Cerebral venous sinus thrombosis in pregnancy: A case report
INTRODUCTION
Cerebral venous thrombosis (CVT) is a rare and severe disease. A recent study found that approximately one-third of CVT patients did not return to paid work, and this was more common in women and patients with parenchymal lesions[1]. According to the 2017 European ESO/EAN Guidelines, anticoagulation is the main therapeutic regimen for CVT in clinical practice[2]. However, some patients have poor outcomes despite anticoagulation. Studies have demonstrated the benefits of endovascular therapy with respect to CVT recanalization[3]. However, due to the low-level of available evidence, the 2017 European guidelines do not make any recommendations, and specific analyses regarding pregnant populations are limited. Here, we report a rare case of CVT in a pregnant woman who underwent endovascular mechanical thrombectomy using two stent retriever devices.
CASE PRESENTATION
Chief complaints
A 29-year-old female in the 8week of her first pregnancy presented to the Obstetrics Department of a referral hospital. The patient had nausea, vomiting and persistent headaches for one week prior to admission. Due to severe nausea and vomiting in pregnancy, she was first diagnosed with hyperemesis gravidarum.
History of present illness
A persistent headache with nausea and non-projectile vomiting occurred 1 wk previously. The headache was mainly characterized by mild-to-moderate, pulsatile headache on both sides of the temple, which was more obvious when shaking her head. The patient had no other discomfort such as fever, blurred vision, hemiplegia, consciousness disturbance, seizures,.
History of past illness
About 8 wk previously, the patient’s menstruation ceased. Two weeks ago, she was treated with oral progesterone to prevent miscarriage due to a small amount of intermittent vaginal discharge. She denied a history of hematologic disorders, autoimmune diseases, intracranial and extracranial tumors.
Many people are in the same situation that I was in. If your friend is saying threatening stuff like my friend was, then they obviously need help-soon. It seems like when one school shooting happens, then another one occurs not too long after that. If there were any way that you could prevent one school shooting it could perhaps save your own life and many others as well. If I had to do it over again, I would-because it really was for the best.
Personal and family history
The patient denied taking oral contraceptives and denied a family history of hereditary thrombophilia.
One day, Amberly and I were talking about what he had said when the teacher overheard our conversation. She took me out into the hallway and made me tell her who had said it and what they had said. At first, I refused to say a word. She told me it really was for the best, so I told her. I felt awful for doing it. I was angry with her for making me tell who said it. I wasn t sure he really meant it and didn t want him to get into trouble.
Physical examination
Due to its superior diagnostic accuracy, MRI is the most suitable option for diagnosing CVT in pregnant women, especially as it does not expose them to radiation, and it clearly differentiates soft tissues. Recent studies have shown that MRI performed with a 1.5-T magnet is safe for diagnosis in pregnant women at all trimesters[8].
Laboratory examinations
So the other trolls had to come and wash, but, the more they did, the blacker and uglier grew the shirt, until at length it was as black as if it had been up the chimney. Oh, cried the Prince, not one of you is good for anything at all! There is a beggar-girl sitting outside the window, and I ll be bound that she can wash better than any of you! Come in, you girl there! he cried. So she came in. Can you wash this shirt clean? he cried. Oh! I don t know, she said; but I will try. And no sooner had she taken the shirt and dipped it in the water than it was white as driven snow, and even whiter than that. I will marry you, said the Prince.
Imaging examinations
Anticoagulation constitutes the first-line therapeutic option for managing the acute stage of CVT. LMWH has been confirmed to be preferable to unfractionated heparin, as it results in reduced mortality as well as better functional outcomes, with equivalent rates of systemic bleeding[9]. Furthermore, in special populations, such as pregnant women, LMWH cannot traverse the placenta, and adverse reactions associated with teratogenicity or fatal bleeding have not been reported. Therefore, it is a reasonable choice of anticoagulation therapy for CVT patients during pregnancy[10].
In the International Study on Cerebral Vein and Dural Sinus Thrombosis, approximately 13% of cases had poor outcomes even after anticoagulation treatment[7]. The 2017 European ESO/EAN Guidelines recommend that patients with acute CVT who are at a low risk of adverse consequences before treatment should not undergo endovascular treatment.

FINAL DIAGNOSIS
The patient was diagnosed with CVT.
TREATMENT
Anticoagulant treatment with subcutaneous low molecular weight heparin (LMWH) administered twice a day was initiated. However, 3 d after admission, her symptoms worsened. The patient developed a right-sided weakness (4/5), and a progressive left limb weakness (3/5). Subsequent MRI confirmed new lesions in the right frontal lobe and left parietal lobe. Selective catheterization of the right internal carotid artery confirmed occlusion of the superior sagittal sinus, as well as the right transverse sinus, and sinus sigmoideus (Figure 2A and B). Despite anticoagulation, the patient’s neurological condition declined; therefore, emergency mechanical thrombectomy was performed. She successfully attained occluded superior sagittal sinus recanalization, as well as right transverse sinus, and sinus sigmoideus recanalization (Figure 2C-G). Microscopic appearance of the cerebral embolus specimen was consistent with a mixed thrombus (Figure 2H). As there were some residual thromboses, she continued LMWH therapy on the first post-procedure day. Immediately after the procedure, her headache diminished.

OUTCOME AND FOLLOW-UP
During the part-time employment at Warner Village Theme Parks, I learnt to work with a team and the great teamwork made me get used to work under pressure. This is really an excellent job, and I had a lot of fun in working, for most of the customers are very friendly and nice. A lot of people who were working with me are local university students. I was impressed that lots of Australian students afford their tuition6 fees by themselves through part-time employment. Compared with the Chinese students, the Australian young people are more independent from the families since they become 18 years old.
Three weeks after the procedure, the patient was completely independent (modified Rankin Scale score = 0), and at a 3-mo follow-up, symptomatic relapse was not reported.
DISCUSSION
Primary headaches, such as tension headaches and migraines, frequently occur in pregnant women and are the most common causes of headaches[4]. However, if pregnant women experience new, deteriorating headaches or when the headaches change in character, secondary origins may exist[5]. Pregnancy is a risk factor for secondary headache disorders. Anesthesia for labor, hypercoagulability, as well as hormonal changes are factors for the high incidence of secondary headaches during pregnancy. The most frequent causes of secondary headaches include stroke, subarachnoid hemorrhage, pituitary tumors, CVT, and reversible cerebral vasoconstriction syndrome[4].
Pregnancy is an important risk factor for CVT. In pregnancy, CVT has a prevalence of 1.2 per 100000 deliveries[6]. An increase in prevalence within the 1trimester is associated with women who have pre-existing thrombophilia who become pregnant. Given its rare incidence and highly diverse clinical manifestations, the clinical diagnosis of CVT is challenging. High incidences of headaches, motor weakness, seizures, and comatose/obtunded status have been reported, in tandem with clinical manifestations among non-pregnant/puerperal patients[7].
On admission, the patient’s main symptoms were a persistent headache, nausea and vomiting. Her vital signs and muscle strength were normal. Three days after admission, she developed a new left-sided motor weakness (4/5). Neurologic consultation was recommended. Neurological examination showed poor spirit, left limb weakness (4/5), neck stiffness, positive Kernig’s sign and positive Babinski's sign on the left. No other focal neurological deficits were found.
Ultrasound scan was performed, which showed a fetus at 8 wk of gestation (Figure 1A). Prethrombectomy brain magnetic resonance imaging (MRI) combined with magnetic resonance venography revealed superior sagittal sinus, right transverse sinus and sinus sigmoideus thrombosis with a right temporal lobe venous infarct (Figure 1B and C). Post-thrombectomy MRI revealed new lesions in the right frontal lobe and left parietal lobe (Figure 1D).
Cerebrospinal fluid pressure was 220 mmHO, cerebrospinal fluid cell count and protein were nearly normal, and β-human chorionic gonadotropin was 150073 IU/L. Her D-dimer level was 12.5 mg/L. Other laboratory tests were normal, such as routine blood tests, coagulation function, routine urinalysis, liver function, kidney function, homocysteine, protein C, protein S and so on. Due to an acute onset of neurologic symptoms, and objective findings upon neurologic examination, the most probable diagnosis was CVT.
When they had reached the middle of the forest the father said: Now, children, go and fetch a lot of wood, and I ll light a fire21 that you may not feel cold
Currently, although there are no randomized controlled trials regarding the effectiveness and safety of endovascular treatment for CVT, more and more evidence has shown that mechanical thrombectomy is a safe and effective treatment for CVT[3,11]. A 2017 review of 235 patients with CVT and a neurologic presentation described the effectiveness and safety of endovascular treatment for CVT. They found that although 40.2% of patients presented with poor baseline characteristics (encephalopathy or coma), 69.0% of patients achieved complete radiographic resolution of CVT after endovascular treatment, 76% of patients achieved a good clinical outcome (a modified Rankin Scale score of 0-2), and the rate of worsening or new intracranial hemorrhage was only 8.7%.
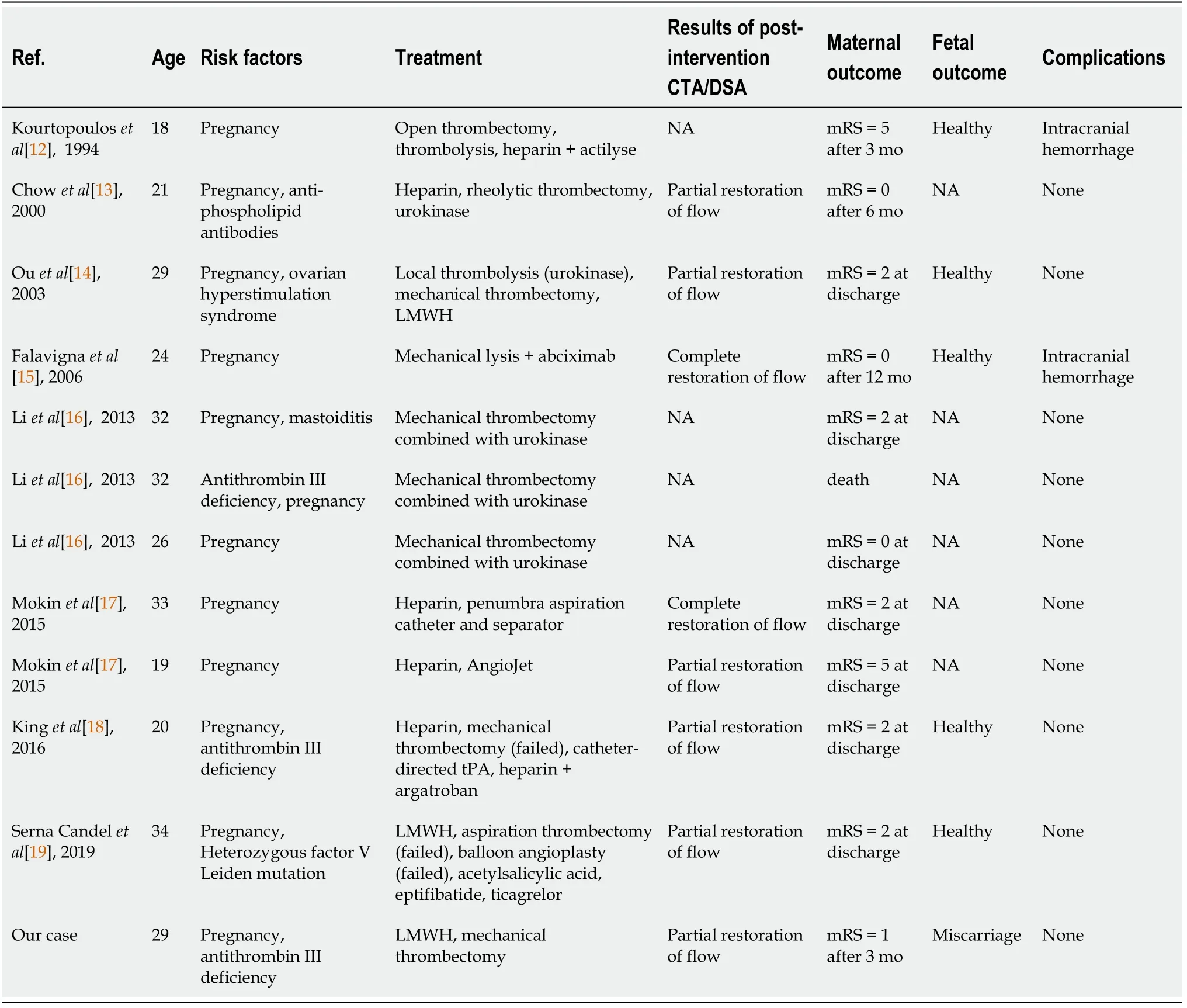
However, studies on the efficacy and safety of mechanical thrombectomy for CVT in pregnant women are mainly limited to case reports and small series. To date, there are only 12 case reports of mechanical thrombectomy for the treatment of CVT in pregnant women. Table 1 summarizes the reported cases of CVT in pregnant women treated with mechanical thrombectomy from the literature along with our patient[12-19]. In addition to pregnancy, most patients (7/12) have other risk factors, such as antithrombin III deficiency and so on. Because of consciousness disorder or rapid deterioration of neurological function, all the patients underwent thrombectomy with or without thrombolysis. In two patients, thrombectomy resulted in complete restoration of flow (2/8) and in the remaining 6 patients (6/8) partial restoration of flow was achieved. Following thrombectomy, two (2/12) patients experienced non-fatal intracranial hemorrhage, 9 (75%) patients had a good clinical outcome and one patient died.
With regard to the safety of radiation exposure on fetal growth during an endovascular procedure, due to the distance between the mother's head and the uterus, the absorbed fetal radiation dose during endovascular treatment was only 2.8 mGy, which was much less than the risk threshold, and this had very little effect on the fetus[20]. The present review showed that the condition of the fetus was not mentioned in half of the 12 pregnant patients. One pregnancy ended in miscarriage, and five fetuses were normal at the time of discharge or follow-up. None of the infants was found to have either congenital anomalies or neonatal morbidity and mortality.
And true to his word, that little elf began to do Patrick s homework. Except there was one glitch4. The elf didn t always know what to do and he needed help. Help me! Help me! he d say. And Patrick would have to help -- in whatever way.
Therapeutic guidelines for CVT in pregnant women are difficult to establish, as the incidence of CVT in pregnancy is rare. If a patient presents with a new persistent headache and abnormalities on neurologic examination during pregnancy, obstetricians and neurologists should consider CVT, and MRI should be performed immediately. If the condition worsens during anticoagulant therapy, mechanical thrombectomy may be a good remedial treatment option.
CONCLUSION
Cerebral venous thrombosis is easily misdiagnosed or missed due to its rarity, diverse, and non-specific clinical manifestations during pregnancy. Prompt multidisciplinary diagnosis and treatment is essential. Our case and those reported in the literature show that mechanical thrombectomy may be an effective alternative therapy for CVT in pregnant women who do not respond to standard management.
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Hepatitis B virus reactivation in rheumatoid arthritis
- Paradoxical role of interleukin-33/suppressor of tumorigenicity 2 in colorectal carcinogenesis: Progress and therapeutic potential
- Changes in rheumatoid arthritis under ultrasound before and after sinomenine injection
- Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients
- Outcomes and complications of open, laparoscopic, and hybrid giant ventral hernia repair
- Surgical resection of intradural extramedullary tumors in the atlantoaxial spine via a posterior approach
