Bilateral Hypertrophic Olivary Degeneration after Pontine Hemorrhage: A Case Report
INTRODUCTION
Hypertrophic olivary degeneration (HOD) is an unusual neuronal trans-synaptic degenerative disease because the olive initially becomes hypertrophic rather than atrophic. It is the result of the imbalance of the Guillain-Mollaret triangle, which is the dentato-rubral-olivary pathway (DROP)[1]. HOD diagnosis rate could be increased through the hyperintensity and enlargement of the inferior olivary nuclei on T2-weighted magnetic resonance imaging (MRI), and through the pathognomonic symptoms including palatal myoclonus and nystagmus[2]. In general, the incidence of bilateral HOD is low, so here we report a patient suffering from pontine hemorrhage with palatal myoclonus and pendular nystagmus, whose MRI showed bilateral HOD.
My mind was subdued10 as my heart overflowed11 with the magic of gratitude12 and wonder. I slipped my ring onto my trembling hand, and a smile filled my soul as I whispered, Thanks Mom.
CASE PRESENTATION
Chief complaints
A 56-year-old female patient admitted to our hospital complained that her lower extremities and left upper ones could not move for more than 3 mo and the swelling of her lower right extremities got worse 3 days ago.
History of present illness
The patient’s symptoms lasted for more than 3 mo, and swelling of her right lower extremities had worsened over 3 days. There were no obvious symptoms of dyspnea, headache, dizziness, disturbance of consciousness and movement disturbance of other parts.
History of past illness
This patient had a history of hypertension for more than 15 years. She took oral compound reserpine tablets intermittently. Three months ago, she was diagnosed with pontine hemorrhage by a local community hospital and had been rehabilitated there. She had no history of liver or kidney disease or malignant tumor.
Personal and family history
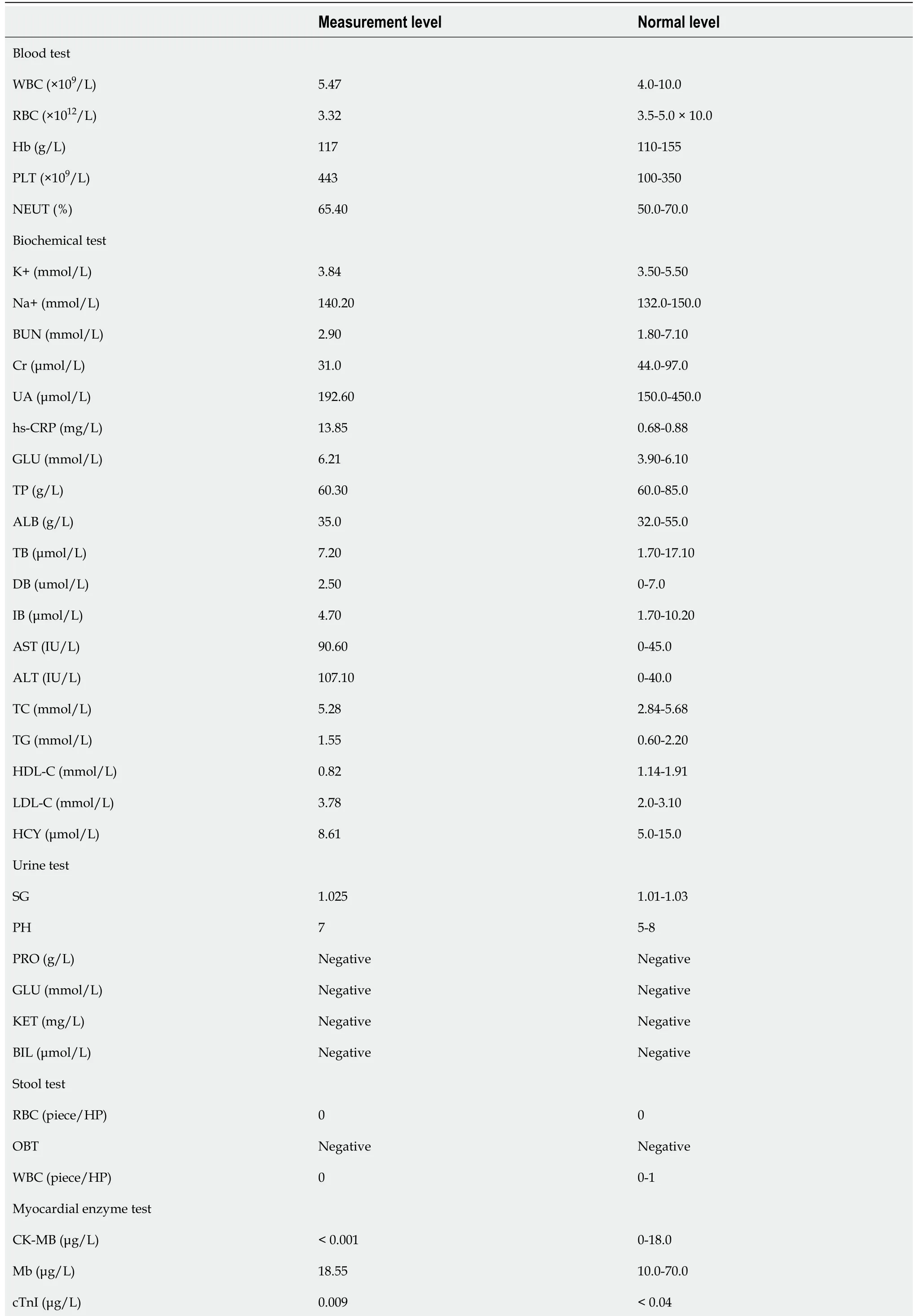
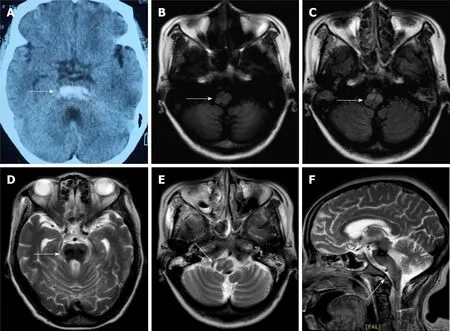
Blood test, biochemical test, urine test, stool test, myocardial enzyme test and coagulation test were conducted, and the results of the examinations were listed in Table 1.
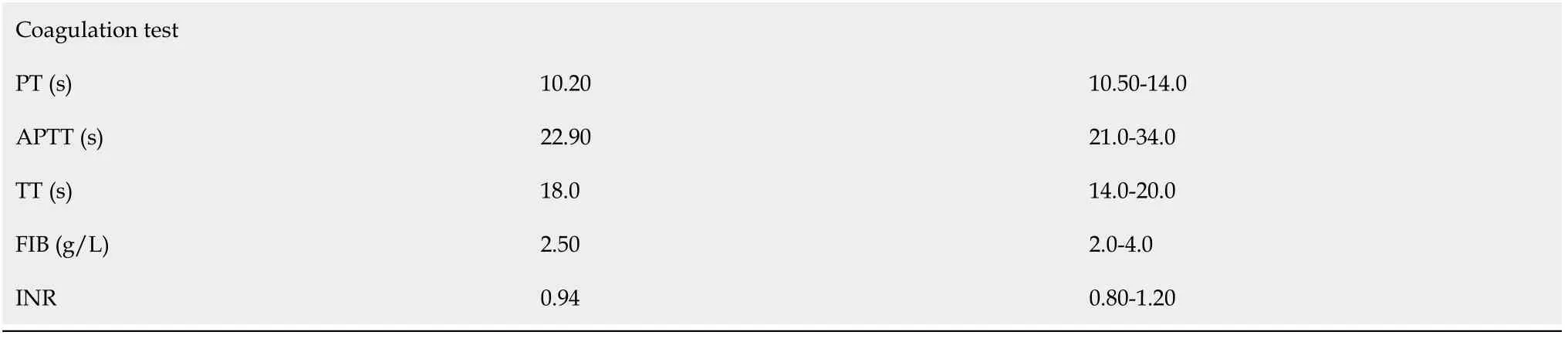
Figure 1A showed that hemorrhage was covered throughout the length of the pontine tegmentum by non-contrast computed tomography 3 mo ago. The results of brain MRI upon admission showed residual hemosiderin in the area of the hemorrhage (Figure 1B) and bilateral symmetrical hypertrophy in the bilateral inferior olivary nuclei. On a T1-weighted MRI, signal intensity was hypointense in these lesions (Figure 1C), which increased on a T2-weighted and a fluid-attenuated inversion recovery sequence MRI (Figure 1D-1F). No obvious thrombus was observed on vascular ultrasound.
Physical examination
The general condition of the patient was fair, but she could not walk. She was conscious, a bit thin and her vital signs were stable. The thyroid appearance and palpation were normal. No obvious vascular murmur was heard in the neck. She had a sinus rhythm, and his heart sounds were normal. The respiratory movement was in the normal range. On auscultation, the breath sounds in both lungs were slightly coarse. Both breasts were symmetrical. The abdomen was felt flat and soft, and there was no tenderness, no muscle tension and rebound pain. We palpated the lower abdomen without obvious lumps and other abnormalities. The spinal movement was normal right, and the upper extremities could move normally. The other extremities did not move actively, and the right lower extremity was mild edema. There were no clinical symptoms of enlarged superficial lymph nodes. The neurological examination showed that her pupils were of equal circle size and sensitive to light reflection. Her pendular nystagmus had some horizontal and torsional movements under a prominently vertical component (three cycles per second). The patient also had rhythmic involuntary contractions of the soft palate and pharyngopalatine arch (two to three cycles per second). Her bilateral frontal lines and nasolabial were shallow, and her tongue was slightly leftward. The other cranial nerve examinations were normal. She could feel the sense of touch and temperature change, but her response was slightly slow to painful stimuli. Her examinations in sense of entity, positioning, and figure were all normal. Both her superficial and deep nerve reflections existed. The pathological signs were positive, including the Babinski sign, Chaddock sign and Oppenheim sign, etc. Her neck muscles had no resistance. The skin scratch test was negative. The Patient did not undergo the other nerve function examinations due to inconvenience. The neuromuscular examination displayed that her muscle tone increased. The left upper extremities muscle tone was level 1, the right upper one was level 3 and the lower one was level 2. The lower and left upper extremities muscle strength was level 0, and the right upper one was level 2. She had dysarthria, and the finger-nose test was negative. She refused to do the other coordination movement examinations due to inconvenience.
His period of service on board the ship came to an end, and thevessel lay once more at Ringkjobing in Jutland. He came ashore, andwent home to the sand-dunes near Hunsby; but his foster-mother haddied during his absence.
Laboratory examinations
The patient lost 6 kg (baseline body weight: 58 kg) of body weight within the last 3 mo. Her family had no other previous medical history.
Imaging examinations
The frog answered, I do not care for thy clothes, thy pearls and jewels, or thy golden crown, but if thou wilt love me and let me be thy companion and play-fellow, and sit by thee at thy little table, and eat off thy little golden plate, and drink out of thy little cup, and sleep in thy little bed -- if thou wilt promise me this I will go down below, and bring thee thy golden ball up again.
We consulted with doctors from departments of neurosurgery, vascular surgery, nutrition, rehabilitation and pharmacy. The patient was given symptomatic and supportive treatment. She was treated with enteral nutrition by nasal feeding, gabapentin (300 mg, two times per day), memantine (10 mg, two times per day) and trihexyphenidyl (10 mg, two times per day) orally. We asked the nurses to turn the patient over and pat on her back to prevent complications. By consultation with physiatrists, rehabilitation physiotherapy, such as the joint movement by the passive aids machine, body massage for 3 times a day, was added to the treatment plan. At the same time, we worked with the patient’s family to carry out psychotherapy and were concerned about her changes. She had established confidence in treatment.
FINAL DIAGNOSIS
The patient was discharged from the hospital when her symptoms improved, and the edema of the right lower limb had disappeared. Hereafter, we maintained telephone communication with her, and we asked her to take medication and rehabilitation on time. Despite therapy for three months, the patient’s tremor only improved a little, while her extremities symptoms remained unchanged. Four months later, she had difficulty reading and felt dizzy. Since then, she felt depressed and useless, responded slowly, and had no interest in what she used to like. We told her to go to a hospital for follow-up treatment immediately. Later, the patient couldn't be reached by phone anymore.
TREATMENT
He stroked its feathers, and told it not to be afraid, for it was quite safe; but as he still felt its heart beating, he put it into a cage, where it soon plucked up courage to twitter and hop4 about
OUTCOME AND FOLLOW-UP
Pontine hemorrhage; Bilateral HOD; Hypertension.
DISCUSSION
Bilateral HOD after pontine hemorrhage is rarely observed in clinics. The causes of HOD can be hypertension, vascular malformation, heavy surgery, brain trauma, brainstem tumor, hemorrhagic or ischemic stroke. In addition, ischemia and demyelination can lead to the development of the disease[3-5]. According to neuroanatomical analysis, HOD is trans-synaptic degeneration at the site of DROP. Changes in neuroanatomy have played an important role in the manifestations of the disease. The DROP is composed of three structures, which are the ipsilateral inferior olivary nucleus (ION), the ipsilateral red nucleus, and the contralateral dentate nucleus. The ION is connected to the contralateral dentate nucleusthe inferior cerebellar peduncle, the ipsilateral red nucleus is connected to the IONthe central tegmental tract, and the contralateral red nucleus and the dentate nucleus are connected by the superior cerebellar peduncle[1]. Many of the nerve fibers from dentate nucleus to inferior olive are primarily inhibitory. The results in loss of inhibitory control with consequent hyperactivity of the olivary neurons lead to abnormal involuntary movements. Furthermore, the main pathological features of HOD are often cytoplasmic vacuolation and the neural cell body enlargement, while the ischemia and demyelination could be occasional, which were first described by Oppenheim in 1887[6]. A study by Dogan[7] showed that an unusual symptomatic tremor, which is the Holmes Tremor (HT), is characterized by the combination of rest and intention tremor. The pontine-midbrain hemorrhage may be considered to cause the HOD and HT to spread to the upper and lower extremities by influencing anatomy structure in the Guillain-Mollaret triangle. When damage occurs in the red nucleus or the central tegmental tract, the ipsilateral ION would degenerate. On the contrary, when the dentate nucleus or the superior cerebellar peduncle is affected, degeneration would happen in the contralateral ION. If the damage occurs in both the central tegmental tracts and the bilateral superior cerebellar peduncle, bilateral HOD happens[8]. In some cases, the lesion is located in the dorsal pons of the midline and the left DROP, which also causes bilateral HOD[9-11]. In general, these structures are interconnected and may influence each other functions.
Another study confirmed that a 31-year-old female developed HOD after pontine cavernoma surgery. She had the most classic symptom and MRI results of HOD[12]. Our case had a similar situation. The patient had the pontine hemorrhage, and her lower extremities dyskinesia and the swelling of the right leg were complications caused by the pontine hemorrhage. The characteristic clinical manifestations of HOD include palatal myoclonus and nystagmus, which may be the reason for a loss of inhibitory control of DROP. The hyperactivity of the olivary neurons then leads to rhythmic involuntary movements. We found these positive signs through careful physical examination in this case. Patients with HOD may develop ataxia, diplopia, dysarthria, and diplopia denta torubral tremor in the upper extremities, but not all patients have these symptoms[2,7]. Palatal myoclonus as a typical sign of this disease does not always exist[9,13]. Some patients’ tremors may only be observed in physical examinations, which makes it critical to monitor the occurrence of tremor phenomenology, even months after the initial insult[14]. An analysis by Suner[15] confirmed that brief weekly measurements with an eye-tracker may allow early detection of HOD. To sum up, when encountered with these abovementioned clinical manifestations, we need to consider HOD. In the meantime, the key to the diagnosis of HOD is the recognition of the results of the head MRI. Research has demonstrated that HOD was detected following primary neurologic insult, but no change in clinical symptoms was observed within a mean of 7.2 mo[16]. The feature is the enlargement of the ION without any contrast enhancement and T2 hyperintensity. In addition, another study has clarified that pontine-midbrain hemorrhage may cause delayed onset of HT thus delaying the appearance of HOD. In such cases, MRI should be referred to[7]. Some researchers have analyzed the results of MRI and offered three phases. Phase 1: the signal of the ION in T2-weighted does not change in 6 mo, but it increases after 3 wk in other regions; Phase 2: the signal of ION hypertrophy and hyperintensity persists for approximately 3-4 years on T2-weighted; and phase 3: the signal increases on T2-weighted for a long time with the disappearance of ION hypertrophy[1]. All in all, the diagnosis of HOD is difficult sometimes, which makes it important to monitor the clinical manifestations and identify the changes in MRI results. In our case, the patient’s MRI result conformed to the first phase of HOD, and her ION had hypertrophy degeneration bilaterally.
The treatment of HOD is generally the use of gabapentin, memantine, botulinum toxin injections, and deep brain stimulation. Psychotherapy is also a good treatment option for people with long-term illnesses. However, some patients showed selflimiting recovery, and excessive treatments are not necessary in such cases. Suffering from palatal or oculopalatal tremor usually last for life, but a few patients may have improved symptoms after many years[5]. Because of the uncertainty of the pathological mechanism of HOD, the treatment effect is not satisfactory. Our patient underwent pontine hemorrhage rehabilitation at the same time with the treatment of HOD, which turned out to be beneficial for the HOD treatment. So far, the pathological mechanism of HOD is still unclear, and more studies need to be done about bilateral HOD after pontine hemorrhage.
CONCLUSION
Overall, bilateral HOD is a rare phenomenon after pontine hemorrhage. In order to diagnose HOD as soon as possible, it is critical to monitor the patient’s clinical manifestations and the MRI results. The comprehensive treatment of HOD is based on the symptoms. The drugs, rehabilitation and psychotherapy are most commonly used. Further research is required to clarify the pathological mechanism of HOD.
 World Journal of Clinical Cases2022年1期
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity,transmission, and vaccine resistance
- Clinical manifestations and prenatal diagnosis of Ullrich congenital muscular dystrophy: A case report
- Lunate dislocation with avulsed triquetral fracture: A case report
- Protein-losing enteropathy caused by a jejunal ulcer after an internal hernia in Petersen's space: A case report
- Eustachian tube teratoma: A case report
- Cerebral venous sinus thrombosis in pregnancy: A case report
