Diagnosis, treatment, and current concepts in the endoscopic management of gastroenteropancreatic neuroendocrine neoplasms
Giuseppe Iabichino, Milena Di Leo, Monica Arena, Giovanni Giuseppe Rubis Passoni, Elisabetta Morandi,Francesca Turpini, Paolo Viaggi, Carmelo Luigiano, Luca De Luca
Abstract Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) are rare tumors derived from the neuroendocrine cell system, which that have increased in incidence and prevalence in recent years. Despite improvements in radiological and metabolic imaging, endoscopy still plays a pivotal role in the number of GEPNENs. Tumor detection, characterization, and staging are essential in management and treatment planning. Upper and lower gastrointestinal (GI)endoscopy is essential for correct localization of the primary tumor site of GI NENs. Endoscopic ultrasonography (EUS) has an important role in the imaging and tissue acquisition of pancreatic NENs and locoregional staging of GI neuroendocrine tumors. Correct staging and histological diagnosis have important prognostic implications. Endoscopic operating techniques allow the removal of small GI NENs in the early stage of mucosal or submucosal invasion of the intestinal wall. Preoperative EUS-guided techniques may help the surgeon locate small and deep tumors, thus avoiding formal pancreatic resections in favor of parenchymal-sparing surgery. Finally, locoregional ablative treatments have been proposed in recent studies with promising results in selected patients.
Key Words: Neuroendocrine neoplasms; Gastrointestinal endoscopy; Endoscopic resection;Endoscopic ultrasound; Ablative technique; Tissue acquisition
lNTRODUCTlON
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) are rare neoplasms arising from neuroendocrine cells distributed in the GEP tract. Most commonly, the primary lesion is located in the gastric mucosa, small and large intestine, rectum, and pancreas[1].
The incidence of GEP-NENs has substantially increased over the last decades. Data from the Surveillance, Epidemiology, and End Results registry show that the incidence of GEP-NENs has increased 6.4 fold since the program’s inception in 1973. This phenomenon may be related to the increasing number of radiological imaging and endoscopic examinations performed[1,2].
Approximately 15%-30% of GEP-NENs are functioning tumors with hormone-related symptoms; the remaining 70%-85% are nonfunctioning and detected incidentally or because the patient has symptoms of mass effects or distant metastases[3]. The management of GEP-NENs requires a multidisciplinary approach. Since GEP-NENs are less frequent than other malignancies, endoscopic management of these tumors may not be fully understood.
This review focuses on the endoscopic diagnosis and treatment of GEP-NENs.
Site
The GEP tract represents the most common localization of NENs. Gastrointestinal NENs (GI-NENs)develop from the stomach (23%), appendix (21%), small bowel (15%), and rectum (14%). Esophageal and colonic NENs are rare tumors that account for a small percentage of GI-NENs. Pancreatic NENs(Pan-NENs) represent about 1% of all pancreatic neoplasms but their prevalence is around 10%[1].
Grade
The World Health Organization subclassifies GEP-NENs based on the mitotic count and Ki-67 index(Table 1). This classification defines both well-differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs). NETs are divided into grade 1 (Ki-67 index < 3,mitotic rate < 2), grade 2 (Ki-67 index 3-20, mitotic rate 2-20), and grade 3 (Ki-67 index > 20, mitotic rate> 20). NECs exhibit poorly differentiated morphology with significant atypia and frequently have geographic necrosis. Tumors involving both neuroendocrine and non-neuroendocrine cells are classified as mixed NENs and non-NENs[4].
Staging
There are two major classifications in current clinical use: the European Neuroendocrine Tumor Society(ENETS) tumor, node and metastasis (TNM) system and the American Joint Committee on Cancer TNM system[5,6].
Functional status
Clinically, GEP-NENs can be classified into nonfunctioning and functioning tumors. The functioning tumors secrete substances that cause appreciable clinical symptoms, whereas the nonfunctioning neoplasms do not secrete any substance or the substance produced is inactive. The hormones produced and clinical symptoms vary by site of the primary GEP-NENs. Clinical symptoms include hypoglycemic syndrome, carcinoid syndrome, Zollinger-Ellison syndrome, watery diarrhea-hypokalemiaachlorhydria syndrome, and glucagonoma (Table 2)[7].
Biomarker levels
Chromogranin A is currently the most commonly used biomarker for GEP-NENs. It has a 10%-35%specificity, and its sensitivity ranges from 32% to 92%. Serotonin and its metabolite 5-hydroxyindoleacetic acid have been measured in blood and urine samples, respectively, as markers of carcinoid syndrome. However, the sensitivity of this biomarker is as low as 35% in the absence of carcinoid syndrome[8].

Table 12019 World Health Organization classification of neuroendocrine neoplasms of the gastrointestinal tract and hepatopancreatobiliary organs
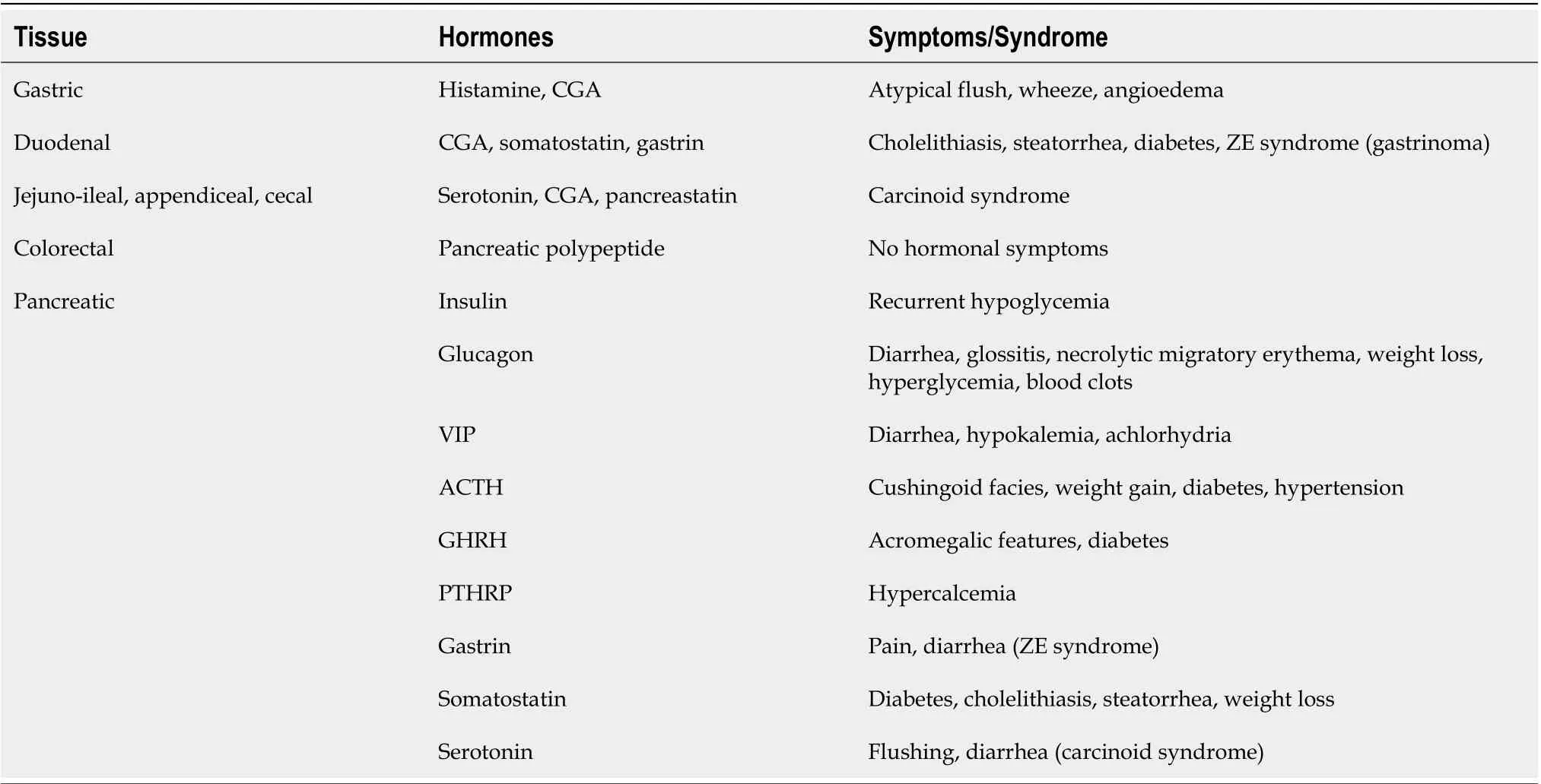
Table 2 The hormones produced by the primary gastroenteropancreatic neuroendocrine neoplasms
Several other potential biomarkers include neuron-specific enolase, human chorionic gonadotropin,alpha-fetoprotein, and pancreatic polypeptide. These circulating biomarkers are useful to aid diagnosis,but are of insufficient value to accurately identify the primary tumor site, correlate with tumor grade,and differentiate low-level malignancy from high-grade disease[9].
In recent years, new biomarkers have been evaluated that may correlate with clinical outcomes and be useful as better prognostic indicators. These include microRNAs, long noncoding RNAs, circulating tumor cells, and DNA methylation patterns[10].
Any associated syndromes
Most GEP-NENs are sporadic, but they also can arise as part of inherited familial syndromes. About 5%of patients with GEP-NENs harbor genomic mutations with well-characterized familial syndromes such as multiple endocrine neoplasia type 1 (MEN1), von Hippel-Lindau (VHL) disease, tuberous sclerosis(TSC), and neurofibromatosis type 1 (NF1)[11].
MEN1 is an autosomal-dominant syndrome, characterized by NENs of the anterior pituitary,parathyroid glands, and pancreas. VHL syndrome is an autosomal-dominant syndrome characterized by a variety of benign and malignant neoplasms including clear renal cell carcinomas, pheochromocytomas, hemangioblastomas, retinal angiomas, paragangliomas, and pNENs. TSC is an autosomaldominant syndrome characterized by widespread, low-grade tumors, and hamartomas in multiple organs including the brain, heart, skin, eyes, kidney, lung, and liver. pNENs are described in only 1% to 5% of cases. NF1 is an autosomal-dominant syndrome characterized by ubiquitous neurofibromas;multiple cafe-au-lait skin spots; and susceptibility to gliomas, myeloid leukemia, pheochromocytomas,and occasionally pNENs[12].
DlAGNOSlS
Gastric NENs
Gastric NENs (G-NENs) are neoplasms derived from the enterochromaffin-like cells of the gastric mucosa. They are classified into types I, II and III according to their clinical and pathophysiological characteristics (Table 3)[13].
Type I G-NENs correspond to the majority of G-NENs found in the stomach (70%-80%) and are associated with autoimmune chronic atrophic gastritis and hypergastrinemia, type II G-NENs lesions are caused by gastrinomas and commonly found in patients with Zollinger-Ellison syndrome (ZES) and MEN1, and type III G-NENs lesions consist of a sporadic lesion and are unrelated to gastrin hypersecretion.
Patients with G-NENs typically present with nonspecific symptoms and the diagnosis is made by upper gastrointestinal (GI) endoscopy for symptoms such as abdominal pain, nausea, bleeding, and anemia. Despite the low incidence of G-NET, recent data have demonstrated an increase due to an expanding use of upper endoscopy, improvement of endoscopes, and more attention to identification and characterization of gastric lesion[14]. Type I G-NENs occur in the corpus and/or fundus and are multiple small reddish polyps, usually subcentimetrics. They are associated with a chronic atrophic gastritis with an excellent prognosis. Tumor extension is limited to the mucosa or submucosa.
Type II G-NENs are similar to type I lesions but the adjacent gastric folds have a hypertrophic gastric mucosa and occasionally have multiple areas of ulceration of gastric and duodenal mucosa. Type II GNENs are involved in MEN1 and ZES and have a good prognosis, similar to type I. Type III G-NENs are single, large (> 2 cm), sometimes ulcerated, more aggressive and associated with local and distant spread, and involve the muscular layer (Figure 1)[15]. The prognosis of this subgroup is poor.
At the time of diagnosis, biopsy samples should be taken from the lesions and multiple gastric biopsies (antrum, body, and fundus) should be performed for etiologic orientation.
Endoscopic ultrasonography (EUS) should be performed if the lesion is greater than 1 cm in order to assess the layer of origin, tumor size, echogenicity, margins, wall invasion, and regional lymph nodes.At EUS, G-NENs present as rounded isoechoic or hypoechoic tumors, localized in the second (deeper mucosal) or third (submucosal) echo layers. EUS diagnostic accuracy for evaluation of subepithelial lesion including G-NET is suboptimal (43%-67%)[16]. EUS is a very accurate technique for assessing tumor size and muscularis propria integrity, factors that seem to condition the potential for distant metastasis[17].
In type I and II G-NENs, staging EUS is frequently performed to evaluate indication to endoscopic treatment. For patients suspected of having type II G-NENs, EUS evaluation must be performed for the assessment of any duodenal or Pan-NENs. In Type III G-NENs, EUS is indicated to stage the disease by assessing the presence of regional lymph node involvement[18].
Duodenal NENs
Duodenal NENs (D-NENs) are solitary, small lesions generally discovered incidentally on imaging studies or endoscopy. They are generally classified into five different tumor types: duodenal gastrinomas, somatostatinomas, nonfunctional D-NENs, duodenal gangliocytic paragangliomas, and high-grade poorly differentiated NEC[19].
Most D-NENs are localized predominantly in the first and second duodenal portion and are nonfunctioning with a low risk of local or distant metastases. Functioning D-NENs are typically associated with higher metastatic power. The presence of multiple D-NENs should raise suspicion of MEN1-ZES[19].
D-NENs located in the ampullary/periampullary region have more aggressive behavior and poorer overall survival than D-NENs located elsewhere in the duodenum[20,21].
On upper GI endoscopy, D-NENs have the appearance of submucosal tumors with a surface color often identical to the surrounding mucosa (Figure 2). As the tumor enlarges, a depression may form in the center, which is eventually replaced by an ulcer crater[22].
EUS evaluation is useful for duodenal subepithelial lesions characterization; the accuracy of combined endoscopic/EUS imaging for all duodenal lesions is 84.9%[23].

Table 3 Characteristics of the subtypes of neuroendocrine neoplasms of the stomach

Figure 1 Gastric neuroendocrine neoplasm. A: Endoscopic image demonstrates a flat lesion in the stomach fundus with depressed center; B: Endoscopic en bloc resection was achieved.
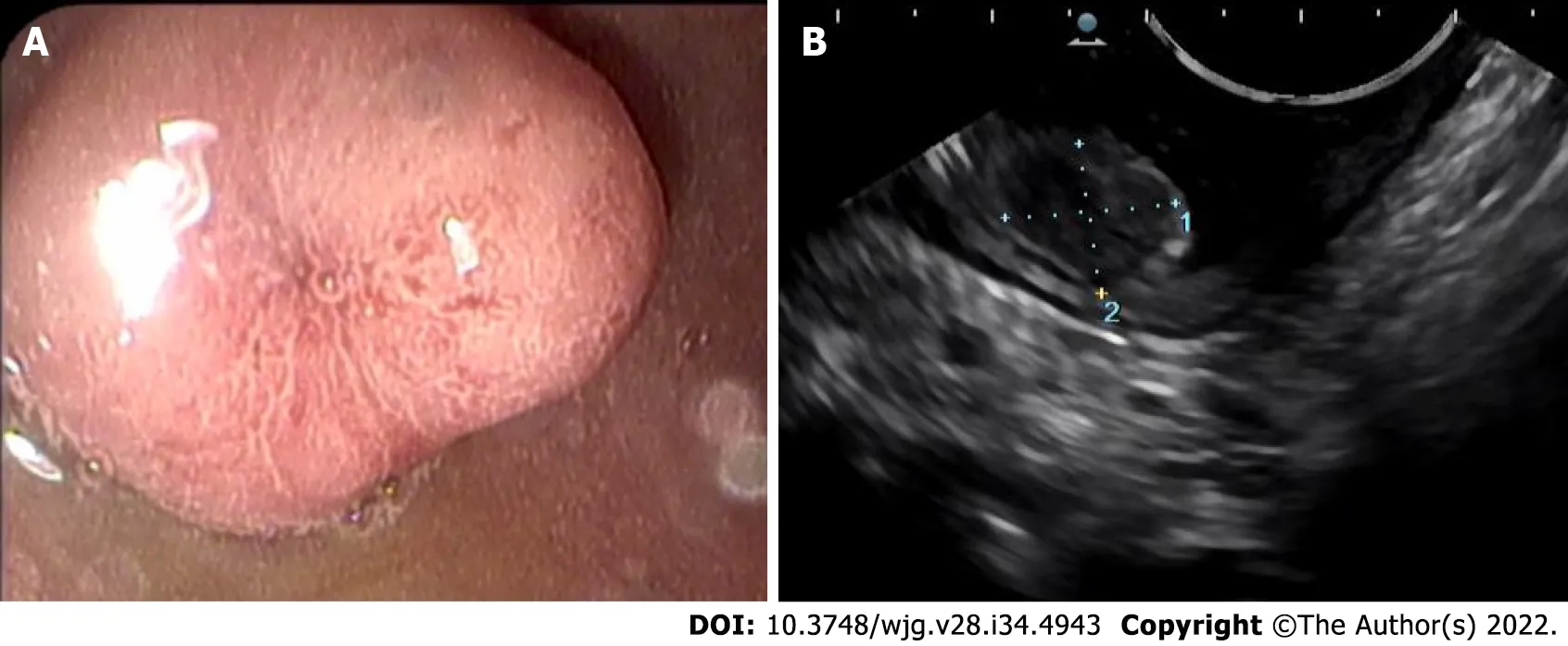
Figure 2 Duodenal neuroendocrine neoplasm. A: Endoscopic image demonstrates a sessile polyp with central depression; B: Endoscopic ultrasound demonstrates a hypoechoic intramural structure in the submucosal layer of the duodenal wall.
EUS is also useful to exclude locoregional lymph node metastases and thus the indication for endoscopic mucosal resection in case of lesions > 1 cm. At EUS evaluation, D-NENs are usually located in the submucosal layer and are rounded, hypoechoic, well-demarcated small lesions. Fine needle aspiration (FNA) should also be performed in cases of nondiagnostic histopathology[18]. Duodenoscopy and EUS are indicated to identify the primary tumor in the case of ZES and in patients with MEN1[24].
Small bowel NENs
Small bowel NENs (SB-NENs) are the most common NENs developing distant metastases; however,their prognosis remains favorable[25]. They tend to present in later stages because clinical symptoms are often insidious and the diagnosis often occurs in the course of an intervention for intestinal obstruction or bleeding[26].
Accurate localization and staging of SB-NENs often involve a combination of several imaging modalities. Endoscopic examinations such as capsule endoscopy and double-balloon enteroscopy are useful in identifying occult SB-NENs when no primary tumor was found on conventional imaging.Macroscopically, most SB-NENs are sessile nodules or ulcerated lesions usually measuring between 1 and 2 cm or as multiple tumors[27,28].
Appendix NENs
Appendiceal NENs (A-NENs) are usually discovered incidentally at final pathological examination after an appendectomy is performed for acute appendicitis. Colonoscopic examination of the entire large bowel is mandatory given the frequency of synchronous colorectal neoplasia[27]. A-NENs usually have a good prognosis. In most cases, appendicectomy alone is considered curative; however, in selected cases with high malignant potential, the right hemicolectomy could be considered[29].
Colorectal NENs
Colonic NENs (C-NENs) and rectal NENs (R-NENs) are two different clinical entities. C-NENs have more aggressive features and much worse prognosis than R-NENs[30]. Nearly 70% of C-NENs are located in the ascending colon, particularly in the cecum with a mean size of 5 cm at presentation. The patients generally experience late symptoms such as abdominal pain, GI bleeding, and weight loss, and most of them have local or distant metastasis[15].
Most R-NENs are diagnosed through screening sigmoidoscopy and/or colonoscopy while only a small fraction have symptoms such as diarrhea, abdominal pain, or rectal bleeding.
The majority of R-NENs are small size lesions less than 1 cm and only 5% present are larger than 2 cm[31].
Endoscopically, R-NENs appear as sessile or semipedunculated polypoid lesions with normal or a yellow-discolored mucosa, frequently located in the midrectum. Larger lesions can have different endoscopic characteristics such as ulcerations, depressions or hyperemic color, which can be suggestive of aggressive disease[30].
At EUS, R-NENs have the aspect of nodular, hypoechoic, or isoechoic submucosal tumor clearly demarcated from the surrounding tissue[18].
EUS-FNA can be helpful to make a differential diagnosis with other subephitelial lesion[32] with a diagnostic accuracy of 85.1%[33].
According to the current ENETS consensus, an EUS should also be performed in order to assess the depth of rectal wall invasion and regional lymphadenopathy prior to endoscopic resection[34].
A complete colonoscopy is indicated after a diagnosis of a R-NENs to exclude concomitant colon cancer and other NENs[35].
Pan-NENs
Pan-NENs comprise 1% to 2% of pancreatic neoplasms[36]. Pan-NENs are classified as functioning or nonfunctioning depending on whether they cause hormonal overproduction syndrome. Functioning Pan-NENs include insulinoma, gastrinoma, VIPoma, and glucagonoma. Nonfunctioning Pan-NENs comprise the largest group of Pan-NENs and do not produce syndromes of hormonal excess. Nonfunctioning Pan-NENs often manifest later in the course of the disease or are discovered incidentally during abdominal imaging examinations performed for other diseases[37].
EUS is a very useful tool in the management of Pan-NENs and has been considered the imaging study of choice to be performed after other negative noninvasive imaging studies are negative[38].
Puliet al[39] assessed the diagnostic accuracy of EUS for detection of Pan-NENs. This meta-analysis demonstrated an excellent accuracy of EUS in this setting with a sensitivity of 87.2% and a specificity of 98.0%.
A meta-analysis of 2015 assessed incremental benefit of preoperative EUS for the detection of suspected Pan-NENs after other investigative modalities have been attempted. EUS increased the overall Pan-NENs detection by over 25% and was particularly useful in functioning Pan-NENs,typically smaller in size (i.e.insulinomas or gastrinoma)[40].
EUS is also very useful in assessing the presence of multiple lesions, size lesion and especially the distance between the lesion and the main pancreatic duct, a factor that can drive the decision on which surgical approach (i.e.enucleationvsresection)[18]. Pancreatic enucleation is commonly performed for Pan-NENs with a low risk of malignant progression but post-operative pancreatic fistula risk is higher for neoplasms located close to the duct[41].
EUS is of course useful for differential diagnosis of Pan-NENs with other solid pancreatic lesions.Pan-NENs are solid lesions and on EUS examination, appear as well-demarcated, hypoechoic lesions with a homogeneous pattern. However, because Pan-NENs grow expansively, they may also appear as cystic or indistinguishable from pancreatic adenocarcinomas.
In Pan-NENs EUS guided tissue acquisition is considered the procedure of choice to reach cytologic diagnosis, but also ascertainment of tumor grade by determining the Ki-67 proliferation index and mitotic count (Figure 3).
EUS-FNA provides a cytological specimen with a sensitivity ranging between 80% and 90%,specificity at 96%[18]. The adequacy and concordance of Ki-67 evaluation of EUS-FNA compared with histology remains unclear especially for tumor > 20 mm[42,43]. To overcome these limitations of cytological Ki-67 determination, sampling with needles for EUS-guided fine-needle biopsy (EUS-FNB)have been introduced with good results[44,45]. In a recent retrospective study EUS-FNB outperformed EUS-FNA for Ki-67 proliferation index determination[46].
EUS elastography (EUS-E) is a newer tool of diagnostic EUS for differential diagnosis of solid pancreatic lesions. It is a technique that analyzes pancreatic stiffness being a useful tool for the differential diagnosis of pancreatic masses with a qualitative or quantitative elastographic assessment. A meta-analysis by Zhanget al[47] showed a sensitivity and specificity of quantitative EUS-E for the differentiation of benign and malignant pancreatic masses of 0.95 and 0.61, respectively. Iglesias-Garcíaet al[48] evaluated the accuracy of quantitative EUS-E for the differential diagnosis of solid pancreatic masses. EUS-E was helpful in differentiating pancreatic cancer from Pan-NENs with a sensitivity of 100% and a specificity of 88%. In another study, elastographic analysis was accurate in discriminating between benign and malignant pancreatic lesions, without difference between NENs and other nonmalignant lesions[49].
Recently, shear wave elastography (SWE) has been introduced as a quantitative absolute measurement of tissue hardness. Ohnoet al[50] compared the diagnostic performances of EUS-SWE and conventional strain elastography for solid pancreatic lesions without significant differences.
To date EUS-E does not provide sufficient diagnostic accuracy to replace tissue diagnosis but it plays a significant role in those cases of suspected pancreatic cancer where biopsy sampling was inconclusive and can help to select the area of the pancreatic lesion to be sampled[51].
Contrast-enhanced EUS (CE-EUS) consists of an intravenous injection of contrast media during the EUS examination so parenchymal perfusion and the microvasculature of the pancreas can be visualized.Pancreatic cancer is observed as a hypoenhanced heterogeneous lesion whereas Pan-NENs are observed as well-demarcated lesions with hyperenhancement in the arterial phase.
CE-EUS increased the accuracy of EUS for both the detection and characterization of solid pancreatic lesions[52].
Kitanoet al[53] prospectively evaluated how accurately CE-EUS characterizes pancreatic lesions and hyperenhanced lesions were diagnosed as Pan-NENs with a sensitivity of 79% and specificity of 99%.Several studies have examined CE-EUS in the differentiation between malignant and benign Pan-NENs[39,40]. Heterogeneous enhancement at an early arterial phase with fewer vessels and more fibrosis is associated with an aggressive tumor[54]. Palazzoet al[55] reported a sensitivity of 86% and a specificity of 96% in prediction tumor aggressiveness in Pan-NENs with the use of CE-EUS.
NET could be found also in the bile ducts[56]; however, the incidence is very low. In the literature,only 100 cases of biliary tree NETs were described and they have an excellent prognosis[57]. In these cases, complete surgical excision offers optimal treatment with no evidence of chemotherapy or radiotherapy’s role in the management.
ENDOSCOPlC THERAPY
In the last 10 years, the approach of GEP-NENs progressively included endoscopic resection technique.The choice of the treatment modality needs of a careful assessment and depends by multiple factors.The indication of endoscopic respective therapy does not include NET of appendix, colon and biliary tree while for pancreatic NET the suitable endoscopic approaches are ablative techniques.
G-NENs
Most type I G-NENs are limited to the mucosa or submucosa and they rarely invade the muscularis propria or metastasize to local lymph nodes if < 10 mm. Current guidelines suggested removing all tumors ≥ 10 mm[16]. EUS is recommended to identify possible involvement of regional lymph nodes and invasion beyond the submucosa prior to resection. Endoscopic resection (ER) either by endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) is the treatment of choice when EUS demonstrates the lesion to be localized to the mucosa or submucosa[58].
Surgical treatment is the option for lesions which are predicted to be T2 (lesion larger than 20 mm or grading G3) or lesions with positive margins[58].

Figure 3 Pancreatic neuroendocrine neoplasm. A: Endoscopic ultrasound revealed a 15 mm hypoechoic lesion of the pancreas; B: Stained immunohistochemically for chromogranin showing diffuse and strong positivity (original magnification 400 ×), consistent with a poorly differentiated neuroendocrine tumor infiltrating the entire thickness of the muscle tissue to the head of the pancreas; C: The proliferation index (Ki-67) < 20%.
Satoet al[59] showed in a low number of cases that about 66% of type I G-NENs resected by EMR had a positive vertical margin, whereas no case with ESD had positive vertical or horizontal margins. Kimetal[60] evaluated the clinical usefulness of ESD with that of EMR for resection of type I G-NENs with an estimated size of ≤ 10 mm. ESD yielded a significantly higher histologic complete resection rate than EMR, particularly in the vertical resection margin.
Nohet al[61] evaluated outcomes of endoscopic treatment for type 1 G-NENs below 20 mm in diameter. The complete resection rate was significantly higher in the ESD group than in the EMR group with similar procedure-related adverse events. For type II G-NENs local or limited excision can be recommended and indication for treatment type is similar to type 1 G-NENs[24,62]. Type III G-NENs are more associated with deeper invasion of the gastric wall, higher risk of nodal metastasis than type I and II G-NENs and surgery is considered the initial therapeutic approach[58]. ER has been proposed for small lesions. Kwonet al[63] investigated the clinical outcomes of type 3 G-NENs (mean tumor size of 10.2 ± 6.3 mm) after endoscopic treatment with a median follow-up of 46 mo. Of the 45 included in the follow-up, no evidence of tumor recurrence was found. Authors concluded that endoscopic treatment could be applied for type 3 G-NENs smaller than 2 cm, confined in the submucosal layer and without lymphovascular invasion. In Figure 4, we summarize the current recommendations for G-NENs.
D-NENs
Most D-NENs are located in the first or second part of the duodenum, with 20% of them occurring in the periampullary region[21]. Current guidelines indicate ER for small (≤ 10 mm) nonperiampullary DNENs confined to the submucosal layer, without lymph node or distant metastasis. Either endoscopic or surgical resection is allowed, for nonperiampullary D-NENs measuring 10-20 mm without metastatic risk (G1, no muscolaris invasion, no lymph-vascular invasion and no lymph-node metastasis)[24,58].
There are different ER techniques, such as cap technique, EMR, EMR with ligation device and ESD[58].
Ginculet al[64] evaluated the feasibility and outcome of endoscopic treatment of D-NENs (including 7 ampullary G1/G2 NETs with ≤ 20 mm) with EMR. The resection rate was R0 only in 51.6% (16/31) of patients. During a median follow-up period of 56 mo, 2 patients (8.3%) presented a tumor recurrence.Morbidity was 38 % (11/29) and mortality was 3% (one severe bleeding).
Nishioet al[65] assessed the efficacy, safety and the long-term outcomes of ESD for nonperiampullary D-NENs ≤ 10 mm in diameter. En bloc, R0 and curative resection were achieved in 100% (8/8), 88%(7/8), and 88% (7/8) of tumors, respectively. During a median follow-up of 34.0 mo none of the patients showed evidence of local recurrence or distant metastasis. Perforation occurred in 2 patients (16%)without need for surgery.
In a recent review, Britoet al[66] evaluated the effectiveness and complications of ER techniques in patients with D-NETs ≤ 20 mm. Polypectomy was associated with a high occurrence of incomplete resections. Among the mucosectomies, EMR with cap or EMR with injection was associated with lower frequencies of compromised margin and recurrent surgery. Endoscopic submucosal dissection was not associated with recurrence but it was associated with a higher occurrence of bleeding and perforation.
ER of D-NENs is complex and associated with significant morbidity. EMR is associated with a lower R0 resection rate than ESD. ESD is associated with better pathologically confirmed resection but with a higher morbidity rate and should be restricted to expert centers[67]. ESGE guidelines suggests choosing between EMR, ESD, and endoscopic full thickness resection (EFTR) to resect nonampullary, nonfunctional duodenal NENs of < 15 mm, depending on size, location, depth of invasion, and local expertise[16].
Ampullary D-NENs have a less favorable prognosis than nonampullary D-NENs and pancreaticoduodenectomy is recommended regardless of size[24].
Local resection might be sufficient for small highly differentiated ampullary D-NENs without node metastases especially in patients with comorbidities[24].
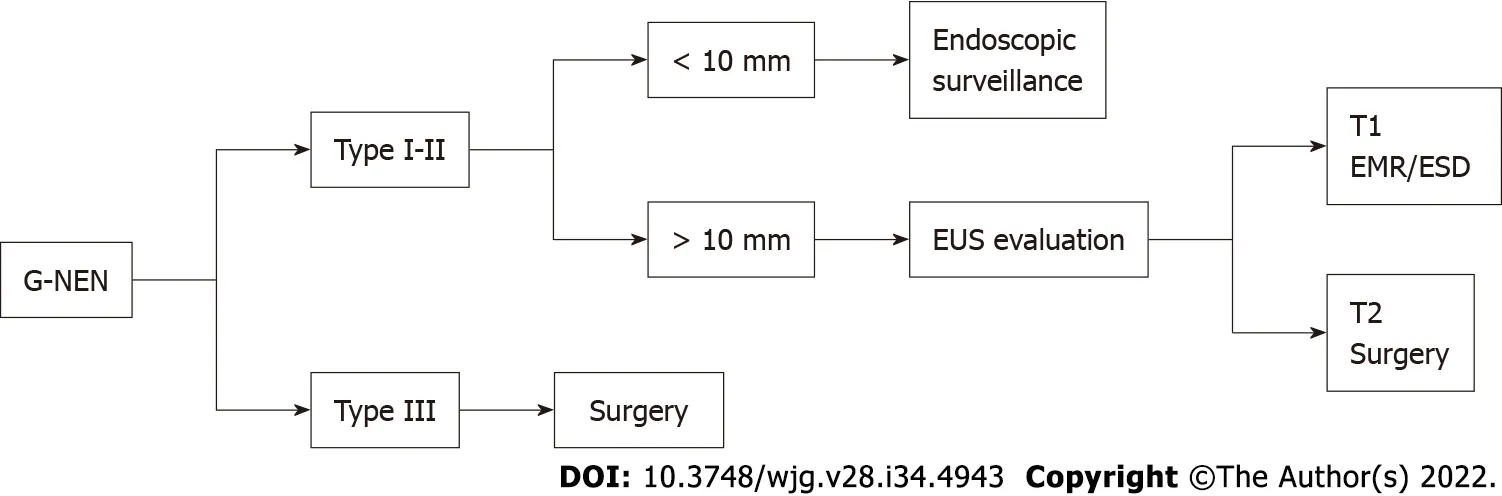
Figure 4 Algorithm for gastric neuroendocrine neoplasm management. EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection;EUS: Endoscopic ultrasonography; G-NEN: Gastric neuroendocrine neoplasm.
In one of the largest studies of EMR of D-NENs above reported, Ginculet al[64] included 7 ampullary G1/G2 D-NENs with ≤ 20 mm. In this subgroup of patients, R0 resection was achieved in 5 patients(71%) without recurrence with a median follow-up period of 56 mo.
Shimaiet al[68] reported 3 patients with an ampullary D-NENS, who underwent endoscopic papillectomy without tumor recurrence or metastasis after a follow-up of 2 years. In Figure 5, we summarize the current recommendations for D-NENs.
R-NENs
The current guidelines recommend ER for R-NENs < 10 mm in size with no risk factors for metastasis.R-NENs larger than 20 mm are candidates for surgical resection. There is controversy over R-NENs of intermediate size 10-19 mm (Figure 6). R-NENs with these sizes have a poorer prognosis compared with those < 10 mm[34]. The main factors associated with the risk of lymph-node metastases are atypical endoscopic aspect (presence of mucosal depression or ulceration), suspicious pararectal lymph node at EUS, invasion of the muscularis propria, G2, and lymphovascular invasion. Rectal NET with any risk factor for metastasis should be considered for surgical resection with lymphadenoctomy. For lesions measuring 10-19 mm without factors associated with metastatic risk the most appropriate resection techniques may be ESD or transanal endoscopic microsurgery (TEM)[24-34].
The appropriate endoscopic technique resection should allow for en bloc oncological excision.Optimal endoscopic treatment modality for R-NENs has not yet been achieved.
Conventional polypectomy is associated with a low rate of complete resection as most of the R-NENs are submucosal. Sonet al[69] reported a complete resection rate by conventional polypectomy of 30.9%.
EMR is simple and has low complication rates but can sometimes cause incomplete resection and difficulty in pathologic evaluation because even small R-NENs can invade the submucosa. Several studies, assessing efficacy of EMR, have reported complete resection rates ranging from 30%-70%[70-74].
Therefore, several m-EMR methods have been reported and included cap-assisted EMR (EMR-C),EMR with a ligating device (EMR-L), and EMR after circumferential precutting (EMR-P).
EMR-L is performed suctioning the lesion into the ligating device and cutting by using a round snare after placing bands around the base of tissue suctioned. EMR-C is performed with a transparent cap fitted to the scope, followed by snare cautery resection. These techniques allow the cutting of the submucosal layer from the muscularis propria[75].
Leeet al[75] performed a retrospective study comparing EMR-L and EMR-C, concluding that EMR-L may achieve both a higher endoscopic rate and a histologic complete resection rate. An analysis of 17 studies reported that the complete resection rate of R-NENs using EMR-L was 94.8% compared with 72.4% for EMR-C[76].
EMR-P is performed by lifting the mucosa with a saline injection, making a circumferential incision using the tip of the snare or special endoknives and resecting the tumor with a snare. This technique has the advantages, unlike the other m-EMR procedures, of not being affected by lesion size. Several studies have investigated the usefulness of EMR-P for resection of R-NENs showing a complete resection rate from 81.2% to 96.7% with a short procedure time, and an acceptable safety profile[77-79].
Recently Parket al[80] evaluated the safety and efficacy of underwater endoscopic mucosal resection in the treatment of small R-NENs (< 10 mm) with high R0 resection rates similar to ESD.
ESD is an advanced endoscopic technique employing a submucosal injection to lift the lesion away from the muscularis propria layer. Dedicated devices are then used to dissect around the entire lesion in the submucosal plane. This technique results in a high en bloc resection rate although more complicated, time consuming and with higher risk of complications than EMR and m-EMR[81].
Zhouet al[82] performed a meta-analysis comparing ESD with EMR and m-EMR in the treatment of R-NENs smaller than 15 mm in diameter. Complete resection rate was significantly higher in the ESD group than in the EMR group and comparable between the ESD group and the m-EMR group. A recent meta-analysis compared efficacy of ESD and EMR in curing R-NENs. This study showed that ESD is more effective in curing R-NENs of 10-20 mm in size than EMR without significant differences for RNENs smaller than 10 mm[83].
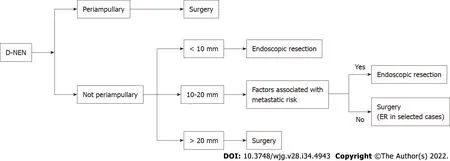
Figure 5 Algorithm for duodenal neuroendocrine neoplasms management. D-NEN: Duodenal neuroendocrine neoplasm; ER: Endoscopic resection.

Figure 6 Algorithm for rectal neuroendocrine neoplasms management. ESD: Endoscopic submucosal dissection; mEMR: Modified endoscopic mucosal resection; R-NEN: Rectal neuroendocrine neoplasm; TEM: Transanal endoscopic microsurgery.
In patients with an incomplete resection from EMR techniques, ESD may be indicated as salvage therapy[24,84].
A recent new endoscopic technique is EFTR, which is performed using a full thickness resection device (FTRD). The FTRD uses a transparent cap with a modified over-the-scope clip (OTSC) mounted over a standard colonoscope. The lesion is pulled into the cap and the pseudopolyp created by the OTSC closure is then resected with the snare preloaded in the tip of the cap. Meieret al[85] conducted a study evaluating EFTR in 40 cases of R-NENs showing effectiveness of this method (R0 resection rate in 95%) in addition to feasibility (median time, 18.5 min) and safety.
Pan-NENs
Patients with small Pan-NENs are candidates for pancreatic-sparing procedures such as central pancreatectomy or enucleation. Small Pan-NENs can be difficult to detect intra-operatively by palpation only.EUS-guided techniques to facilitate small Pan-NENs localization especially during laparoscopy surgery are tattooing or fiducial markers implantation. These techniques allow a precise localization of lesions ensuring adequate margins of resection and preserving normal pancreatic parenchyma[86].
Endoscopic ultrasound-guided fine needle tattooing (EUS-FNT) is a safe, easy to perform and useful new method to mark preoperatively small Pan-NENs. Generally, a 22-gauge standard needle allows easy injection of the tattooing solution. The needle is inserted inside the target lesion or immediately near the lesion borders into the normal parenchyma. The most frequently solution utilized is a sterile carbon-based ink which is nondegradable and remains in the tissues indefinitely[87].
Recently Rosaet al[88] evaluated EUS-FNT in facilitating intra-operative detection of Pan-NENs (8 insulinoma and 8 nonfunctional Pan-NENs.) The tattoo mark was detected in all but one patient. Only a small hematoma secondary to the EUS-FNT was observed.
The placement of fiducial markers implantation under EUS guidance is another technique to facilitate Pan-NENs localization during surgery. Fiducials are implantable radiographic markers that have been used for many years to mark soft tissue in radiology. The fiducial is easily visible during an intraoperative ultrasound[86].
Lawet al[89] reported on two consecutive patients with small Pan-NENs who underwent fiducial placement. In both of the reported cases, the fiducials were visualized by intraoperative ultrasound, and the surgical resection was successful without procedure-related complications.
In recent years endoscopic ultrasound-guided ablation therapy has emerged as a new therapeutic option for solid pancreatic tumors, especially for Pan-NENs in elderly patients and candidates unfit for surgery. There are two main techniques used, EUS-guided radiofrequency ablation (EUS-RFA) and EUS-guided ethanol ablation (EUS-EA)[90]. Functioning and multiple Pan-NENs seem to be the ideal target for endoscopic ultrasound -guided ablation therapy resolving symptomatic hormonal syndromes.In case of nonfunctioning Pan-NENs, these techniques could be a therapeutic option in the case of patients unfit to surgery[91].
EUS-EA can be safe and useful for the control of symptoms in patients with small insulinomas[91-93].
Jürgensenet al[92] reported the first case of EUS-EA of a 13 mm pancreatic insulinoma in a 78-yearold woman. The patient exhibited no further hypoglycemic episodes with no recurrence of the tumor on follow-up.
Levyet al[93] reported a small series of 5 patients for EUS-EA of insulinomas; they observed that symptomatic relief was relieved almost immediately after the procedure and maintained during the follow-up.
Qinet al[94] reported a series of 4 patients for EUS-EA of insulinomas with no recurrence of hypoglycemia and complications during follow-up.
Choiet al[95] reported the largest cohort of 32 patients with nonfunctioning Pan-NENs treated with EUS-EA. In 24 out of 40 tumors (60%) complete ablation was achieved.
The other less invasive locoregional therapy for Pan-NENs is EUS-RFA. Multiple case reports of EUSRFA of insulinomas showed complete regression of the clinical syndrome[96-98].
Regarding nonfunctioning Pan-NENs, Barthetet al[99] conducted a prospective multicenter study including 12 patients with 14 Pan-NENs (mean size 13.1 mm) treated with EUS-RFA. Among the 14 Pan-NENs, at 1-year follow-up, 12 had completely disappeared (86% tumor resolution). Two adverse events occurred (one pancreatitis, one pancreatic ductal stenosis). Another case series included 11 patients with nonfunctioning Pan-NENs. A complete radiological response was achieved in 8 of 11 patients treated with EUS-RFA. Two cases of mild pancreatitis occurred[100].
CONCLUSlON
GEP-NENs are on the rise. The reasons for this phenomenon are a better awareness of an increased and more widespread use of GI endoscopy and advanced radiological imaging[1]. The overall survival rate for patients with GEP-NENs has improved in the last years[2]. This achievement is due to both early detection and better therapeutic strategies of GEP-NENs.
Endoscopy is the only method of choice to detect asymptomatic GI-NENs at an early stage. Most patients with early, GI-NENs can be treated with ER or surveillance.
Pan-NENs are relatively rare tumors but their number is increasing, mainly because of the advances in various diagnostic imaging modalities as EUS. Newer advancement in the field of EUS such as the evolution of needles, EUS-E and CE-EUS can provide useful information with an improvement in the management of Pan-NENs. EUS-guided tumor ablation therapies can be a therapeutic option in selected patients unfit for surgery.
The literature evidence on this field is growing every day. For the nature of our study (mini-review)and the very wide issue, we collected and summarized the most important evidence regarding the endoscopic treatment underlying current guideline. We believe that a systematic review the literature with meta-analysis (when applicable) for every specific GI-NENs is needed to prove and confirm the role of endoscopy in diagnosis and therapy of many types of GI-NENs.
FOOTNOTES
Author contributions:All authors made substantial contributions to the conception of the study and literature search,drafted the manuscript or revised it critically for important intellectual content, and approved the final version of the manuscript to be published.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Giuseppe Iabichino 0000-0003-3786-7292; Milena Di Leo 0000-0002-5933-8474; Monica Arena 0000-0002-2958-3655; Giovanni Giuseppe Rubis Passoni 0000-0001-9934-8311; Elisabetta Morandi 0000-0002-5568-5831; Francesca Turpini 0000-0002-4408-0810; Paolo Viaggi 0000-0002-3467-7031; Carmelo Luigiano 0000-0001-5719-3948; Luca De Luca 0000-0002-3290-3103.
S-Editor:Zhang H
L-Editor:Filipodia
P-Editor:Zhang H
 World Journal of Gastroenterology2022年34期
World Journal of Gastroenterology2022年34期
- World Journal of Gastroenterology的其它文章
- Therapeutic strategies for post-transplant recurrence of hepatocellular carcinoma
- Pregnancy and fetal outcomes of chronic hepatitis C mothers with viremia in China
- Spontaneous expulsion of a duodenal lipoma after endoscopic biopsy: A case report
- Trends in hospitalization for alcoholic hepatitis from 2011 to 2017: A USA nationwide study
- Analysis of invasiveness and tumor-associated macrophages infiltration in solid pseudopapillary tumors of pancreas
- lmpact of adalimumab on disease burden in moderate-to-severe ulcerative colitis patients: The one-year, real-world UCanADA study
