Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
INTRODUCTION
An incisional hernia is a common complication of abdominal surgery. It has an incidence of 9%-20% at 1 year of follow-up[1]. Fink[2] reported an incidence of incisional hernia of 22.4% in 755 cases of laparotomy at 3 years compared to 12.6% at 1 year after the procedure[2]. These findings indicate an increasing incidence of incisional hernia over time. A giant incisional hernia (> 10 cm in diameter) is normally treated with a prosthetic mesh using an open procedure[3,4]. This procedure is associated with a large amount of tissue dissection, extensive postoperative complications, long hospitalization, and lengthy recovery[5].
Incisional hernia repair with a laparoscopic approach has been advocated for approximately two decades and is characterized by minimal trauma, fast recovery, and short hospitalization[3]. A wide and clear visual field assists adhesion separation and examination of the abdominal wall defect[5]. However, laparoscopic closure is slightly difficult due to the suture technique, suture type, and increased abdominal wall tension caused by the pneumoperitoneum[6]. General laparoscopic repair requires a V-Loc suture, which increases treatment costs and is not widely used in China. Furthermore, the postoperative occurrence of seroma and hernia recurrence is high in both open and laparoscopic hernia repair[6], particularly in laparoscopic repair of giant abdominal hernias[7]. There is currently no consensus for the management of giant ventral hernias; nevertheless, several new methods have been proposed[8-10].
The hybrid application of open and laparoscopic procedures has been increasingly attempted for giant ventral hernia repair. In 2000, Lowe[11] proposed an endoscopy-assisted procedure for abdominal wall defect repair[11]. Sharma[12] subsequently argued that a limited-conversion technique offered a safe and viable alternative in laparoscopic incisional hernia repair in patients with a bowelincarcerated hernia sac or requiring extensive adhesiolysis[12]. Other studies revealed that a hybrid technique (laparoscopy with an additional open procedure using only a small incision) reduced the incidence of postoperative complications in patients with giant ventral hernias[13,14]. Griniatsos[15] reported a hybrid technique for recurrent incisional hernia repair[15]. Stoikes[16] proposed that the hybrid approach could be used in obese patients requiring open adhesiolysis during incisional hernia repair[16]. However, the outcomes and operative complications of hybrid approaches have not been compared with the single application of an open or laparoscopic approach. This study retrospectively reviewed patients with giant ventral hernias who underwent surgery from 2006 to 2013 and compared the outcomes and complications of the three commonly used techniques for giant ventral hernia repair.
MATERIALS AND METHODS
Patients
The medical records of adult patients (> 18 years of age) who underwent giant ventral hernia repair at the Department of Hernia and Abdominal Wall, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China, from January 2006 to June 2013, were retrospectively reviewed.
Adolescents < 18 years were excluded because they are still in the growth and development phase. Also, the use of synthetic materials can result in complications. Thus, the institution of this study prohibits the use of artificial materials in persons < 18 years.
A preoperative computed tomography (CT) of the abdomen was performed in all patients to diagnose the hernia and evaluate the hernia characteristics. A giant ventral hernia was defined as a hernia defect with a diameter ≥ 10 cm. The hernias were classified based on the 29Congress of the European Hernia Society[3]. Patients with a giant ventral hernia, who received a planned hernia repair procedure, open, laparoscopic, or hybrid, were included in the analysis. Exclusion criteria were as follows: (1) The presence of skin ulceration or infection; (2) The use of anticoagulants or high-dose hormones within 4 wk before the procedure (anticoagulants can result in bleeding and may affect hematoma formation; hormones can affect the immune system and alter postoperative changes of inflammatory mediators); (3) Participation in other clinical studies within 3 mo before the procedure; (4) A history of atopic allergy; (5) Major mental illness (, schizophrenia, severe anxiety, or depression); (6) Conditions that can significantly increase intra-abdominal pressure (, ascites associated with liver cirrhosis, cough from chronic obstructive pulmonary disease, and intractable constipation); (7) Infection at the operative site or bacteremia; and (8) Patients requiring emergency surgery (, bowel strangulation).
The laparoscopic group had a relatively high postoperative complication rate. Laparoscopic extraperitoneal hernia repair began in 2009, and a learning curve was evident. The definition of intestinal injury during laparoscopic manipulation was partial or full-thickness intestinal wall injury when laparoscopic hernia repair began. This complication was relatively common at the beginning of the learning curve. With advances in equipment and our experience, the current injury rate is very low. In addition, the cost of open cases was lower than for laparoscopic cases due to the cost of equipment required for laparoscopic repair. For example, using a hernia fixer (Medtronic, Shanghai, China; a product similar to ProTack) in laparoscopic repair raises the costs compared to an open procedure.
Operations
All procedures were performed under general anesthesia by surgeons with a minimum of 10 years of experience repairing ventral hernias by open and laparoscopic approaches.
Open and laparoscopic repairs were performed using the intraperitoneal onlay mesh technique. Composix E/X mesh (15.5 cm × 20.5 cm to 20 cm × 30 cm; Davol Inc., Warwick, RI, United States) was used for hernia repair. Every patch was extended 5 cm beyond the exterior margin of the inner defect and was fixed to the abdominal wall. In the open procedures, the mesh was fixed with an abdominal wall suturing device (Covidien, Dublin, Ireland). A full-thickness abdominal wall penetrating hanging suturing line (single polypropylene suture) was fixed at the 12 or 10 o’clock position. The mesh patch was fixed in the laparoscopic group at one central and two side points using an abdominal wall hanging penetrating suture. The surrounding area and edge were fixed with laparoscopic tacks. The basic principle was that the distance between tacks was not < 3 cm.
Patients who received a preplanned hybrid procedure had a low complication rate, indicating that careful preoperative planning and preparation are important for improving the procedure’s safety. Furthermore, a hybrid procedure was associated with a low rate of postoperative intestinal fistula formation. These results may be due to the avoidance of forced intestinal adhesiolysis, the recognition of hidden injury in the laparoscopic phase, and reliable intestinal injury repair in the open phase. Importantly, postoperative complications were significantly lower in the hybrid group. Hernia recurrence and reoperation rates were the lowest, whereas laparoscopic cases had the highest reoperation rate. This finding may be due to the preservation of the hernia sac in the laparoscopic procedure. Moreover, a laparoscopic procedure alone does not allow proper closure of the hernia defect or adequate remodeling of abdominal wall integrity, resulting in higher recurrence and seroma formation.
It was another long, winter afternoon with everyone stuck in the house and the four McDonald children were at it again -- bickering1, teasing, fighting over their toys. At times like these, Mother was almost ready to believe that her children didn’t love each other, though she knew that wasn’t really true. All brothers and sisters fight, of course, but lately her little lively bunch had been particularly horrible to each other, especially Eric and Kelly, who were just a year apart. They seemed determined2 to spend the whole winter making each other miserable3.
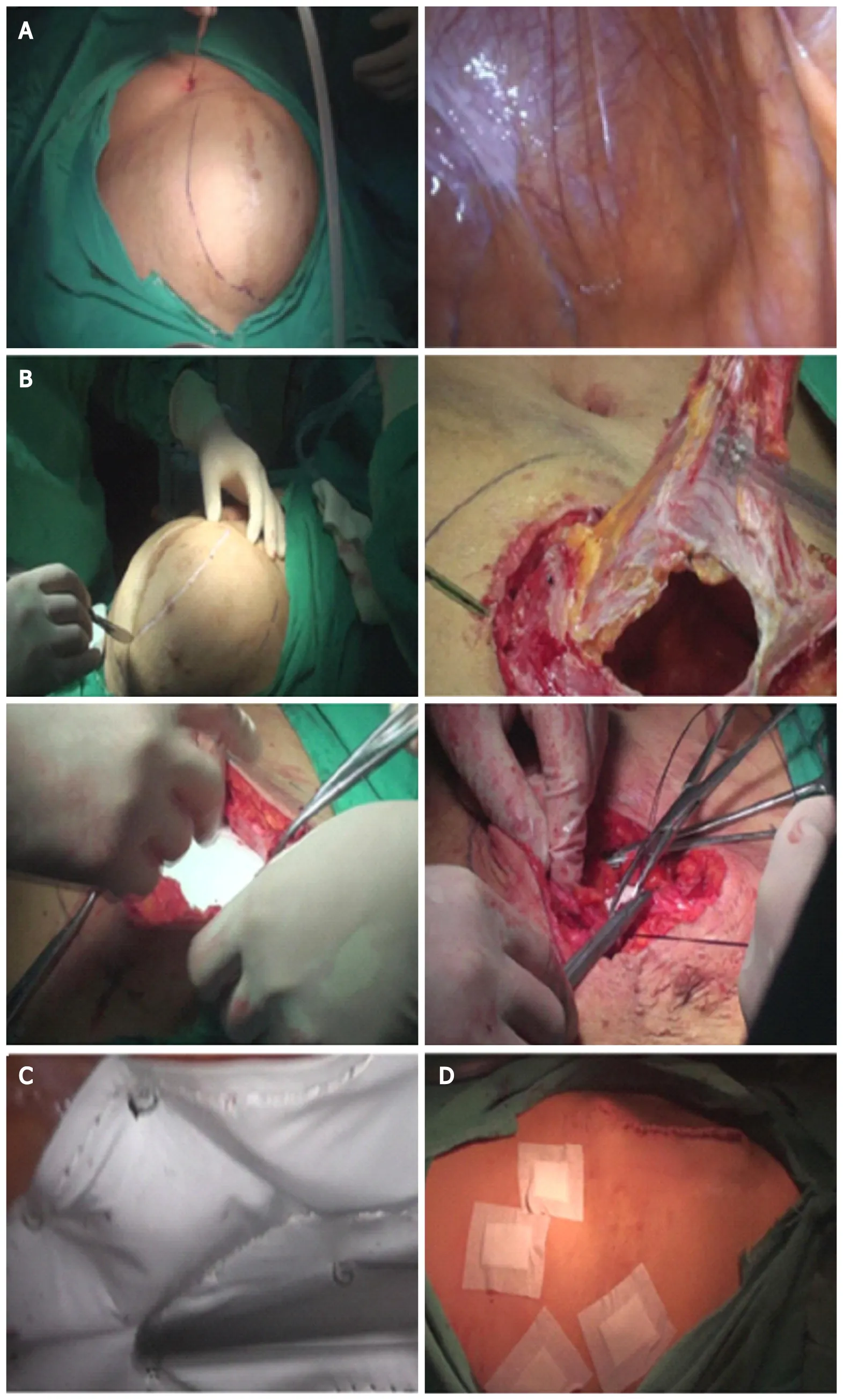
The anti-adhesive surface of the mesh was placed facing the abdominal cavity. The center of the mesh patch and the hernia ring was sutured using PDS-II sutures, and laparoscopic tacks fixed the surrounding mesh. The basic principle was that the distance between the tacks was not < 3 cm. A low-pressure (8-10 mmHg) pneumoperitoneum was reestablished, and the mesh was laparoscopically fixed with spiral tacks (Medtronic Inc., Minneapolis, MN, United States; Figure 1C) using double-loop multipoint fixation at 1.5-2.0 cm intervals. The pneumoperitoneum was evacuated, and the trocars removed. Superficial tissues were closed with a 2-0 absorbable interrupted suture. The skin was closed with staples or a continuous 4-0 absorbable suture (Figure 1D).
The hernia recurrence rate was calculated. Intraoperative and postoperative complications, surgical time, blood loss, length of hospital stay, and mortality were also recorded. Intraoperative and postoperative complications included intraoperative intestinal injury, postoperative intestinal fistula formation, chronic pain, postoperative infection, hematoma or seroma, and perioperative mortality. Patients were followed at 1, 3, and 6 mo after the procedure and then yearly by outpatient visit or telephone interview with the surgeon. Hernia recurrence was diagnosedphysical examination and abdominal CT scan. A CT scan was requested to determine if a hernia recurrence existed if a patient described a bulge or pain in the area of the operation. Diagnosis of all recurrent hernias was based on CT and/or abdominal examination.
Data were expressed as mean ± SD for continuous variables and frequencies and percentages for categorical variables. Normally distributed data were compared using a one-way analysis of variance followed by the Bonferroni test. Moreover, categorical variables were analyzed with thetest. A statistically significant difference was defined as a< 0.05. SPSS version 20 (SPSS Statistics, IBM Corp., Armonk, NY, United States) was used for all statistical analyses.
This can still be seen in many rich farms on the west coast ofJutland: plenty to eat and drink, clean, prettily decorated rooms,active minds, cheerful tempers, and hospitality can be found there, asin an Arab s tent
Outcome measures
After which you must steer towards the land, and she will follow you, for she won t be able to resist the beautiful wares29 you have on board your ship
Chronic pain was defined as moderate or severe pain (C4) in the mesh fixation area 3 mo after the procedure based on a visual analog scale: 0 points, no pain; 1-3 points, mild pain; 4-7 points, moderate pain; and 8-10 points, severe pain. Ultrasound examination was performed in patients with suspected hematoma or seroma (suspected fluid collection on physical examination or a complaint of pain). If fineneedle aspiration produced a minimum of 10 mL of fluid, the diagnosis was made. Wound infections were defined as the presence of swelling, increased pain and temperature at the incision site, and purulent drainage.
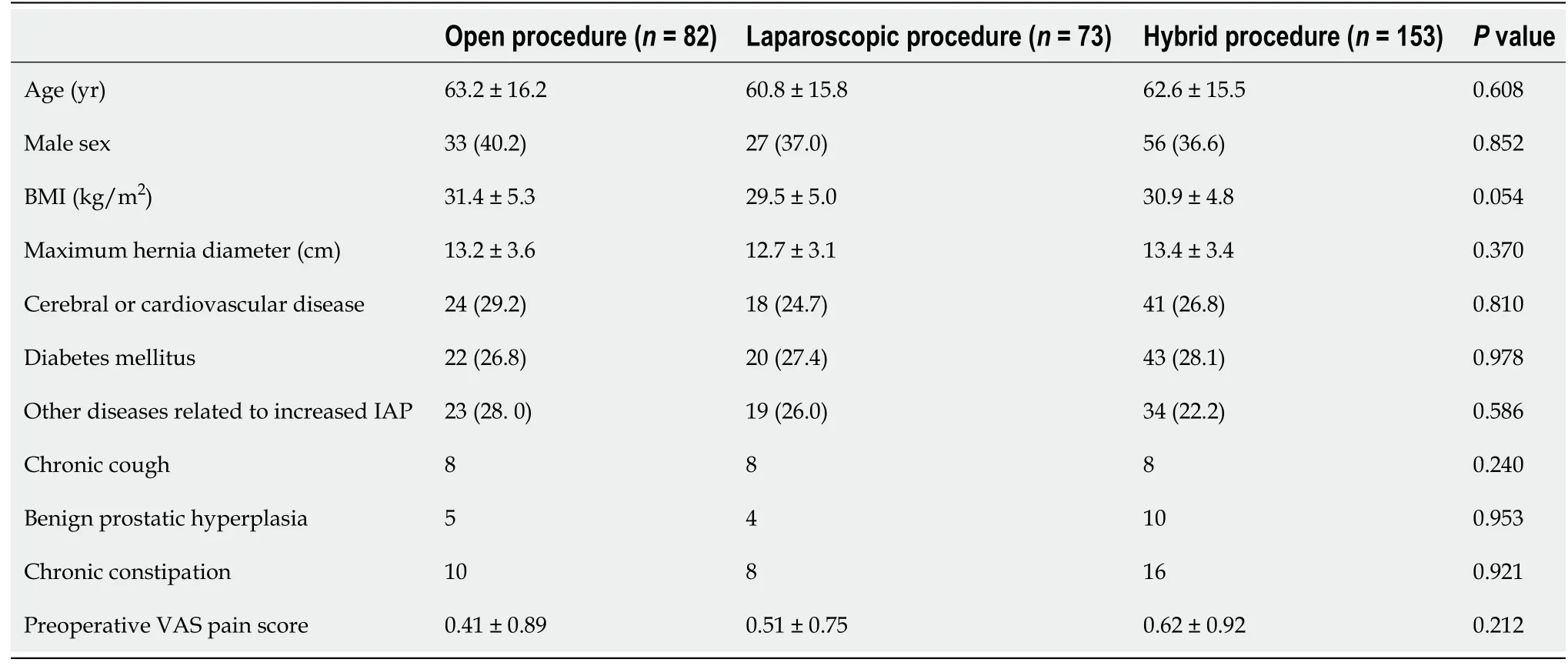
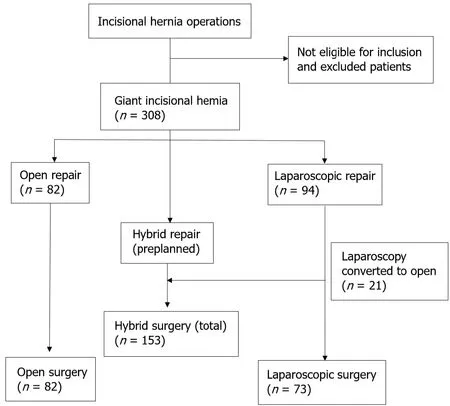
A total of 754 patients received surgical treatment for incisional hernias, and 308 cases were included. A flow diagram of patient inclusion is shown in Figure 2. Table 1 summarizes patient characteristics. The minimum and maximum hernia diameters were 10 and 30 cm, respectively. An open procedure, laparoscopic approach, and hybrid approach were performed in 82, 94, and 132 patients, respectively. Moreover, 58.7% of the patients were women, and the mean diameter of hernias was 13.11 ± 3.4 cm (range, 10-30 cm). Patients had a mean body mass index of 29.7 ± 44.6 kg/m(range, 16.7-38.3 kg/m), and the three groups were comparable in demographic and baseline characteristics (all,> 0.05).
Systemic or intra-abdominal infections were defined as a body temperature > 38 °C for 3 consecutive days, excluding respiratory and urinary tract infections and a white blood cell count > 10000 with a neutrophil ratio > 80%.
Statistical analysis
Intraoperative serosal injuries in all cases were repaired with 3-0 absorbable sutures. Full-thickness injuries were repaired by resection, and drains were placed in the abdominal cavity if a large dissection was performed in all three procedures. Drains were placed in the pelvic cavitythe paracolic sulcus to be at the lowest position. Similarly, suction drains were subcutaneously placed. All drains were typically removed 2-3 d after the procedure. Postoperative care was the same for all three groups. All cases were advised to take necessary measures to protect the repair, including an abdominal bandage for 6 mo after the procedure and control of body weight to minimize abdominal pressure. After consulting the allergy history, patients were treated with second-generation cephalosporins. Quinolones were used if patients were allergic to cephalosporins.
RESULTS
Patients
In a preface to a later collection of his tales, Andersen explained that The Emperor s New Clothes, published in 1837, is of Spanish origin. He went on to say, We owe the amusing idea to Prince Don Manuel, who was born in the late thirteenth century. Andersen also pointed out that Cervantes used the idea in an entr acte. But if the idea of The Emperor s New Clothes was centuries old, it did not become international shorthand for all sorts of conformist behavior until Andersen wrote it his way (Frank and Frank 105).
The surgical details of the three groups are summarized in Table 2. The mean operation times were 76.7 ± 23.7, 63.6 ± 12.1, and 113.6 ± 21.8 min for the hybrid groups, respectively (< 0.001). Overall, the incidence of postoperative complications was significantly lower in the hybrid group (7.23%) than in the open (17.1%;= 0.019) or laparoscopic (26.0%;< 0.05) groups. The intraoperative intestinal injury rates were 6.1%, 4.1%, and 1.5% in the open, laparoscopic, and hybrid groups, respectively (hybridopen and laparoscopic procedures;< 0.05). In addition, the postoperative intestinal fistula formation rates in the open, laparoscopic, and hybrid groups were 2.4%, 6.8%, and 3.3%, respectively, and these differences were not significant (> 0.05). The postoperative intestinal fistula ratiointraoperative intestinal injury was markedly lower in the hybrid group than in the laparoscopic group (hybrid group, 0.2; laparoscopic group, 0.7;= 0.013) but was not different from the open group (0.4;> 0.05). The reoperation rate was lowest in the hybrid group (3.9%; open group, 12.2%; laparoscopic group, 24.78%;< 0.001) because it had the lowest postoperative hernia recurrence. The patients with seroma were asymptomatic. The laparoscopic procedure group had the highest seroma formation rate (32.8%; open group, 6.1%; and hybrid group, 2.6%;< 0.001) but the lowest incidence of operative site infections (1.4%; open group, 0.3%; and hybrid group, 5.2%;> 0.05). Patients who received an open procedure had a longer hospital stay (13.0 ± 8.7 d) than those who received laparoscopic (6.9 ± 14.2 d) and hybrid (8.5 ± 7.9 d) procedures (= 0.002).
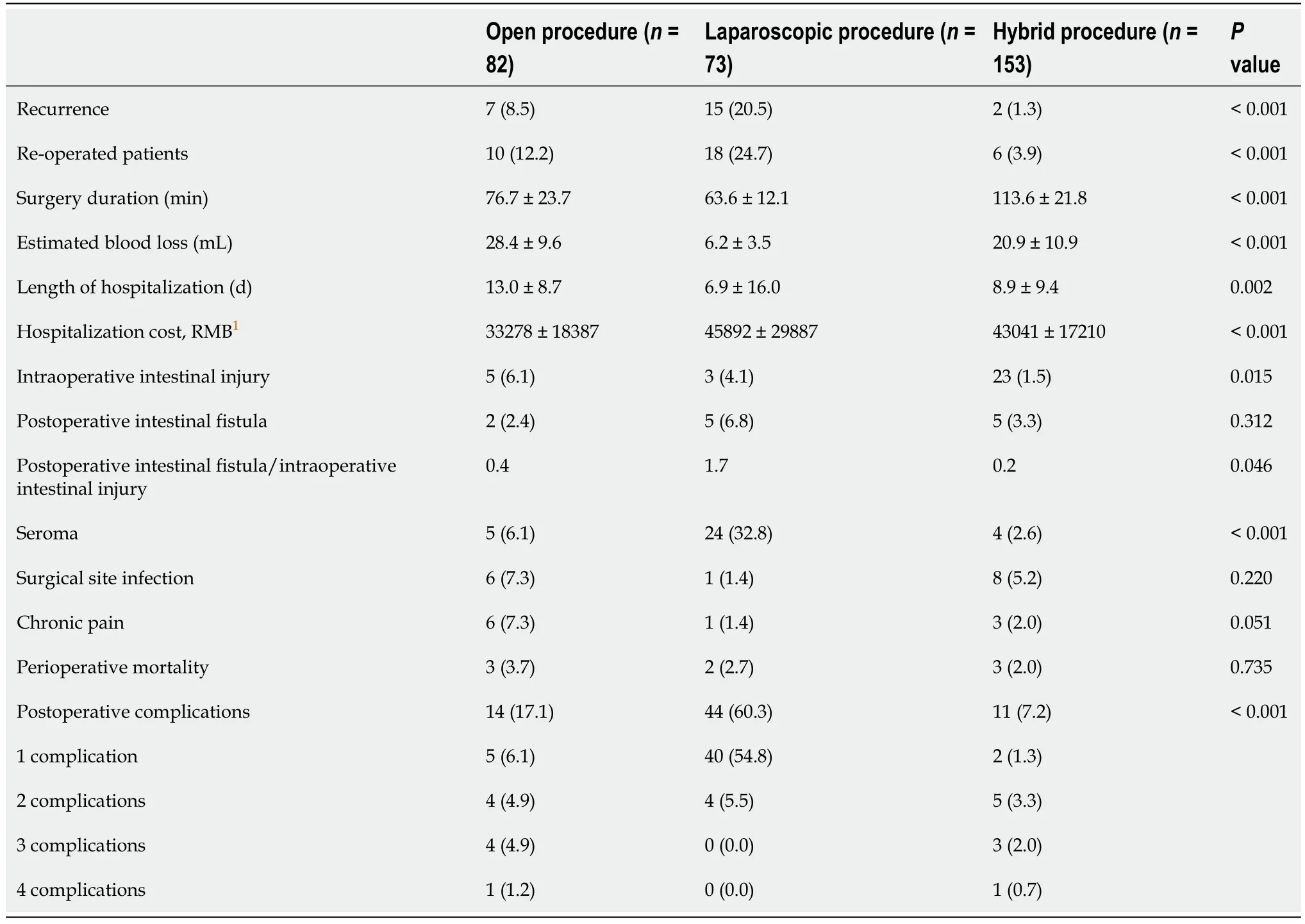
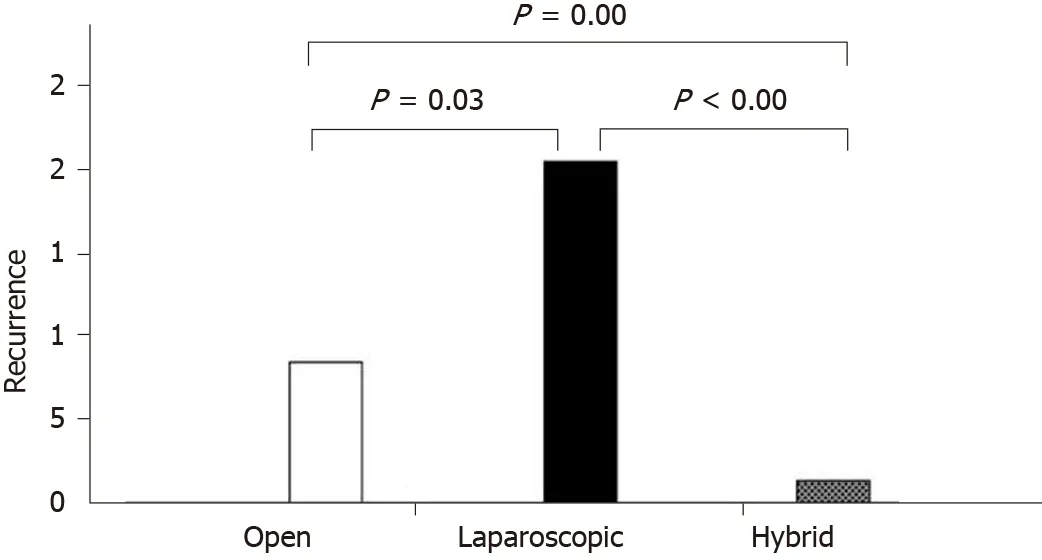
All patients were followed up 1 wk after the operation. The outpatient clinic followup rates at 1 mo, 3 mo, and 1 year were 40.6%, 37.3%, and 14.6%, respectively. Other patients were followedtelephone interview. The mean follow-up times for the open, laparoscopic, and hybrid groups were 45, 40, and 39 mo, respectively. Thus, the mean follow-up time for the three groups was 41 mo (range, 12-88). The follow-up time in the hybrid group was shorter than in the other two groups. The hernia recurrence rate in patients who received a hybrid procedure was 1.3% at the final follow-up. This finding was significantly lower than that in the laparoscopic (12.3%) or open groups (8.5%;< 0.05; Figure 3).
The Princess s father, who had never ceased to repent13 his harshness towards his daughter, had sought her through the land, but as no one could tell him anything of her, he supposed her dead
Patients who received an open procedure had the highest rate of chronic pain (laparoscopic group, 1.4%; open group, 7.3%; and hybrid group, 2.0%;> 0.05) but the lowest hospitalization costs (< 0.001). Perioperative mortality was comparable among the three groups (open, 3.7%; laparoscopic, 2.7%; and hybrid, 2.0%;> 0.05).
So he procured16 some bears skins, and covered himself and his horse with them, so that not a particle of gold could be seen, and then rode bravely on into the heart of the forest
DISCUSSION
Although component separation with retromuscular mesh repair is the primary procedure used, multiple alternative strategies have been gradually investigated to overcome the high rate of hernia recurrence and the unacceptably high incidence of wound complications[19]. A hybrid procedure combining open repair with a laparoscopic technique has been increasingly reported[15,16]. However, there is no literature regarding its efficacy, safety, and cost-effectiveness compared to open and laparoscopic procedures. This study evaluated the outcomes and surgical complications of the hybrid approach of open and laparoscopic approaches. Hernia recurrence and complication rates were significantly lower in patients who received a hybrid procedure compared with the single application of open or laparoscopic procedures.
In a study conducted from 2006 to 2008, Ozturk[20] randomized 28 patients with giant incisional hernias to receive standard laparoscopic repair or a hybrid approach,, laparoscopy combined with an open approach[20]. The mean length of hospital stay and the operative site infection rate were comparable in both groups. Six patients developed seromas in the laparoscopy group and one in the hybrid group. However, there were no recurrences in the hybrid group and one in the laparoscopic group. However, this study was partially compromised by the small number of cases and a short follow-up. Large hernia size, infection, and operative technique are important determinants of surgical outcomes after giant hernia repair[6,21]. This study showed that the hernia recurrence rate of the hybrid procedure was 1.3%. This finding significantly lower than a laparoscopic or open procedure and the reported recurrence rates[19]. The low recurrence rate with the hybrid technique may be due to the complete removal of the hernia sac, proper closure of the hernia defect, and satisfactory reshaping of the abdominal wall in the open phase. Careful laparoscopic exploration, adhesiolysis, mesh flattening and fixation, ensuring the integrity of abdominal wall remodeling, and avoiding hidden hernia omission also likely contribute to the low incidence of hernia recurrence[16,19].
A recent meta-analysis showed 2.7% and 8.2% recurrence in mesh and repairs, respectively[22]. The hernia recurrence rates of open and laparoscopic procedures were higher in this study, which may be due to a longer follow-up. Fink[2]. reported that the hernia recurrence rate with open repair increased over time (22.4% at 3 years12.6% at 1 year after the procedure)[2]. Another study showed that the hernia recurrence rate increases up to 10 years after the primary incisional hernia repair[23]. Reportedly, 85% and 77% of recurrences after laparoscopic and open repair, respectively, occur within 2 years of the procedure in ventral hernias cases[24]. Therefore, a long-term follow-up is needed to determine if the hybrid approach is superior to other approaches concerning recurrence.
The treatment of abdominal hernias using the hybrid method explored and separated the intra-abdominal adhesions under laparoscopy. Open surgery was then used to remove the extra hernia sac to extensively separate tissues along the interstitial muscle line, place the patch in the abdominal cavity, suture and close the hernia ring, and close the incision. The patch was then fixed under laparoscopy. Pneumoperitoneum (12-14 mmHg pressure) was established in hybrid procedures. The laparoscope was introduced to explore the abdominal cavity, separate adhesions, and reduce the hernia content. The hernia defect was dissected 5 cm beyond the exterior margin of the inner defect (Figure 1A). Conversion to laparotomy was performed if the hernia contents could not be completely reduced. The pneumoperitoneum was evacuated with the trocars retained. A targeted fusiform incision (usually 4-8 cm long and 1-3 cm wide) was made at the weakest point of the hernia sac along the original incision line (Figure 1B). The hernia sac was completely resected by stripping, and the intestines were explored. The posterior component separation technique with transversus abdominis release was used to close the abdominal wall defect with low or no tension[17,18]. The hernia defect was closed by continuous suture using PDS-II at 1 cm intervals after the Composix E/X mesh was implanted in the abdominal cavity.
Patients undergoing laparoscopic or open giant ventral hernia repair have a high likelihood of chronic pain and activity limitations[25,26]. In this study, the length of hospital stay, intraoperative blood loss, and postoperative chronic pain were lowest in the hybrid group, possibly due to a smaller incision and avoidance of excessive fullthickness abdominal wall suspension fixation (transabdominal sutures), which are typically used in an open repair.
The local Ethics Review Boards of Chao-Yang Hospital approved the study protocol. All procedures were performed following established European and American guidelines for hernia repair, and all patients provided written informed consent for all procedures performed.
This study had some limitations. First, the retrospective nature of this study may cause biases. Second, the hernia sac volume was not examined. Moreover, the diagnosis of hernia recurrence may slightly affect lead-time bias. Last, the definition of hematoma/seroma formation may underestimate their occurrence.
CONCLUSION
In conclusion, a hybrid approach of laparoscopic and open procedures is effective for giant ventral hernia repair. It is associated with low complication and hernia recurrence rates. Hybrid repair combines laparoscopic and open repair advantages and minimizes the disadvantages of the two approaches.
ARTICLE HIGHLIGHTS
Research background
Incisional hernia is a common complication of abdominal surgery. The traditional method, including open or laparoscopic surgery, still has many limitations.
Most of the time we gossiped() about people, and I soon realized that nobody was good enough for Jennifer. Jennifer had a list of bad things about everybody, even Amy. And I m sure she had a list of bad things about me, too. After months of living through school this way, I had really changed. I was moody4(), depressed5, lonely, and I didn t smile much. I spent lots of days trying not to cry, I felt so left out.
Research motivation
This study motivated us to investigate the potential advantages of a hybrid application of open and laparoscopic approaches in giant ventral hernia repair.
Research objectives
This study tried to determine if a hybrid application of open and laparoscopic approaches is more effective and safer in the repair of giant ventral hernias than a single open or laparoscopic procedure.
Research methods
Patients were retrospectively reviewed and divided into open (n = 82), laparoscopic (n= 73), and hybrid group (n = 153), respectively. The hernia recurrence rate, intraoperative and postoperative complications, operative time, blood loss, length of hospital stay, and mortality in the three groups were also recorded and analyzed.
If I am not much mistaken, said he, there is some mysterious connection between our misfortunes, but how to find the key to the riddle91 is the question
Research results
Patients in the three groups were comparable in demographic and baseline characteristics(all, P > 0.05). The mean operation times of the hybrid group were significantly longer than the open and laparoscopic groups (76.7 ± 23.7 vs 63.6 ± 12.1 and 113.6 ±21.8, P < 0.001). However, the incidence of postoperative complications was significantly lower in the hybrid group (7.23%) than in the open (17.1%; P = 0.019) or laparoscopic (26.0%; P < 0.05) groups. Besides, the hybrid group had a significantly lower intraoperative intestinal injury rate, reoperation rate, and seroma formation than the open and laparoscopic groups (1.5% vs 6.1% and 4.1%, P < 0.05; 3.9% vs 12.2% and 24.78%, P < 0.001; 2.6% vs 6.1% and 32.8%, P < 0.001).
The forecast helped Maggie to make up her mind. Despite misgivings6, the attraction of the moor in the late summer sun was too strong. It had to be faced one day on her own; it was too beautiful to stay away forever. The time had come to lay this ghost to rest and picking a few berries would keep her mind occupied. Decision made, Maggie turned off the TV and went to help with homework.
Research conclusions
The hybrid approach of laparoscopic and open procedures is associated with lower complication and hernia recurrence rates. It combines the advantages of laparoscopic and open repair and minimizes the disadvantages of the two approaches.
Research perspectives
The hybrid approach of the laparoscopic and open procedures, which is worthy of clinical application, is an effective method for giant ventral hernia repair.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
- Vancomycin lavage for the incidence of acute surgical site infection following primary total hip arthroplasty and total knee arthroplasty
