Protein-losing enteropathy caused by a jejunal ulcer after an internal hernia in Petersen's space: A case report
INTRODUCTION
Internal hernias are the center of attention again as their incidence has increased worldwide with the popularization of laparoscopic surgery in what is considered a global gastrointestinal emergency[1-3]. Internal hernias were originally defined by Steinke[4] in 1932 as a state of intestinal intrusion or protrusion into an unusual fossa, fovea, or foramen in the abdominal cavity and are often found in strangulated bowel obstruction as well as after surgery for gastric cancer and obesity in Petersen’s space. This surgically created space is surrounded by the transverse colon and jejunal mesentery. Internal hernias in this space are a fairly common postoperative complication, with a reported incidence of 1.2%-2.3% after gastrectomy with Roux-en-Y reconstruction for gastric cancer[5,6]. This surgical complication causes disastrous sequelae, such as massive intestinal necrosis, fatal Roux limb necrosis, and superior mesenteric vein (SMV) thrombus[7]. Protein-losing enteropathy (PLE) is a rare syndrome characterized by a loss of serum protein in the gastrointestinal tract. It may accompany edema, ascites, pleural effusion, and malnutrition, which often complicate various diseases and make diagnosis difficult. Although there are many reported causes of PLE thus far, the rarity of the disease and the difficulty in diagnosis often make the relationship with the primary disease unclear[8]. Furthermore, it is unknown whether an internal hernia in Petersen’s space causes PLE due to delayed jejunal ulceration, even if the hernia is reduced without resection of the small intestine.
So he went to his son-in-law s room, and who should he see lying in the bed but a splendid golden man, and the rough bearskin thrown on the ground close by
Here we report the case of a patient who presented with bilateral leg edema and hypoalbuminemia 4 mo after developing an internal hernia in Petersen’s space. The etiology of this PLE was found to be a wide area of jejunal ulceration with stenosis, with the diagnosis confirmed through double-balloon endoscopy (DBE). DBE facilitated a combination of detailed observation, amidotrizoic acid radiography, tissue biopsy, and India ink injection, not only revealing a rare form of extensive jejunal ulceration after an internal hernia in Petersen's space but also proving to be an effective procedure from diagnosis to successful treatment with minimal bowel resection.
Then she began to say, Why should I not marry? But she wanted a husband who could answer when he was spoken to, not one who would stand up stiffly and look respectable--that would be too dull
CASE PRESENTATION
Chief complaints
Following an open gastrectomy for early-stage gastric cancer and a subsequent internal hernia in Petersen’s space, reduction of this internal hernia, and incident bilateral leg edema, a 75-year-old man presented at the emergency room of our medical center with a recurrence of post-surgical bilateral leg edema.
History of present illness
The patient had a history of Type II diabetes mellitus and hypertension. Apart from this, his medical history was uncomplicated before early-stage gastric cancer, with no chronic or acute major illnesses, infections, or injuries.
Approximately 3 mo after his surgery for Petersen’s hernia, the patient developed bilateral leg edema, with laboratory findings and diagnostic imaging scans described in detail below. Briefly, as a contrast-enhanced computed tomography (CT) scan showed no thrombus in the SMV but a slight thrombus in the lower limb, the patient was started on oral edoxaban. Although the etiology of this complication was not discerned, prompt recovery of his leg edema after administration of albumin solutions and diuretics resulted in early discharge. However, the leg edema resurfaced three weeks after discharge, and the patient was re-admitted for examination.
History of past illness
A 75-year-old man with a history of diabetes and hypertension had undergone an open gastrectomy for early-stage gastric cancer 1 year and 5 mo before the occurrence of an internal hernia in Petersen’s space. Following the initial surgery, he was treated conservatively on an outpatient basis without receiving chemotherapy and showed no recurrence or metastasis. At this point (1 year and 5 mo after the gastric cancer surgery), he presented at the emergency room of our medical center with complaints of mild, occasional abdominal distention and pain after meals that had mainly resolved naturally and a worrisome continued loss of appetite over approximately the past two weeks. Following imaging examinations described below, an internal hernia in Petersen's space was suspected, and laparoscopy was immediately performed. The operation revealed small intestine intrusion in Petersen's space, which was challenging to reduce laparoscopically. The patient underwent laparotomy, and the incarcerated small intestine was restored successfully, and the Petersen's defect was sutured using a non-absorbable thread. There was no necrosis of the intestine, and bowel resection was not performed. After surgery, the patient was managed with analgesia (mainly epidural anesthesia). He was administered non-steroidal anti-inflammatory drugs (NSAIDs), such as flurbiprofen axetil (twice on the day of surgery and the next day) during his hospitalization and later follow-up. Excluding a mild surgical site infection, the patient had a good postoperative course and was discharged on the fifteenth day after surgery.
Personal and family history
Who knows what may not happen before that? thought the miller s daughter; and besides, she saw no other way out of it, so she promised the manikin what he demanded, and he set to work once more and spun the straw into gold
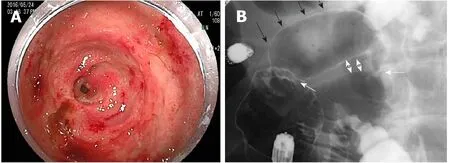
As this patient had no signs of inflammatory bowel disease (diarrhea or similar gastrointestinal symptoms), based on the previously described physical examinations, procedures, laboratory findings, and imaging scans, he was diagnosed with PLE with an alpha-1 antitrypsin clearance of 733 mL/24 h. Oral DBE revealed an extensive and continuous jejunal ulcer with circumferential stenosis and erosion extending approximately 8 cm; amidotrizoic acid radiography revealed that this stenosis and poor dilation extended approximately 6 cm (Figure 2). No signs of lymphoma or small intestine cancer were detected, and PLE was diagnosed as an extensive jejunal ulcer with stenosis, occurring as a post-surgical complication following an internal hernia in Petersen's space.
The patient’s height was 157 cm, and his weight was 51 kg. He was retired and did not have any family history of cancer or allergies to food and drugs. His medical history included Type II diabetes mellitus and hypertension, both of which were well controlled without oral treatment and insulin injection or any diet at the time of presentation. He had been taking magnesium oxide (330 mg × 6 tablets), mosapride citrate (5 mg × 3 tablets), Pancrelipase (150 mg × 6 capsules), and Kampo Daikenchuto (2.5 g × 6 packages) after surgery for gastric cancer, and he also took edoxaban for lower limb thrombosis and furosemide (20 mg × 2 tablets) and spironolactone (25 mg × 2 tablets) for the bilateral leg edema.
Oh, I must rest for a long time before I can talk, she replied, and beside, I very much doubt if you will have leisure to listen, for the affair is by no means finished
Physical examination
During the patient’s second incidence of bilateral leg edema, we performed technetium diethyl-enetriamine-pentaacetic acid human serum albumin lymphoscintigraphy, which showed accumulation in the ascending and transverse colon. However, no abnormalities were found on colonoscopy. Capsule endoscopy was performed to examine the small intestine, revealing an extensive jejunal ulcer with stenosis. The capsule was stalled by this stenosis. Oral DBE was performed to retrieve the capsule and closely examine the lesions in the jejunum, revealing continuous jejunal ulceration with circumferential stenosis and erosion extending approximately 8 cm. Tissue biopsy was performed to differentiate lymphoma and small intestine cancer, and India ink injection was used to mark the lesionDBE. Transanal DBE could not reach the jejunal ulcer and stenosis. No other lesions were found in the intestine.
Laboratory examinations
As previously described, approximately 3 mo following this patient’s surgery for Petersen’s hernia, he developed bilateral leg edema. Four months after the surgery, his serum albumin had dropped to 1.9 g/dL, and his total serum protein levels had dropped to 4.2 g/dL, resulting in admission to the hospital for additional examination. At the first incidence of leg edema, blood tests showed no liver dysfunction, and urine tests for protein were negative. In addition, no signs of lymphoma or small intestine cancer were detected by histopathology during diagnostic tests performed following the second incidence of leg edema.
Imaging examinations
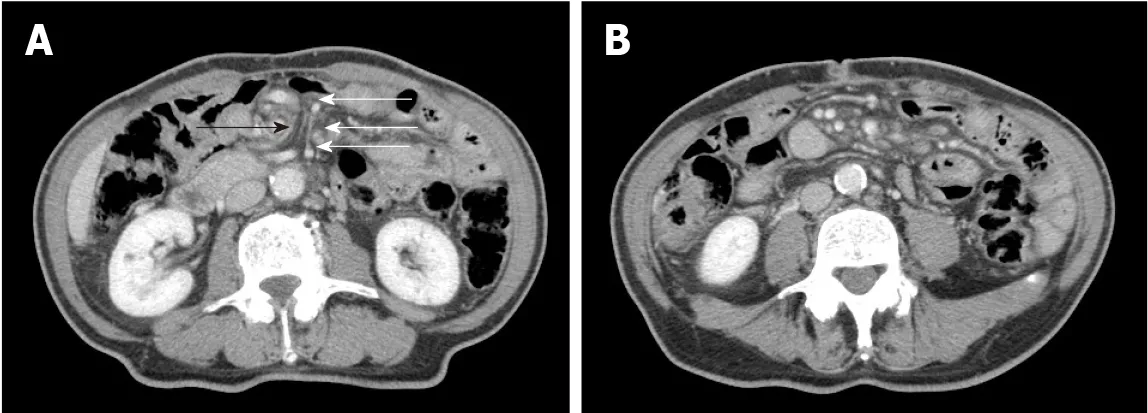
Upon the patient’s presentation with Petersen’s hernia, a contrast-enhanced CT scan showed an SMV twisted around the superior mesenteric artery in a spiral-like pattern, as well as venous congestion in the small intestine mesentery (Figure 1). On presentation for bilateral leg edema following his surgery for Petersen’s hernia, a contrastenhanced CT scan showed no thrombus in the SMV but a slight thrombus in the lower limb. At his presentation for the second occurrence of bilateral leg edema, amidotrizoic acid radiography revealed lesion stenosis and poor dilation over a segment approximately 6 cm in length (Figure 2).
FINAL DIAGNOSIS
Blood test results, including those for renal and hepatic function, at the time of admission were as follows: Total protein, 4.2 g/dL; albumin, 1.9 g/dL; blood urea nitrogen, 33.1 mg/dL; creatinine, 0.83 mg/dL; Na, 136 mEq/L; K, 4.4 mEq/L; Cl, 100 mEq/L; Ca, 7.1 mg/dL; aspartate aminotransferase, 45 U/L; alanine aminotransferase, 33 U/L; total bilirubin, 0.6 mg/dL; direct bilirubin, 0.2 mg/dL; lactate dehydrogenase, 336 U/L; creatine phosphokinase, 116 U/L; amylase, 51 U/L; cholinesterase, 70 U/L; total cholesterol, 131 mg/dL; high density lipoprotein cholesterol, 51 mg/dL; low density lipoprotein cholesterol, 63 mg/dL; and triglyceride, 88 mg/dL.
TREATMENT
This case report demonstrated two clinically important points. First, PLE complicated by extensive jejunal ulceration can develop in a delayed manner following the reduction of Petersen's hernia. Second, late-onset ulceration and stenosis of the jejunum occur in a segment of the small intestine vasculature following reduction of Petersen’s hernia, and preoperative DBE can help identify and successfully resect such lesions.
OUTCOME AND FOLLOW-UP
One month after discharge, the patient was edema-free, and his serum albumin and total protein levels had recovered to within normal limits. He has been free from leg edema and hypoalbuminemia over five years of follow-up.
DISCUSSION
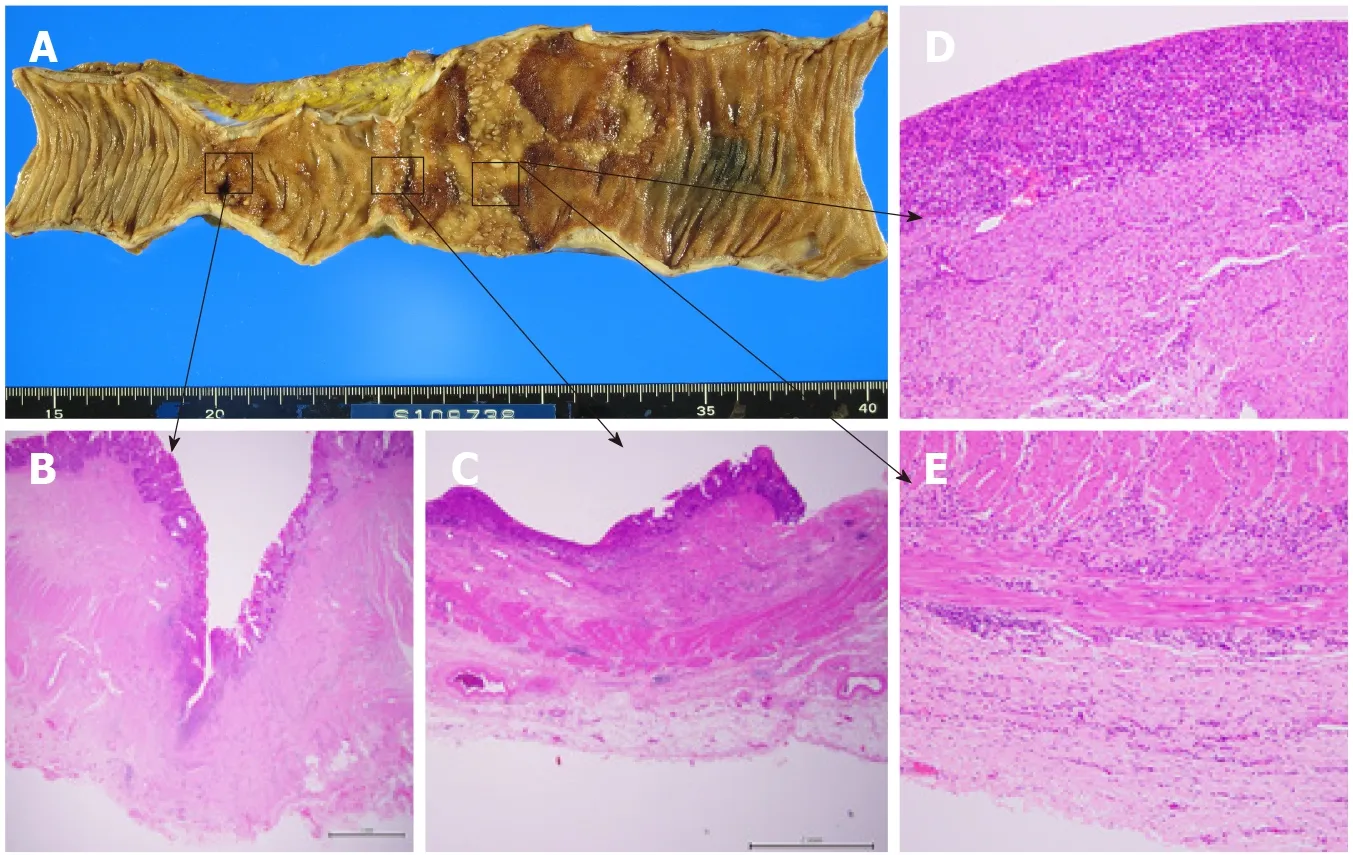
One week after the DBE, albumin solutions were administered again to treat bilateral leg edema, and laparotomy was performed. The jejunum proximal to the stenosis was extensively dilated, and marked ulcerative lesions were found. Therefore, only the jejunum between the stenosis and the marked jejunum was resected, and the remaining jejunum was anastomosed. The patient had a good postoperative course and was discharged on the 16day following the final surgery. Pathological findings examining the ulcerative lesions showed a deep-mining ulcer in the jejunum (to the muscularis propria) with collagen hyperplasia and a shallow ulcer with extensive epithelial loss and chronic inflammatory cell infiltration in all layers; pathological findings showed no evidence of lymphangiectasia, lymphoma, or vascular abnormalities (Figure 3).
He followed an ordinary diet before admission and switched to a low-fat, highprotein, elemental diet in the hospital.
When Sonali sang on the steps of the state capitol, her voice was unbelievably strong. It was as though she wanted to fill the whole universe with this impassioned prayer so it would reach her daddy. As she sang, I felt it also become a pure prayer to everyone gathered-a prayer that painted a vision. I was delighted when she asked me if she could sing again, this time for Alan s memorial service at Grace Cathedral in San Francisco.
According to a recent review, PLE can be divided into erosive and non-erosive intestinal lesions[8]. Common causes of erosive lesions of the small intestine include Crohn's disease, NSAID-associated enteritis, lymphoma, cytomegalovirus infection, and tuberculous enteritis, while rare causes include celiac disease, systemic vasculitis, ischemia, radiation-induced stenosis, and cryptogenic multifocal ulcerous stenosing enteritis[9]. Even a small jejunal ulcer can lead to PLE[10]. The major causes of nonerosive lesions are increased central venous pressure due to congestive heart failure, constrictive pericarditis, post-Fontan operation, and increased intralymphatic pressure due to lymphoma and primary intestinal lymphangiectasia[8]. To date, there have been few reports showing associations between hernias and PLE. Two previous reports showed congestion of mesenteric venous and lymphatic flow due to an internal hernia and bacterial overgrowth in the blind loop due to an incisional hernia; in these reports, PLE developed from non-erosive lesions and was successfully resolved by hernia repair[11,12]. This case report illustrates PLE caused by a completely different mechanism (an internal hernia after the surgical creation of Petersen’s space). To the best of our knowledge, this is the first report to show that a wide area of jejunal ulceration caused by ischemic attacks, including internal hernias, can lead to PLE.
The Prince turned sharply round and to his horror saw a huge Giant approaching with mighty strides, crying fiercely-- Who has made my lion whistle I should like to know? I have, replied Prince Vivien boldly, but I can answer for it that he will not do it again! At these words the Giant began to howl and lament94
Possible explanations for this mechanism include intestinal ischemia-reperfusioninduced inflammation and the characteristic wide Petersen’s space. It has long been shown in animal experiments that ischemia-reperfusion injury after a limited period of ischemia (the “window of reperfusion injury”) causes intense inflammation in all layers of the intestine[13,14]. It has likewise been shown that intensive inflammation due to prolonged intestinal ischemia reperfusion results in failure to restore damaged epithelium[15]. As Petersen's hernia has a wide hernial orifice and an accommodating space, intestinal necrosis is rare. However, a large amount of the small intestine is incarcerated. Therefore, extensive unrepaired epithelium caused by ischemiareperfusion-induced inflammation in cases of Petersen’s hernia can lead to PLE.
The efficacy of DBE for the diagnosis of PLE as well as obscure gastrointestinal bleeding and small bowel strictures has been demonstrated previously[16-23,25]. DBE has also been reported to be useful for not only treatments such as hemostasis, polypectomy, and balloon dilation but also preoperative India ink injection[24-29]. In this case, DBE revealed extensive intestinal damage with stenosis, poor dilation of > 5 cm, and a continuous ulcer of approximately 8 cm. Although resection of this sizable segmental lesion (which was due to ischemia) required minimal bowel resection, a dilated intestine (due to stenosis) makes surgical identification of extensive ulceration difficult. DBE effectively determined the extent of the lesion in the intestinal lumen before surgery, facilitating a combination of detailed observation, amidotrizoic acid radiography, tissue biopsy, and India ink injection. Thus, it not only revealed a rare form of extensive jejunal ulceration after an internal hernia in Petersen’s space but also proved to be an effective procedure from diagnosis to successful treatment with minimal bowel resection.
CONCLUSION
Following the reduction of Petersen's hernia, PLE complicated by extensive jejunal ulceration may develop in a delayed fashion. DBE is useful for identifying and resecting this lesion in segments of the small intestine vasculature. PLE after reduction of Petersen’s hernia may be misdiagnosed as hypoalbuminemia due to undernutrition after gastric surgery and various other diseases, and hence the presenting symptomology requires a search for small intestinal lesions that may underlie this presentation. Small bowel strictures after an ischemic attack have been reported to occur at intervals of several weeks following ischemia[30]. Therefore, even patients who have successfully recovered from Petersen’s hernia should be carefully followed up to detect delayed ulceration and stenosis at an early stage. While many patients with Petersen's hernia do not suffer from ischemia-reperfusion injury, it is unclear why this injury occurred in the incarcerated intestine in this case (resulting in a delayed jejunal ulcer). It is necessary to investigate the causes of ischemia-reperfusion injury after the reduction of Petersen’s hernias.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
