Vancomycin lavage for the incidence of acute surgical site infection following primary total hip arthroplasty and total knee arthroplasty
INTRODUCTION
Total joint arthroplasty (TJA) is highly effective for reducing pain and improving quality of life in patients requiring joint replacement[1]. However, implant infections remain a relatively rare but devastating complication associated with this procedure[2-5]. Although improved sterile techniques, wound protection, minimization of contamination, and prophylactic antibiotics (systemic or local antibiotics) have markedly reduced the incidence of surgical site infection following TJA, implants may become infected by direct contact with an infected wound during the procedure or by spread of a superficial wound infection to the fascia lata or bloodborne contamination during or after the procedure[6]. Intraoperative contamination of the surgical wound by bacterial seeding from the air of the operating room, the skin of the patient, or fallen debris or hair from surgical staff is an important cause of surgical site infection following TJA[7-10]. In addition, TJA can lead to hematoma formation, which creates conditions that encourage bacterial growth[10,11], and bacteria can form biofilms that protect them from antimicrobials and the patients’ immune response, thus making eradication difficult.
The incidence of postoperative wound infection is estimated to be 0.5%-2% following primary TJA and 3%-7% following revision TJA[6,7,12]. Local application of an antibiotic solution may reduce the contamination of wounds with commensal bacteria from the patient’s skin or with airborne bacteria during TJA. Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery[13-20]. Therefore, the purpose of this retrospective study was to investigate the effectiveness of prophylactic intraoperative application of vancomycin (1000 mg/L; 2 L) solution vs. plain irrigation in reducing the incidence of acute surgical site infection following primary total hip arthroplasty (THA) and total knee arthroplasty (TKA).
MATERIALS AND METHODS
After institutional review board approval, we reviewed data for 2725 consecutive patients undergoing primary THA or primary TKA between January 2012 and December 2019 with a minimum of 3 mo of follow-up. One surgeon performed all the procedures in the given time period. Patients were identified, and data related to patient demographics, baseline characteristics, and comorbidities and operative data were collected from medical records. These cases were retrospectively reviewed for the occurrence of surgical site infections within 3 mo after surgery.
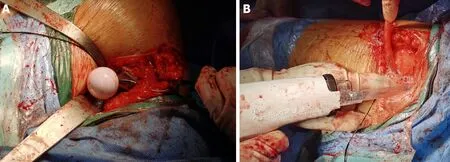
Each patient received standard antibiotic prophylaxis (2 g cefazolin) approximately 30 min before surgery. Antibiotic-loaded cement was used in patients with a higher risk for infection due to a body mass index of > 35, diabetes mellitus, or rheumatoid arthritis. The first 1018 patients (453 undergoing THA and 565 undergoing TKA) received irrigation with 2 L of normal saline after hardware implantation during THA between January 2012 and December 2015 (control group); the subsequent 1175 patients (512 undergoing THA and 663 undergoing TKA) received irrigation with 2 L of vancomycin (1000 mg/L) before wound closure between January 2016 and December 2019 (vancomycin group). Postoperatively, all patients were provided routine antibiotics (1000 mg cefazolin/8 h or 1000 mg vancomycin/12 h for patients who were allergic to penicillin) for 24 h (Figure 1).
Acute infections that occurred within the period of interest were classified as superficial or deep. Superficial infections were defined as infections in which the sutures and anastomosis of the fascial layer were intact without pus or fistula draining from the subfascial layer during debridement. Deep infections were defined as infections involving the drainage of pus from the subfascial layer, with the subfascial layer being open. Superficial wound infections were managed with superficial debridement and antibiotics. Deep infections were treated with debridement, an antibiotic-loaded bone cement spacer, and two-stage revision. Postoperative wound complications such as minor fat liquefaction or erythema were treated with routine wound care. The 3-mo period investigated in this study was defined as the acute infection phase based on the authors’ clinical experience, which indicates that 95% of infections occur within this time frame.
Statistical analysis
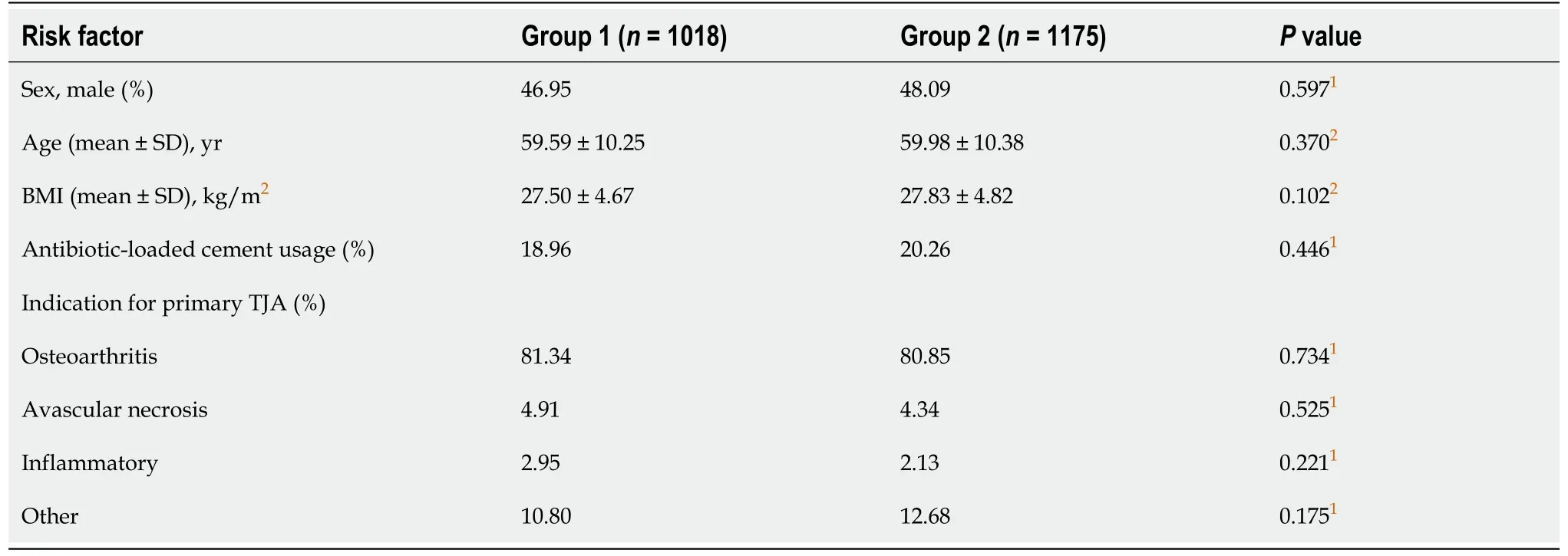
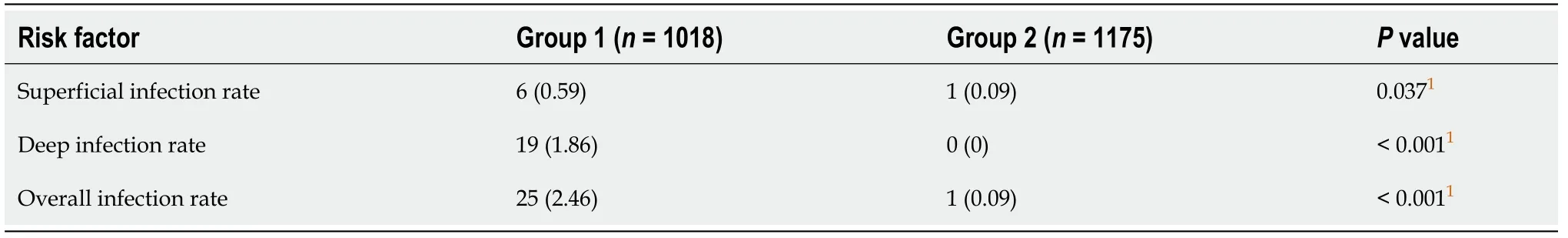
There were no significant differences in sex, age, duration of surgical procedure, or use of antibiotic-loaded cement between the two groups (Table 1). There was a significantly higher incidence of acute infection at the surgical site in patients who received intrawound irrigation with normal saline prior to wound closure than in patients who received intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) prior to wound closure (Table 2). The overall incidence of infection in group 1 was 2.46%, and that in group 2 was 0.09% (< 0.001).
RESULTS
All analyses were conducted using SPSS version 21.0 software. Between-group differences for continuous variables were evaluated using Student’s-test. Betweengroup differences in the rate of surgical site infection were assessed using thetest with Yates; correction or thetest alone when the sample size was < 20 or any value was < 5. Statistical significance was defined as< 0.05.
Only one patient in the vancomycin group had an acute superficial infection at the surgical site (occurring within 2 wk), and the infecting organism was.
Prophylactic irrigation with vancomycin solution (1000 mg/L; 2 L) significantly reduces the incidence of infection after primary TJA. This strategy is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
At least a hundred people witnessed the most difficult moment of my life, but only one person mattered. Of course I will sing for you, Mom. Feel free to ask me any time.
Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery.
One day another ship was wrecked on the coast, and among otherthings a chest filled with valuable flower bulbs was washed ashore.Some were put into saucepans and cooked, for they were thought to be fit to eat, and others lay and shrivelled in the sand- they did notaccomplish their purpose, or unfold their magnificent colours. WouldJurgen fare better? The flower bulbs had soon played their part, buthe had years of apprenticeship before him. Neither he nor hisfriends noticed in what a monotonous, uniform way one day followedanother, for there was always plenty to do and see. The ocean itselfwas a great lesson-book, and it unfolded a new leaf each day of calmor storm- the crested wave or the smooth surface.
DISCUSSION
This retrospective review of patients undergoing primary TJA, which was undertaken by a single-surgeon team over a ten-year period, suggests that compared with irrigation with normal saline alone, intraoperative irrigation with vancomycin solution (1000 mg/L; 2 L) can significantly reduce the incidence of acute infection of the surgical site following primary THA and primary TKA (2.46%0.09%,< 0.01).
High concentrations of antibiotics in the surgical wound are necessary to prevent infection throughout the operation from incision to wound closure[18]. Unfortunately, intravenous application yields a relatively low concentration of antibiotics at the surgical site over time (generally above the minimal inhibitory concentration for < one hour)[18]. Minimal toxicity is not associated with the generation of microbial resistance[21,22]. Surgical wounds contain areas that are not reachable by intravenously delivered antibiotics (such as hematomas and ischemic areas).
Intraoperative contamination of the wound is an important risk factor for surgical site infection after joint replacement[7-10]. Wound contamination may result from commensal organisms (present on the patient’s skin), airborne bacteria, and occasionally, debris or hair falling from the surgical staff[7-10]. Prophylactic antibiotics have been used to reduce surgical site infections. However, the overuse and misuse of antibiotics in recent years has led to the development of antibiotic-resistant pathogens. Irrigation of surgical wounds with antiseptics has been used to prevent infections during the treatment of open fractures and other surgically related conditions. Vancomycin is an effective prophylactic systemic antibiotic that is used during total knee or hip arthroplasty and drastically reduces the risk of infection[14-17]. Intrawound application of vancomycin powder has been proven to reduce infection rates following spine surgery and to decrease the incidence of surgical site infections; however, the data regarding the use of vancomycin powder during primary TJA are controversial[19,21-25]. In 2010, a prospective, controlled study evaluating the safety and effectiveness of an absorbable calcium hydroxyapatite (Hac) layer mixed with vancomycin and applied to the articular surface of prosthetic implants in preventing deep infections after non-cemented TKA was conducted[19]. Vancomycin paste (a mixture of 2 g absorbable Hac and 1-2 g vancomycin) was applied to the implants in the study group. The rate of early infection was 0% in the study group and 4.1% in the control group. This study shows that local anti-infection treatment is an effective supplement to systemic antibiotic therapy for the prevention of deep infections in noncemented TKA. The pharmacokinetics of vancomycin powder in thirty-four TJA patients who received 2 g of vancomycin powder intraoperatively were investigated[23]. Serum and wound concentrations were measured at multiple intervals in the 24-h period after closure. The wound concentrations were 922 μg/mL 3 h after closure and 207 μg/mL at 24 h. Vancomycin powder application during TJA produced high therapeutic intrawound concentrations while yielding low systemic levels. However, in 2017, the safety of using vancomycin powder to reduce infection rates was investigated by reviewing the incidence of acute postoperative complications[24]. It was found that compared with control treatment, vancomycin powder was associated with an increased rate of sterile wound complications (4.4%0%)[24]. The rate of prosthetic joint infection (PJI) was decreased with the use of vancomycin powder (5.5%0.7%). Researchers therefore do not recommend for or against the use of vancomycin powder at the time of wound closure to prevent PJI. Furthermore, a controlled trial was conducted to investigate the efficacy and side effects of local highdose vancomycin powder application to the joint to prevent PJI following TKA[25]. They found that intrawound administration of vancomycin powder did not decrease the occurrence of PJI following primary TKA and caused aseptic wound complications. Thus, the use of intrawound and intravenous agents for the prevention of PJI after primary TKA is not recommended.
In the present study, no surgical site infections occurred during the 3 mo after surgery in primary TJA patients who received intrawound irrigation with vancomycin solution before wound closure. Intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) before wound closure may create a potent bactericidal environment by producing a high local tissue concentration of antibiotics. A similar technique during TJA was recently described[18]. A study involving > 2000 patients was performed to evaluate the effectiveness of local antibiotic irrigation during surgery for the prevention of acute postoperative infections after TJA. The intraoperative protocol included irrigation with normal saline containing 1000 mg/L vancomycin and 250000 units/L polymyxin at a rate of 2 L per hour. The researchers found that the use of antibiotic irrigation during arthroplasty surgery was highly effective in preventing infection and reported that irrigation with local antibiotics can prevent acute infection, even with prolonged operating times during revision procedures. However, there was a lack of a control group in the study.
This study showed that the prophylactic use of vancomycin solution can significantly decrease the incidence of acute surgical site infection following primary THA and TKA. However, the present investigation had several limitations. First, it was a retrospective study. Second, all patients had a minimum follow-up of 3 mo (acute infection); a longer follow-up period will help detect delayed infections. Third, other factors, such as hip joint materials (ceramic-ceramic and metal-polyethylene), affected the scores in the study, which might have influenced the results between the 2 groups. A prospective, double-blind randomized controlled trial would eliminate these potentially confounding factors.
CONCLUSION
All patients with acute infection at the surgical site presented with surgical site pain and fever. All 25 patients with infection at the surgical site yielded positive bacteriologic cultures. In the normal saline group, sixteen patients were positive for Staphylococcus epidermidis, and 9 patients were positive for Staphylococcus aureus. In this same group, 80% (20/25) of the patients with postoperative infection developed the infection within 3 wk (9-20 d).
ARTICLE HIGHLIGHTS
Research background
Total joint arthroplasty (TJA) is highly effective for reducing pain and improving quality of life in patients requiring joint replacement. However, implant infections remain a relatively rare but devastating complication associated with this procedure.Although improved sterile techniques, wound protection, minimization of contamination,and prophylactic antibiotics (systemic or local antibiotics) have markedly reduced the incidence of surgical site infection following TJA, implants may become infected by direct contact with an infected wound during the procedure or by spread of a superficial wound infection to the fascia lata or bloodborne contamination during or after the procedure. Intraoperative contamination of the surgical wound by bacterial seeding from the air of the operating room, the skin of the patient, or fallen debris or hair from surgical staff is an important cause of surgical site infection following TJA. In addition, TJA can lead to hematoma formation, which creates conditions that encourage bacterial growth, and bacteria can form biofilms that protect them from antimicrobials and the patients’ immune response, thus making eradication difficult.
The incidence of postoperative wound infection is estimated to be 0.5%-2% following primary TJA and 3%-7% following revision TJA. Local application of an antibiotic solution may reduce the contamination of wounds with commensal bacteria from the patient’s skin or with airborne bacteria during TJA. Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery.
Research motivation
29.Pumpkin:Besides being a suitable shape for a carriage, a pumpkin has several symbolic82 meanings beyond Halloween imagery. A pumpkin symbolizes83 feminine containment84, the moon, witches, and a charm against evil spirits (Olderr 1986).Return to place in story.
One day in mid-August, I was in the school office when Timmy s teacher came running in with Timmy. He was sobbing3 and the teacher was nearly hysterical4. The bathroom door had slammed on his finger. She had a handkerchief wrapped around Timmy s index finger and wasn t sure how much of it was left because it was bleeding so much. Our school bus driver rushed them immediately to the Emergency Room.
Research objectives
No significant differences in wound healing or the incidence of complications were observed between the vancomycin group and the normal saline group.
Roma sighs heavily and continues. It is hard to describe how we felt about each other-after all, we were young, and we only exchanged a few words when we could-but I can tell you, there was much love there. I assume he was killed like so many others. But I cannot bear to think that, and so I try to remember him as he was for those months we were given together.
Could it be 20 years already? I shuddered3. Cold chills went up and down my spine4 as tiny beads5 of sweat popped out on my forehead. What had I done with my life the past 20 years? My mother told me I’d have to deal with this some day, but I had laughed it off, just like I laughed off those embarrassing pink plastic curlers she used to wear in her hair. (I picked up a set at a garage sale just last week. Got a great deal on them, too!)
What does a frog want with thee? Ah, dear father, yesterday as I was in the forest sitting by the well, playing, my golden ball fell into the water. And because I cried so, the frog brought it out again for me, and because he so insisted, I promised him he should be my companion, but I never thought he would be able to come out of his water! And now he is outside there, and wants to come in to me.
Research methods
One surgeon performed all the procedures in the given time period. Patients were identified, and data related to patient demographics, baseline characteristics, and comorbidities and operative data were collected from medical records. These cases were retrospectively reviewed for the occurrence of surgical site infections within 3 mo after surgery. Each patient received standard antibiotic prophylaxis (2 g cefazolin)approximately 30 min before surgery. Antibiotic-loaded cement was used in patients with a higher risk for infection due to a body mass index of > 35, diabetes mellitus, or rheumatoid arthritis.
Research results
There were no significant differences in sex, age, duration of surgical procedure, or use of antibiotic-loaded cement between the two groups. There was a significantly higher incidence of acute infection at the surgical site in patients who received intrawound irrigation with normal saline prior to wound closure than in patients who received intrawound irrigation with vancomycin solution prior to wound closure. The overall incidence of infection in group 1 was 2.46%, and that in group 2 was 0.09%.
Research conclusions
Prophylactic irrigation with vancomycin solution significantly reduces the incidence of infection after primary TJA. This strategy is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
Research perspectives
Prophylactic irrigation with vancomycin solution is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
