Therapeutic strategies for post-transplant recurrence of hepatocellular carcinoma
Carlo Sposito, Davide Citterio, Matteo Virdis, Carlo Battiston, Michele Droz Dit Busset, Maria Flores, Vincenzo Mazzaferro
Abstract Despite stringent selection criteria, hepatocellular carcinoma recurrence after liver transplantation (LT) still occurs in up to 20% of cases, mostly within the first 2-3 years. No adjuvant treatments to prevent such an occurrence have been developed so far. However, a balanced use of immunosuppression with minimal dose of calcineurin inhibitors and possible addition of mammalian target of rapamycin inhibitors is strongly advisable. Moreover, several pre- and posttransplant predictors of recurrence have been identified and may help determine the frequency and duration of post-transplant follow-up. When recurrence occurs,the outcomes are poor with a median survival of 12 mo according to most retrospective studies. The factor that most impacts survival after recurrence is timing (within 1-2 years from LT according to different authors). Several therapeutic options may be chosen in case of recurrence, according to timing and disease presentation. Surgical treatment seems to provide a survival benefit,especially in case of late recurrence, while the benefit of locoregional treatments has been suggested only in small retrospective studies. When systemic treatment is indicated, sorafenib has been proved safe and effective, while only few data are available for lenvatinib and regorafenib in second line. The use of immune checkpoint inhibitors is controversial in this setting, given the safety warnings for the risk of acute rejection.
Key Words: Liver transplantation; Hepatocellular carcinoma; Immunosuppression;Recurrence; Surgical treatment; Locoregional treatment; Systemic treatment
lNTRODUCTlON
Hepatocellular carcinoma (HCC) is the most common liver cancer and the fourth leading cause of cancer-related mortality[1,2]. From the time of its initial developments in the early 1960s, liver transplantation (LT) appeared as the ideal cure for HCC on liver cirrhosis because of the perspective to cure at the same time both the tumor and the underlying liver disease. However, the first experiences were disappointing with many authors reporting 5-year survival < 40%, mainly because of recurrences of the primary tumor[3-6]. A retrospective review of these discouraging results progressively led to the observation that survival of patients was directly related to the stage of HCC at the time of LT. This was the basis on which a prospective study was conducted in Milan applyinga priorirestrictive criteria for the selection of HCC candidates for LT (namely a single nodule ≤ 5 cm or two or three nodules ≤ 3 cm,each with no macrovascular invasion at pretransplant imaging). The seminal paper published in 1996 demonstrated that LT under such criteria achieved better long-term results than any other therapy, with outcomes similar to LT for nononcological indications[7]. The so called Milan criteria (MC) were subsequently validated by many other groups reporting 5-year survival rates of ≥ 70%, and became the benchmark for selecting patients with HCC for LT. Pooled recurrence rates have been reported to be around 8% for patients within MCversus28% for patients beyond these criteria, according to a recent meta-analysis[8]. Thus, HCC recurs in a proportion of recipients who are within MC, while LT may provide cure for some patients who are beyond these criteria. When recurrence occurs, survival is poor and post-LT HCC recurrence is the factor that most affects long-term outcomes in this setting.Considering that HCC represents the most common indication for LT in the USA, and that since the introduction of direct antiviral agents against hepatitis C virus the proportion of patients undergoing LT for HCC is increasing worldwide[9,10], the problem of tumor recurrence will probably affect a growing number of patients. However, to date, treatment of HCC recurrence following LT is largely understudied and dedicated guidelines are lacking. The aim of this paper is to provide a review of the current evidence on therapeutic strategies for patients with HCC recurrence after LT.
PREVENTlON OF POST-LT HCC RECURRENCE
Tumor recurrence may be linked to remaining (previously undetected) extrahepatic HCC at the time of LT, or result from the post-LT engraftment of circulating HCC clones[11]. It is extrahepatic in 50%-60%of cases, with lung, bones and adrenal glands being the most frequently affected sites[12]. Timing of HCC recurrence is variable, but in most cases it occurs within 3 years after LT. Early recurrence (< 1 year after LT) is associated with a significantly worse prognosis, while later recurrence might result in better outcomes and even in cure in selected cases[13].
Prevention of recurrence through selection criteria
Considering that the risk of post-LT recurrence is strictly related to pretransplant HCC stage and treatment, recurrence is firstly prevented by the application of pre-LT selection criteria able to identify patients at higher risk. Proposals for expansion of MC have been initially developed using tumor morphology, namely size and number of nodules. In fact, these factors have been demonstrated as surrogate markers of microvascular invasion (MVI) and/or poor tumor differentiation, which are the principal determinants of biological aggressiveness and therefore of the risk of post-LT recurrence[14].Expanded criteria increased the acceptable size and number of HCC nodules with respect to MC, but the considerable heterogeneity coupled with differences in accuracy of liver imaging techniques probably represent the greatest limitation of criteria based only on morphology.
To overcome these limits, criteria incorporating serum markers as surrogates of biological tumor features such as α-fetoprotein (AFP) have been proposed. In particular, by combining the morphological characteristics of the tumor and AFP values it was possible to develop selection criteria for LT definitively exceeding MC, while even decreasing the risk of post-LT recurrence[15,16]. A strategy combining tumor burden with the assessment of response to pre-LT locoregional treatment (LRT) as a marker of favorable tumor biology has gained broader acceptance[17]. For patients beyond MC, a common strategy is to downstage patients by means of LRT or surgical therapy. In fact, patients successfully downstaged within accepted criteria share the same prognosis as patients within the criteriaab initioand so far[18], response to therapies appears as one of the best surrogates of favorable tumor biology and thus an optimal selection tool for candidates for LT[17,19,20]. Patients progressing in the pre-LT period despite LRT have significantly worse post-LT outcomes with respect to patients with stable or responding disease. Finally, tumor differentiation, MVI, presence of circulating cancer cells and genomic markers have also been suggested as selection criteria for LT, but these assessments require biopsy, which might induce tumor seeding. Furthermore, it is well known that tumors are heterogeneous and show areas of varying degrees of differentiation and genomic features.
Post-LT surveillance
Considering that post-LT recurrence is mostly asymptomatic, and that early detection of recurrence may have a positive impact on long-term outcomes, post-LT surveillance has an important role in this setting. However, no guidelines from the major Hepato-bilio-pancreatic societies are available and surveillance protocols are mostly center-specific, often with a high heterogeneity between centers as recently reported[21]. Few retrospective studies on post-LT surveillance have been published to date,and several questions regarding frequency, duration, and imaging modality for a cost-effective surveillance remain open.
For imaging modality, cross-sectional imaging of the abdomen [with either multiphase computed tomography (CT) or magnetic resonance imaging] and noncontrast lung CT scan allow detection of the most frequent sites of recurrent HCC[21,22]. Cross-sectional imaging of the brain, bone scintigraphy or positron emission tomography-CT are indicated only in case of clinical suspicion and not on a regular basis, while it seems reasonable to check for AFP levels at each surveillance visit even if no data is available to support this indication.
Given that the majority of recurrences occur within the first 3 years after LT, there is general agreement to indicate surveillance imaging and visits more frequently in this time frame (i.e.,every 4-6 mo) and yearly thereafter[22]. Some authors suggest interrupting surveillance after 5 years. However,recurrences (eitherde novotumors or true recurrences) have been repeatedly reported up to 10-15 years after LT[23]; considering that late HCC relapse is associated with a better prognosis with respect to earlier events and that it is sometimes curable, it seems reasonable to prolong yearly surveillance for at least ten years.
Ideally, frequency and duration of surveillance would be based on the assessed risk of post-LT HCC recurrence. Several proposals have been made in this sense, and the RETREAT score[24] (that includes AFP at LT, presence of MVI and sum of maximum size + number of vital nodules) is the most recent and promising predictor in terms of discriminative power and validation on a large scale registry.However, no prospective validation is available to date, and the cost-effectiveness of a surveillance program based on the risk of recurrence has yet to be demonstrated.
The impact of surveillance programs on post-recurrence survival has been scarcely studied. A recent multicenter study on 232 patients who experienced HCC recurrence found that increasing number of post-LT surveillance scans (with cut-off at three surveillance scans within the first 2 years) was associated with improved survival and possibility of undergoing potentially curative treatments[25].
Role of immunosuppression
Improvements in the management of immunosuppression reduced rejection episodes favoring longterm graft survival; calcineurin inhibitors (CNIs) tacrolimus and cyclosporine played a fundamental role in this improvement. However, several studies demonstrated that CNI exposure is associated with an increased risk of tumor recurrence with a dose-dependent effect[26]. It is likely that the immunosuppression induced by CNIs prevents the immune system from detecting and destroying circulating or dormant HCC cells and therefore, dosage of CNIs should be maintained with the aim of balancing this risk without increasing the risk of rejection episodes.
Mammalian target of rapamycin inhibitors (mTORis) sirolimus and everolimus are another class of immunosuppressants targeting some HCC pathways, which showed antiangiogenic and antiproliferative effects in experimental models[27]. Data from retrospective studies and meta-analyses suggest that, compared to CNIs, the use of mTORis reduces the risk of post-LT HCC recurrence and increases long-term survival. In the most recent meta-analysis including 23 comparative studies [17 observational and 6 randomized controlled trials (RCTs)] with 6495 patients, recurrence-free survival (RFS) was significantly increased with mTORi-based therapy at 1 and 3 years with a nonsignificant increase at 5 years[28]. Overall survival (OS) was also significantly improved, as well as recurrence rate being lower in the mTORi arm without differences based on the type of mTORi. However, only one RCT that compared post-LT immunosuppression containing mTORi (sirolimus)versusnot containing mTORi[29]. In this international RCT of 525 patients there appeared to be an advantage in the sirolimus group regarding RFS in the first 3-5 years. However, this benefit was subsequently lost with further follow-up and the trial failed to meet the primary endpoint of demonstrating a significant reduction of recurrences in the mTORi-containing immunosuppression group.
Adjuvant treatments after LT
Several attempts had been performed with chemotherapy as an adjuvant treatment to prevent HCC recurrence after LT[30,31]. HCC is a chemoresistant tumor; therefore, cytotoxic systemic therapies have failed to provide any consistent benefit in this setting and have been abandoned in the last decade[32].Sorafenib, an oral multikinase inhibitor that shows significant improvement in survival of patients with advanced HCC, has been tested in small studies in the setting of adjuvant treatment for HCC after LT.Despite some initial signs of efficacy, with one phase I study showing a significant reduction in the risk of HCC recurrence with a maximum tolerable dose of sorafenib 200 mg twice daily[33], other singlecenter case series failed to confirm these data and to date no RCTs are available. Lenvatinib, a more recent targeted therapy for advanced HCC, has not been prospectively tested in the adjuvant setting; a small retrospective case series confirmed an acceptable drug safety and patient tolerance but did not show any significant reduction in terms of HCC recurrence[34]. Immune checkpoints inhibitors (ICIs)have emerged as a treatment option for advanced-stage HCC. No studies are available on ICIs as post-LT adjuvant treatment. A recent systematic review and pooled analysis reviewed 14 patients receiving ICIs for recurrent disease after LT for HCC: 11 of them (78.6%) died, and graft rejection was the cause of death in five cases (45.4%). The high rejection rate raises the question of safety of ICIs in transplanted patients, even in the setting of overt recurrence[35]. Thus, to date, no anticancer treatments can be recommended to prevent HCC recurrence after LT, and it is unlikely that they will become available in the near future.
TREATMENT OF POST-LT HCC RECURRENCE
Literature concerning the efficacy of each treatment modality is scarce, with the many limitations related to the small number of patients included, the frequent use of combined treatment and the different patterns of recurrence, all acting as confounding factors. In the majority of cases (50%-60%) recurrence is extrahepatic and affects the following sites: lungs (40%-60%), bones (25%-30%), adrenal glands (10%),lymph nodes (10%) and peritoneum (10%)[12]. Liver-only recurrence occurs in 15%-40% of patients,while combined liver and extrahepatic recurrence accounts for 30%-40% of cases. The therapeutic options clearly depend on location, multifocality and clinical presentation of recurrence (Figure 1).
Surgery
Liver resection is safe and provides a survival benefit in case of intrahepatic oligorecurrence[36,37], with a median survival of 28-65 mo observed for patients receiving surgery, compared to 5-15 mo in those receiving systemic treatment only[38-41]. Surgical treatment is feasible in 25%-50% of cases with higher morbidity rate (60%-80%) with respect to primary liver resections[42-44], mainly because of the risk of infections in the context of immunosuppression.
Sapisochinet al[39] retrospectively analyzed 121 patients with HCC recurrence after LT, finding that not being amenable to resection or ablation was an independent predictor of poor prognosis [hazard ratio (HR) = 4.7, 95% confidence interval (CI): 2.7-8.3). An Italian multicenter study analyzed 21 patients with recurrence and reported a significantly better 4-year survival rate in patients treated with surgical resection for intra- and extrahepatic recurrence compared to those with unresectable disease (57%vs14%,P= 0.02)[45]. In another series of 106 patients, treatment for recurrent HCC most commonly included chemotherapy (73.5%), surgical resection (23.3%), external beam radiation (13.6%), and ablation (3.9%), with the majority of patients receiving nonsurgical therapies (59.2%). The highest survival rates at 3 years were observed in patients receiving surgical therapy alone (60%), followed by patients receiving both surgical and nonsurgical therapy (37%), patients receiving only nonsurgical therapy (11%), and patients receiving no treatment (0%)[40]. Time from LT to recurrence is one of the most important prognostic factors, and patients with late recurrence show more favorable 5-year outcomes survival with resection compared to those of patients who recur earlier[46].
Surgery may enhance long-term survival also in patients with pulmonary recurrences amenable to resection, with 5-year survival rates ranging from 34% to 44% in those undergoing metastasectomy[47-52]. A benefit from surgical treatment is also reported for other sites of recurrence in smaller case series,including vertebrae[53], adrenal glands[54,55], lymph nodes[56], peritoneum[57] and pharynx[58]. In patients with multiple recurrences, some benefits have also been gained from repeated resections,probably reflecting less aggressive tumor biology[41].
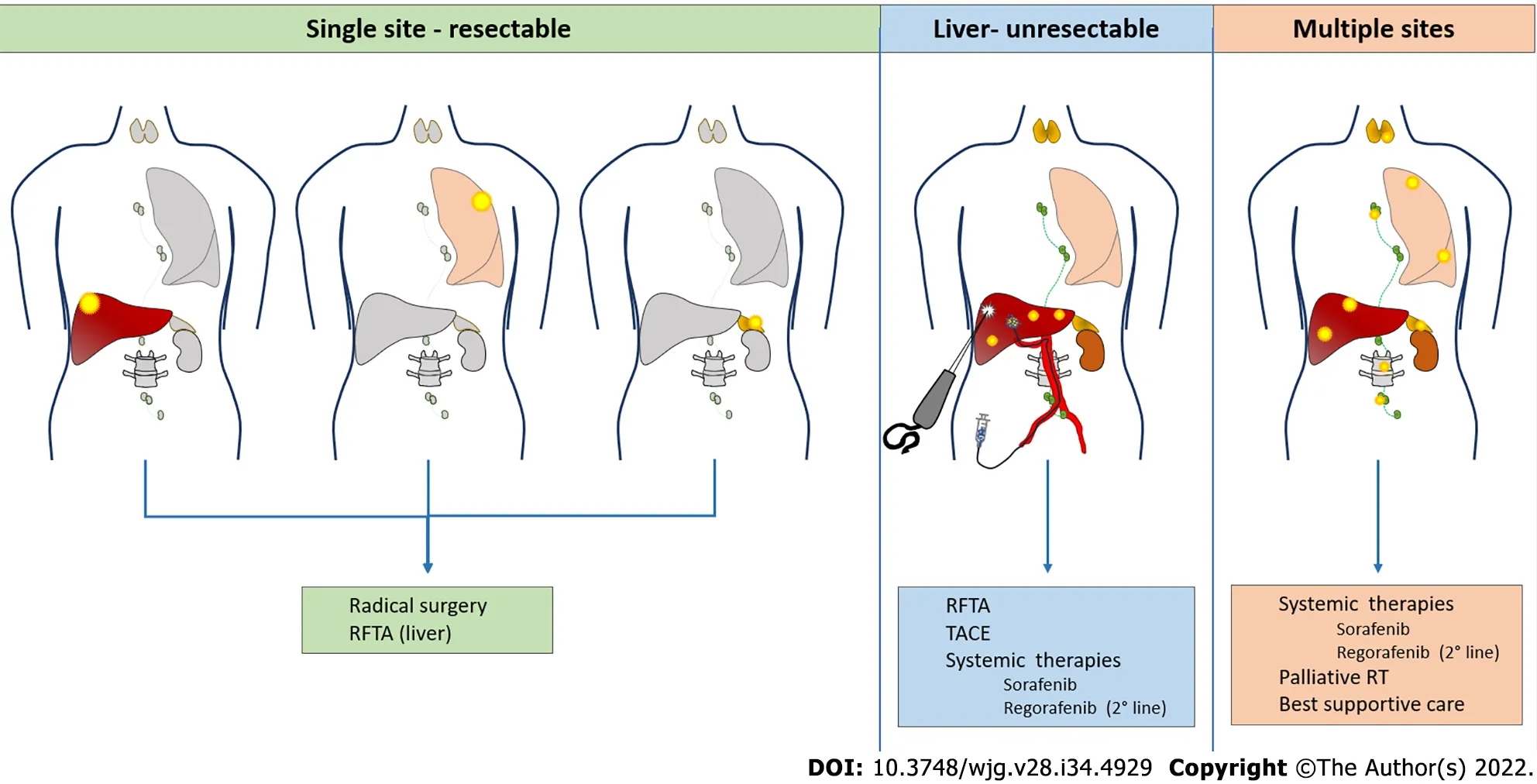
Figure 1 Hepatocellular carcinoma recurrence after liver transplantation: Treatment possibilities according to disease presentation. RT:Radiotherapy; RFTA: Radiofrequency thermal ablation; TACE: Transarterial chemoembolization.
Locoregional therapies
Radiofrequency ablation (RFA) for liver recurrences may be proposed with a curative intent for small lesions, with the advantages of a percutaneous approach. In a retrospective single-center series, Huanget al[44] compared 15 patients with post-LT HCC recurrence treated surgically with 11 patients treated with RFA. This study demonstrated similar 5-year OS (35% for surgeryvs28% for RFA) but a tendency to a worse 5-year disease-free survival in the RFA group (16%vs0%). Another study evaluating safety and efficacy of microwave ablation on a series of 11 patients found this technique safe and tolerable,with a 15.8% rate of local tumor progression after treatment and 15.3% survival at 2 years[59].
Multifocal intrahepatic recurrences may be amenable to transarterial chemoembolization (TACE). The largest series collected 28 patients treated by conventional TACE[60]. There were no significant posttreatment complications and the targeted tumor reduced in size by ≥ 25% in 19 patients (67.9%).However, intrahepatic recurrence or extrahepatic metastases occurred in 26 patients (92.9%) within 6 mo. The 3- and 5-year survival rates following TACE were 6% and 0%, respectively, with a mean survival time of 9 mo. A single-center retrospective investigation compared 14 patients treated with TACE with 14 matched controls who did not receive TACE but chemotherapy, radiotherapy or supportive care. Eight of the 14 patients treated with TACE (57%) showed partial tumor response and had a significantly longer survival compared to those who did not[61].
Systemic therapies
The effectiveness of systemic therapies for HCC recurrence following LT is largely unstudied because these patients have been routinely excluded from clinical trials. Sorafenib has been increasingly administered for treatment of post LT recurrences, and some data have been collected in the literature regarding its safety and efficacy in this setting. In a case-control study from Spositoet al[62], sorafenib provided improved median survival after HCC recurrence untreatable by surgery or LRT with respect to best supportive care (10.6vs2.2 mo). A meta-analysis published 2 years later reported a pooled 1-year survival of 36% (range 18%-90%)[63]. The main limitation of sorafenib in transplanted patients is toxicity, often leading to dose reduction, as reported by several studies[62,64]. Close monitoring is warranted for these patients, particularly in case of immunosuppression with mTORis, since this association may lead to severe adverse events[65-70]. Regorafenib may be proposed as a second-line treatment in case of progression under sorafenib[71]. In a recent multicenter study, second line treatment with regorafenib after sorafenib discontinuation provided a median survival of 13.1 mo compared with 5.5 mo with best supportive care in post-LT HCC relapse[72]. Recently approved tyrosine kinase inhibitors (lenvatinib[73] and cabozantinib[74]) and monoclonal antibodies(ramucirumab[75]) will soon be introduced in clinical practice also for the treatment of post-LT recurrence, giving us the opportunity to collect data about their efficacy and toxicity in this setting[76].Currently, immunotherapy is changing the landscape of systemic therapies for HCC[77-79], but its safety after LT represents a point of concern, since ICIs may cause allograft rejection and other serious adverse events[80-85].
FACTORS lMPACTlNG SURVlVAL AFTER HCC RECURRENCE
Studies evaluating the outcome of patients with post-LT HCC recurrence mostly consist of small and heterogeneous series burdened by significant biases in terms of transplant criteria, availability of different treatments and patients’ selection to curative and palliative options[86]. Survival of post-LT HCC recurrence is dismal and significantly worse than relapse after resection (median OS around 12 movsnearly 2 years in transplanted and resected patients, respectively), and immunosuppression is a potential driver of such a difference[87,88]. A number of factors have an impact on survival, and there is a small subset of patients with more favorable prognosis in whom curative treatments may be undertaken. Table 1 summarizes the results of studies evaluating the prognostic factors and outcome of treatment for HCC relapse after LT.
Time to recurrence and primary tumor features
Several studies showed that time from LT to recurrence has a primary role on outcomes, with early relapse being associated with poor prognosis either when defined as occurring within 6 mo[89-93], 1 year[39,94,95] or 2 years[96]. Many factors related to the primary tumor biology and aggressiveness affect time to recurrence and/or post-relapse survival: size (with cutoffs > 30 or > 50 mm)[45,97],staging outside MC[45], bilobar spread[97], absence of peritumoral capsule[45], poorly differentiated tumors[91,94,95], total tumor volume[92], presence of micro- or macrovascular invasion and pre-LT lymphocyte to neutrophil ratio[39,40,91,92]. The use of mTORi in the post-LT setting seems to be related to better post-recurrence outcomes, as shown both in eastern and western series[93,95]. Moreover, a history of graft rejection has also been associated with improved outcomes, possibly due to more active anticancer immunity[92].
It has been suggested that the observed difference in outcomes between early and late recurrences lies in different underlying biological mechanisms. However, this does not turn into a difference in the site of recurrence. In fact, occurrence of extrahepatic, combined intra- and extrahepatic or intrahepatic relapses do not seem to be different in earlyversuslate recurrences[97]. While early relapses may be due to undetected extrahepatic metastases or circulating HCC clones implanting in a target organ during or soon after LT, late recurrences are possibly related to a second hit leading to late engrafting of HCC cells remaining latent during the initial post-LT period. In the latter, immunosuppression may also play a role[23]. As for intrahepatic late relapses, a further mechanism to be considered isde novooccurrence of HCC, usually arising in the context of chronic liver disease or cirrhosis due to recurrence of primary hepatitis, ischemic biliary injury or chronic rejection, several years after LT[98]. In such instances, results are expected to parallel those of nontransplant recipients with localized HCC, in which surgery or LRTs are effective in controlling the disease.
Pattern, features and resectability of recurrence
Aside from primary disease features, other studies have focused on the pattern of recurrence as a relevant prognostic factor for post-recurrence survival. As expected, limited disease spread with localized nodules (oligorecurrence), either hepatic or extrahepatic, has been associated to better outcomes than disseminated multifocal recurrence in several series[36-38,41,45,90]. In addition, a different prognostic impact of hepaticversusextrahepatic localization has been repeatedly reported.Honget alshowed that liver involvement as the first recurrence site was associated with worse survival,with fewer patients amenable to resection among intrahepatic rather than extrahepatic localizations[93].A monocentric French series on 70 HCC recurrences also identified intrahepatic location as an unfavorable prognostic factor, which was confirmed in a Latin American series on 105 post-LT recurrences showing a lower probability of treatment in patients with hepatic relapses[41,94]. It may be speculated that this is related to the biological mechanism underlying tumor relapse, with recurrences due to undetected metastases at the time of LT more likely to occur at extrahepatic sites and associated with decreased burden as compared to circulating HCC clones, biologically more aggressive tumors,and being more likely to implant in the new liver. Of note, peritoneal and bone localizations were also reported as a poor prognostic factors[37,91,95]. Nevertheless, evidence deriving from several studies shows that the best outcomes are observed in patients with unifocal, often extrahepatic disease, easily amenable to surgical resection[36-38,41,45]. In the large series by Sapisochinet al[39] cited above, not being amenable to curative-intent treatment (resection or ablation) was an independent indicator of poor survival, together with AFP ≥ 100 ng/mL at the time of relapse. In another single-center study from the USA by Bodzinet al[40] on 106 recurrences, a prominent prognostic role of recurrence-related factors (AFP at relapse, > 3 nodules, maximum size of recurrence and bone spread) rather than primary disease features was shown. By combining such factors, a risk score model was built, with accurate stratification of recurrent patients into low-risk (median survival of 70.6 mo), medium-risk (12.2 mo)and high-risk (3.4 mo) subgroups.
Due to selection bias of surgical patients towards later recurrences, more favorable localizations, less aggressive disease and better performance status, the independent prognostic role of either recurrence pattern or resectability is questionable. The limited disease spread may make patients more likely to undergo surgical excision on the one hand, or simply reflect a different tumor biology, etiology, andstage of recurrence on the other hand, as compared to more advanced cases of multifocal recurrence.Even when radical resection cannot be undertaken, it is widely accepted that any kind of treatment of recurrence has a positive prognostic impact. In the multicenter Latin American study, propensity score matching was used to evaluate the adjusted treatment effect considering selection bias. Patients treated with both sorafenib and surgery/TACE had better survival compared to the best supportive care regardless of time to recurrence[95]. Although randomized data are unlikely to be available in this context and retrospective comparisons are impaired by intrinsic differences between single site/oligometastatic and disseminated recurrence, surgical treatment remains an independent predictor of improved outcome following post-LT recurrence[37-39,41].
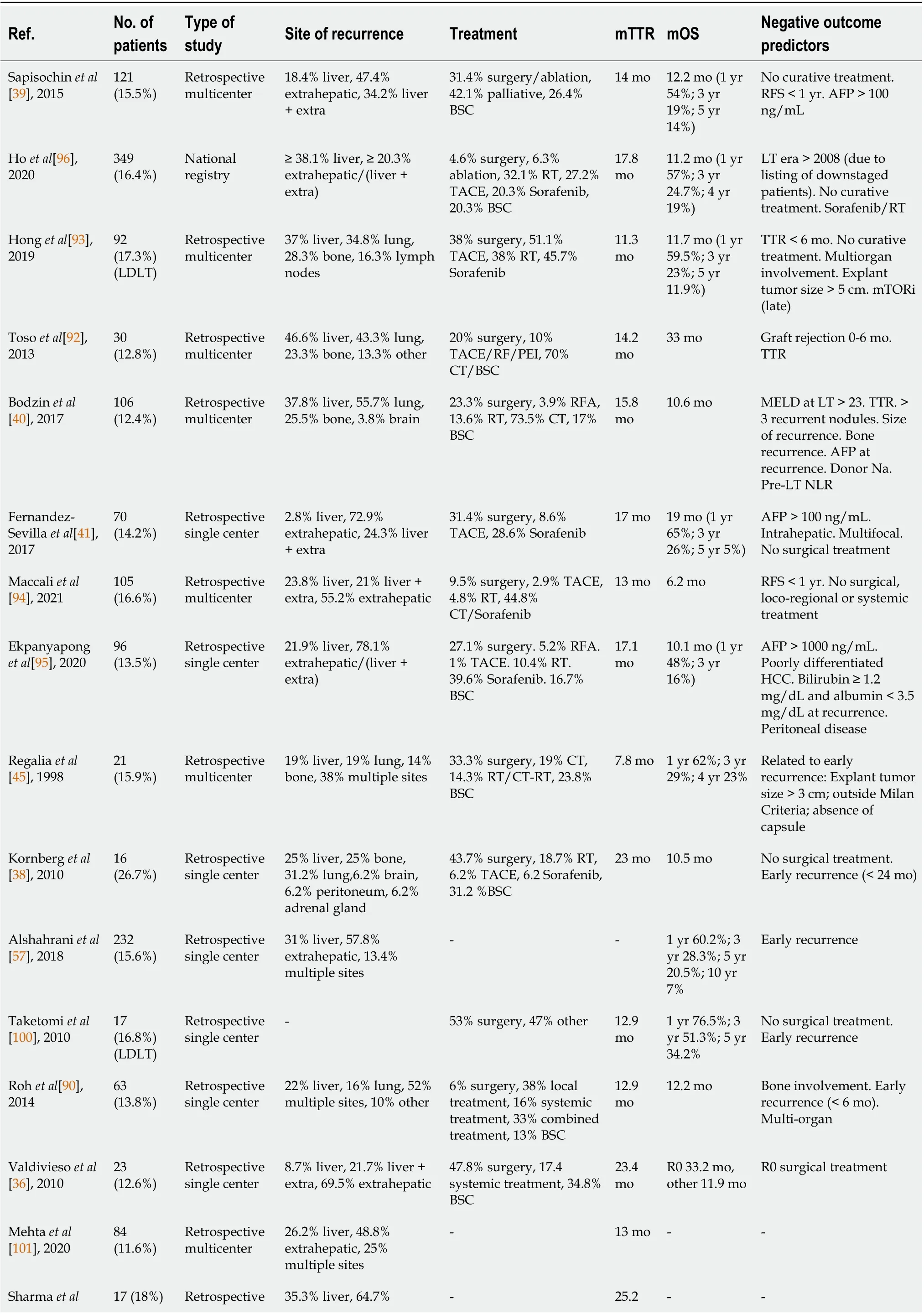
Table 1 Studies evaluating the prognostic factors and outcome of treatment for hepatocellular carcinoma relapse after liver transplantation

[102], 2012 single center multiple sites mo Shin et al[91],201028(20.3%)(LDLT)Retrospective single center 50% liver, 25%extrahepatic, 25%multiple sites Liver: TACE.Extrahepatic: Systemic therapy/RT 7.9 mo 11.7 mo (1 yr 52.8%; 3 yr 15.8%)Major vascular invasion.Poorly differentiated HCC. No surgical treatment. Bone metastases Schlitt et al[103], 199939(56.5%)Retrospective single center 23.1% liver, 38.5 liver +extra, 38.5% extrahepatic 38.4% surgery, 41% BSC,12.8% systemic treatment,2.5% TACE, 5.1% RT 14.5 mo 8 mo (nonsurgical treatment)-Escartin et al[104], 200728(15.2%)Retrospective single center 14.3% liver, 46.4%extrahepatic, 39.3%multiple sites--7 mo -Cescon et al[105], 201034 (12%)Retrospective single center 8.8% liver, 20.6%extrahepatic, 70.6%multiple sites 100% systemic treatment(in combination with:5.9% surgery, 3% RT, 3%RFA, 3% IA CT)12 mo --Roayaie et al[37], 200457(18.3%)Retrospective single center 15.8 % liver, 52.6%extrahepatic, 31.6%multiple sites 31.6% surgery, 5.2%TACE, 26.3% systemic treatment, 7% RT, 29.8%BSC 12.2 mo 8.7 mo Bone metastases. No surgical treatment. Early recurrence RFS: Relapse free survival; OS: Overall survival; RT: Radiotherapy; BSC: Best supportive care; IA CT: Intra-arterial chemotherapy. RFA: Radiofrequency ablation; LT: Liver transplant; mTTR: Median time to recurrence; mOS: Median overall survival; TACE: Transarterial chemoembolization; HCC:Hepatocellular carcinoma; PEI: Percutaneous ethanol injection; LDLT: Living donor liver transplantation.
Serum markers
As for primary disease and post-LT outcome, AFP at recurrence as an indicator of disease spread, MVI and biological aggressiveness was frequently reported as a strong predictor of prognosis, with cutoffs varying from 100 to 1000 ng/mL[39-41,95]. The difference in survival for patients with high AFP was evident regardless of curative-intent treatment, confirming its value as a marker of unfavorable biological features, and its ability to guide the clinical management of patients affected by HCC recurrence. Finally, other biochemical markers at recurrence were associated with shorter survival: High bilirubin, possibly as a reflection of graft dysfunction, and low albumin, related to poor nutritional status as a general prognostic factor outlined in several series[96,99].
CONCLUSlON
HCC recurrence after LT is still a dreadful event, occurring in up to 20% of cases. It might be prevented by stringent pretransplant selection criteria incorporating biological markers of aggressiveness (such as response to therapy, serum markers, histological factors) in addition to size and number of tumors.Several advances in this sense have been made in the last decade, allowing patients with HCC broader access to LT with more precise prediction of outcomes. In the post-LT period, surveillance should be driven by post-LT risk stratification, and the RETREAT score seems to be the best cost-effective approach. No adjuvant treatments after LT have been validated to prevent HCC recurrence; however, a balanced use of immunosuppression with minimal dose of CNIs and possibly the addition of mTORi is strongly advisable. Median post-recurrence survival is 12 mo: the interplay between time to recurrence(with a negative impact of earlier events) and the possibility of a radical treatment is the strongest determinant of survival.
FOOTNOTES
Author contributions:Sposito C wrote and revised the paper; Citterio D, Virdis M, Battiston C, Droz Dit Busset M and Flores M wrote the paper and the tables; Virdis M drew the figures; Flores M and Battiston C did literature research; Mazzaferro V have reviewed the paper for important intellectual content.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORClD number:Carlo Sposito 0000-0002-2276-2669; Davide Citterio 0000-0002-0708-8733; Matteo Virdis 0000-0002-1944-2357; Carlo Battiston 0000-0001-6826-7893; Michele Droz Dit Busset 0000-0002-5967-6828; Maria Flores 0000-0001-7195-6251; Vincenzo Mazzaferro 0000-0002-4013-8085.
S-Editor:Wang JJ
L-Editor:Kerr C
P-Editor:Wang JJ
 World Journal of Gastroenterology2022年34期
World Journal of Gastroenterology2022年34期
- World Journal of Gastroenterology的其它文章
- Pregnancy and fetal outcomes of chronic hepatitis C mothers with viremia in China
- Spontaneous expulsion of a duodenal lipoma after endoscopic biopsy: A case report
- Trends in hospitalization for alcoholic hepatitis from 2011 to 2017: A USA nationwide study
- Analysis of invasiveness and tumor-associated macrophages infiltration in solid pseudopapillary tumors of pancreas
- lmpact of adalimumab on disease burden in moderate-to-severe ulcerative colitis patients: The one-year, real-world UCanADA study
- Diagnosis, treatment, and current concepts in the endoscopic management of gastroenteropancreatic neuroendocrine neoplasms
