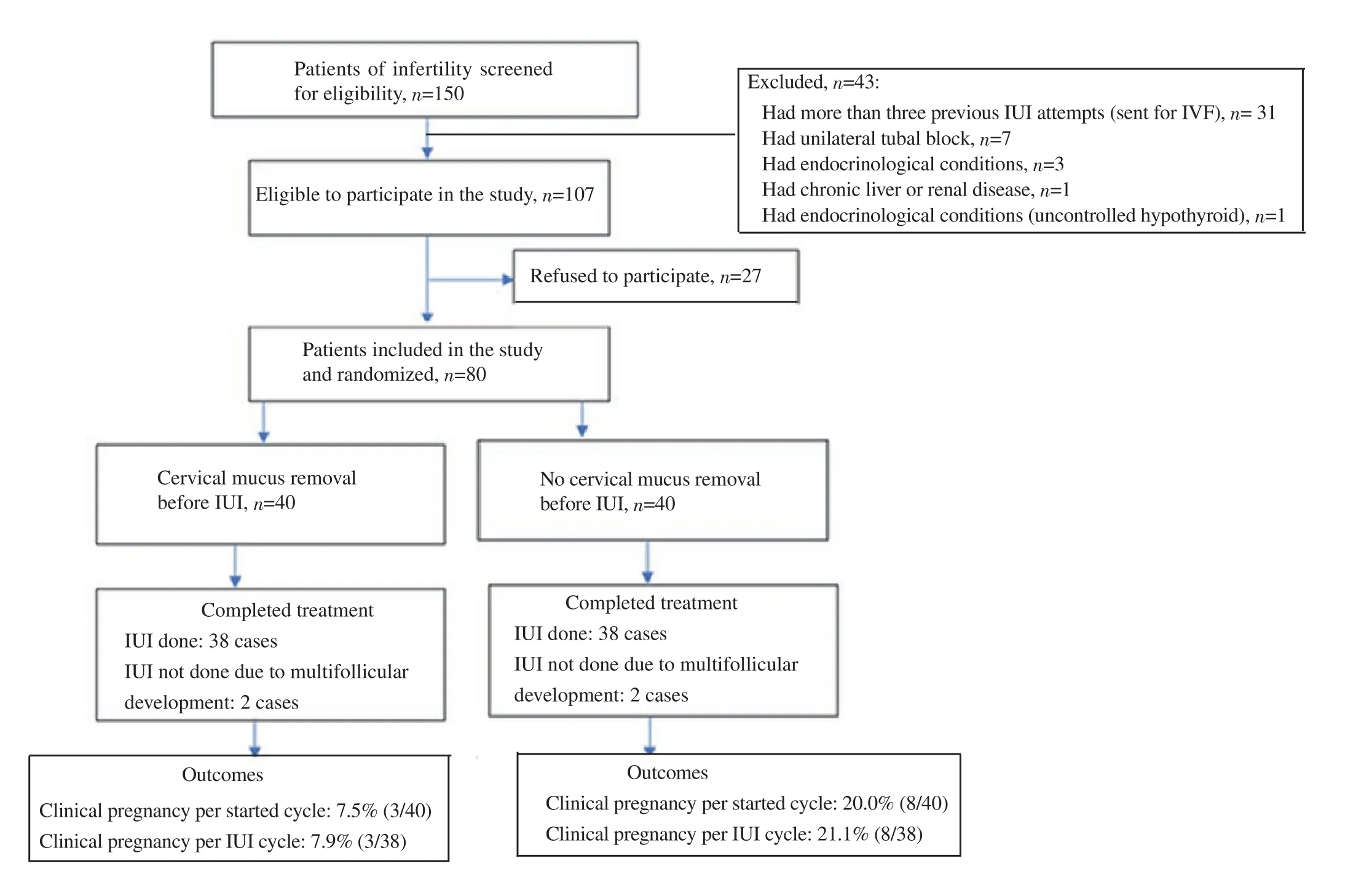
Figure 1. Flowchart of screening of the study.
There were no differences in baseline characteristics of the patients like age, duration of infertility, previous conception, previous live birth, history of previous one or two IUI, BMI, serum hormone levels (TSH, prolactin, FSH, LH) and markers of ovarian reserve(AFC, serum AMH) between the two groups, so the study population was homogenous. Baseline characteristics of the patients are given in Table 1.
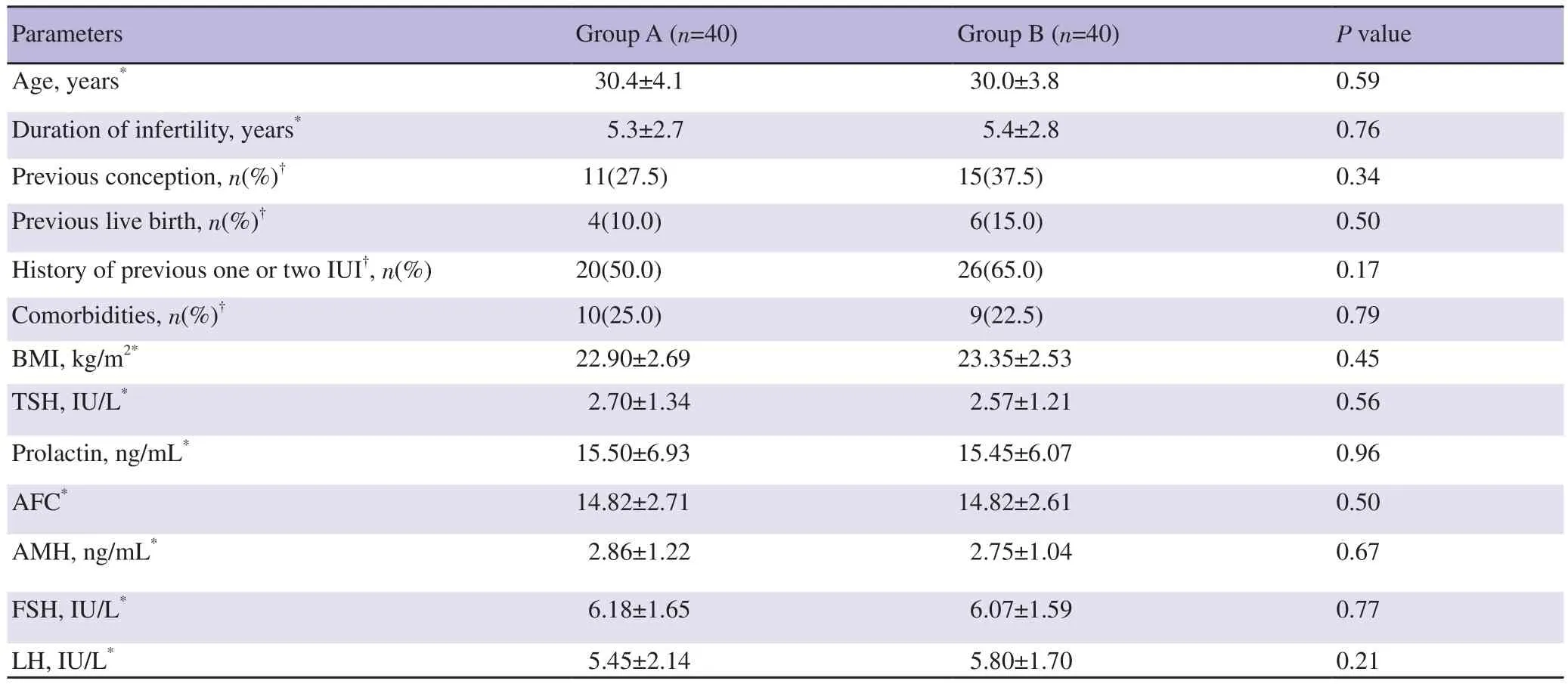
Table 1. Comparison of the baseline characteristics of patients in the two groups.
3.2. Comparison of ovarian stimulation and IUI characteristics between the two groups
Ovarian stimulation characteristics like dose of gonadotropins required, endometrial thickness and mean number of dominant follicles were similar in the two groups, so this could not be the reason of difference in outcome of IUI. Difficult IUI was experienced in 5.3%(2/38) in group A and 13.2% (5/38) in group B (P=0.43) (Table 2).
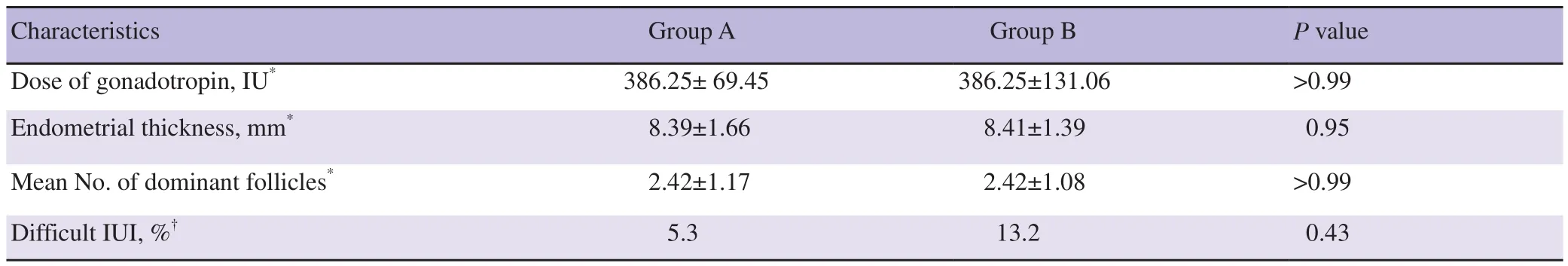
Table 2. Stimulation characteristics of IUI cycle of patients in the two groups.
3.3. Outcomes
The comparison of primary outcome was done per started cycle and per IUI cycle. Totally 7.5% (3/40) patients became pregnant in group A (cleaning of cervical mucus) and 20.0% (8/40) in group B (no cleaning of cervical mucus), per started cycle (P=0.19). Pregnancies occurred in 7.9% (3/38) in group A and 21.1% (8/38) group B, per IUI cycle (P=0.19). It was showing a trend towards harm by mucus cleaning but the effect was not statistically significant. Secondary outcome of cycle cancellation due to hyperstimulation was the same between two groups (5% each). There was no case of multiple pregnancy or biochemical pregnancy in either of the groups.
4. Discussion
We evaluated the effect of cervical mucus cleaning on the outcome of IUI in cases of unexplained infertility. We found the pregnancy rate of 7.9% per IUI cycle when cervical mucus was cleaned before IUI and 21.1% when this intervention was not done; a trend towards harm with the intervention though the result did not reach statistical significance.
The potential causes of unexplained infertility include disturbances in endocrine balance, immunology and genetic or reproductive physiology, but nothing is conclusively known[2]. In the absence of any identifiable cause, treatment of unexplained infertility is mostly empirical. The most widely used evidence-based treatment for unexplained infertility is controlled ovarian stimulation with IUI and IVF. The reported pregnancy rates per IUI cycle range from 8% to 33% depending on numerous factors like duration of infertility,age of female, semen quality, method of semen preparation, single or double IUI, stimulation protocol used, etc[4-7]. National Institute of Health and Care Excellence (NICE) guideline recommends IVF as the first line treatment after 2 years of unexplained infertility[8].In clinical practice, most of the times, 3-6 cycles of controlled ovarian stimulation with IUI are considered for primary treatment of unexplained infertility. The lesser cost, side effects and complexity of treatment can be the cause of this preference. The clinicians have been trying to improve the success of IUI by various modalities like doing double IUI in a controlled ovarian stimulation cycle,altering stimulation protocols, changing timing of insemination, etc.In natural conception, cervical mucus helps in sperm capacitation and acts as reservoir of sperm in cervical canal. But hostile cervical mucus can be one of the reasons behind unexplained infertility. It has been hypothesized that when this hostile cervical mucus enters inside uterine cavity during IUI, it can negatively affect sperm motility and may decrease the success of the procedure. Cervical mucus removal is a cost effective and less labor-intensive modality,which can be routinely used before IUI, if it improves the outcome of the procedure. The effect of cervical mucus removal before embryo transfer in IVF/ICSI cycle has been extensively studied.Initial studies have shown the advantage of this intervention on IVF outcome[9] but later studies[10] found the disadvantage of the same procedure and finally Cochrane review and other meta-analysis refuted the advantage of the procedure[11,12]. Therefore, the effect of this procedure on outcome of IUI requires further investigation.Previous studies have shown the significant advantage of cervical mucus removal on outcome of IUI in unexplained infertility[14-16]and other causes of infertility as well[17-19]. Simsek et al performed a prospective study with retrospective controls, the authors included all the types of infertility (unexplained, female factor, male factor,combined female and male factor). Totally 505 case of mucus cleaning were compared with 1 057 retrospective controls[17]. The authors found that cervical mucus aspiration before IUI significantly improved overall clinical pregnancy rates (15.1% in the aspiration group vs. 9.9% in the control group; P=0.05) more so in unexplained infertility (24% in the aspiration group vs. 9.5% in the control group;P=0.04). Berjis et al conducted a randomized controlled trial (RCT)on cervical mucus cleaning before IUI in patients of unexplained infertility. Totally 112 patients in each group were included. The authors found non-significant increase in pregnancy rate by cleaning cervical canal with swab before IUI (15.1% vs. 9.8%; P=0.31)[16].Ghasemi et al conducted a RCT on this topic in IUI performed for all indications. Totally 148 cases and 143 controls were included and the study showed increase in pregnancy rates (14.2 % vs. 7.0%; P=0.04)by doing this intervention[18]. Similarly, Abdallah et al conducted a prospective study with retrospective controls, enrolling 50 patients of unexplained infertility in two groups. The authors found increase in pregnancy rates of IUI when done after cleaning of cervical mucus (18% vs. 8%; P=0.05)[14]. In a RCT done by Azmodeh et al in total 154 cases and 156 controls of moderate male infertility and unexplained infertility, cervical mucus cleaning before IUI was found beneficial (14.3 % vs. 10.3%; P=0.02)[19]. The largest RCT conducted on this intervention was done by Maher et al in 361 cases and 353 controls of unexplained infertility, and the authors found significant increase in pregnancy rates by doing this intervention(31.0% vs. 21.8%; P=0.005)[15]. Different method of mucus cleaning was used in different studies. Simsek et al and Abdallah et al in their study cleaned the cervical mucus by aspirating it with insemination catheter[17,14]. Berjis et al and Azmodeh et al used cotton swab roundly and genteelly with 3-5 swabs made wet with ringer lactate solution or normal saline[16,19]. Maher et al combined the above two methods. They first used insemination catheter by passing it repeatedly from internal to external os. Then, saline soaked small cotton swab was used to completely remove the cervical mucus[15].In the present study, cervical mucus was removed with IUI catheter attached to 1 mL syringe (Infer Tech Fertile Solutions) by repeatedly moving catheter in cervical canal from the internal to external os maintaining negative suction with it, until mucus stopped coming.This was followed by saline wet cotton swab stick to ensure complete removal.
Many probable reasons have been hypothesized for increasing success rate of IUI by cervical mucus removal, e.g. sperm will not come in contact with hostile cervical mucus, which is supposed to decrease its motility and oocyte-sperm interaction[17]. Also,introduction of cervical mucus into uterine cavity can introduce pathogenic microorganisms inside which have been shown to decrease success rate of embryo transfer in IVF; the same mechanism can have a detrimental effect on IUI success also.
Our study found a trend of negative effect of mucus cleaning on the outcome of IUI, though the result did not reach statistical significance. The reason behind potential harmful effect of cervical mucus cleaning on outcome of IUI can be multiple. Though our study did not find statistically significant increase in difficult IUI with cervical mucus removal, it has been hypothesized that the removal of the lubricating effect of the cervical mucus may lead to difficult IUI and thus counterbalance any beneficial effects of the same. Cervical mucus could be the site of commensal and useful microorganism which could be good for IUI success and removal of the same can explain poorer IUI outcome. Further, touching the cervical canal repeatedly can stimulate uterine contractions, which can also have a negative effect on conception rate[20].
The strength of the study is that it was a randomized controlled trial done on a homogenous study population (age, duration of infertility,unexplained infertility), using same ovarian stimulation protocol,thus, minimizing confounding factors which could have affected the outcome of IUI. The limitation of the study was its small sample size for the effect on primary outcome. Future studies on evaluating the cervical mucus for presence of antisperm antibodies and cervical swab culture in both mucus cleaning and non-cleaning groups and correlating this with IUI outcome can throw some light on the mechanism effect of this intervention. Further, whether one method of cleaning being useful or not needs to be investigated, so that standardization of the intervention could be done.
In conclusion, this study has shown result completely opposite from other studies done on this intervention. We find a trend towards harm from cervical mucus cleaning before IUI in unexplained infertility cases, though the effect is not statistically significant, in contrast to all other studies which showed the advantage of the intervention in unexplained infertility and other cases of IUI. Hence, further large randomized trials should be done to see the effect of intervention.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Funding
This study received no extramural funding.
Authors’ contributions
Richa Vatsa was involved in conceptualization, writing,validation, review, and formal analysis. Vanita Suri was involved in conceptualization, validation, investigation, and methodology.Shalini Gainder was involved in conceptualization, validation and methodology. Aashima Arora was involved in conceptualization,validation, and methodology. Japleen Kaur was involved in conceptualization, writing, validation, investigation, and methodology. Neelam Choudhary was involved in conceptualization,validation, investigation, and methodology. Shruti Sharma was involved in conceptualization, validation and investigation.
Publisher’s Note
The Publisher of the Journal remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
 Asian Pacific Journal of Reproduction2022年6期
Asian Pacific Journal of Reproduction2022年6期
- Asian Pacific Journal of Reproduction的其它文章
- Ovarian hyperstimulation syndrome following the use of GnRH agonist trigger of final oocyte maturation and freeze-all strategy: A case report and review of the literature
- Exogenous gonadotropin releasing hormone (GnRH) modulates scrotal and testicular biometrics, libido, endocrinological and heamatological profiles in Ganjam goat under humid tropical coastal ecosystem of Odisha
- L-arginine alleviates postmenopausal complications in female rats by stimulating ovarian dopamine beta hydroxylase
- Predictors of readiness for discharge in mothers of preterm infants: The role of stress,self-efficacy and perceived social support
- Awareness about transmission and preventive measures of COVID-19 from mother to child: A cross-sectional study among pregnant women
- Prevalence and risks of reproductive tract infections among women of urban slums in North India: A cross-sectional study
