Complex proximal femoral fracture in a young patient followed up for 3 years: A case report
INTRODUCTION
Proximal femoral fractures (PFFs) are one of the most common orthopedic injuries, which mainly occur in the elderly and are uncommon in young people[1,2]. PFFs mainly refer to femoral head fracture, femoral neck fracture, and intertrochanteric fracture, while ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare. PFFs in young patients are mostly caused by high-energy trauma[3,4]. The fracture mechanism, bone quality, and treatment requirements of young patients are different from those of elderly patients. Although there are a large number of reports of PFFs in elderly patients, there is no reference for the treatment of young patients, especially those with ipsilateral femoral neck and intertrochanteric fractures. Therefore, we report the case of a 27-year-old patient who sustained a complex proximal femoral fracture that involved ipsilateral femoral neck and intertrochanteric fractures. The literature on ipsilateral femoral neck and intertrochanteric fractures was also reviewed.
CASE PRESENTATION
Chief complaints
A 27-year-old male patient was admitted to the Department of Orthopedics of our hospital with left hip pain and limited mobility 5 h after a car accident.
History of present illness
The patient was involved in a car accident 5 h previously and underwent clinical and radiological examinations due to left hip pain and limited mobility.
History of past illness
The patient had no previous medical history.
Then their marriage had to be celebrated17, for the witch had to stick to what she had promised, and he must get the princess whatever might happen afterwards
Personal and family history
At 12 mo postoperatively, X-rays showed that the fractured end of the femoral neck had collapsed, the cervico-diaphyseal angle had reduced, and the fracture lines were blurred (Figure 2C). The fractures had healed completely, and complications such as hip varus deformity and slight limitation in the range of motion of the hip joint were observed. However, there were no complications such as necrosis of the femoral head and hip pain. The HHS was 91. The patient did not engage in exercise-related work, and his hip function after surgery met his life and work needs.
We left the orphanage on Christmas Eve at midnight. My tiny daughter, Noelle Joy Oksana Brani, was wrapped in a soft pink blanket. As I walked out into the night to catch the train back to Moscow, the snow was gently falling. And I thought I could hear the angels singing.
Physical examination
At 24 mo (Figure 2D) and 36 mo postoperatively, X-rays were similar to those at 12 mo postoperatively, and the hip varus deformity did not significantly worsen. The HHS was 93. No complications such as necrosis of the femoral head and hip pain were observed.
Laboratory examinations
After confirming the patient's fractures, we immediately performed skeletal traction of the left lower extremity tibial tubercle and provided symptomatic treatment such as analgesia and elimination of swelling before surgery.
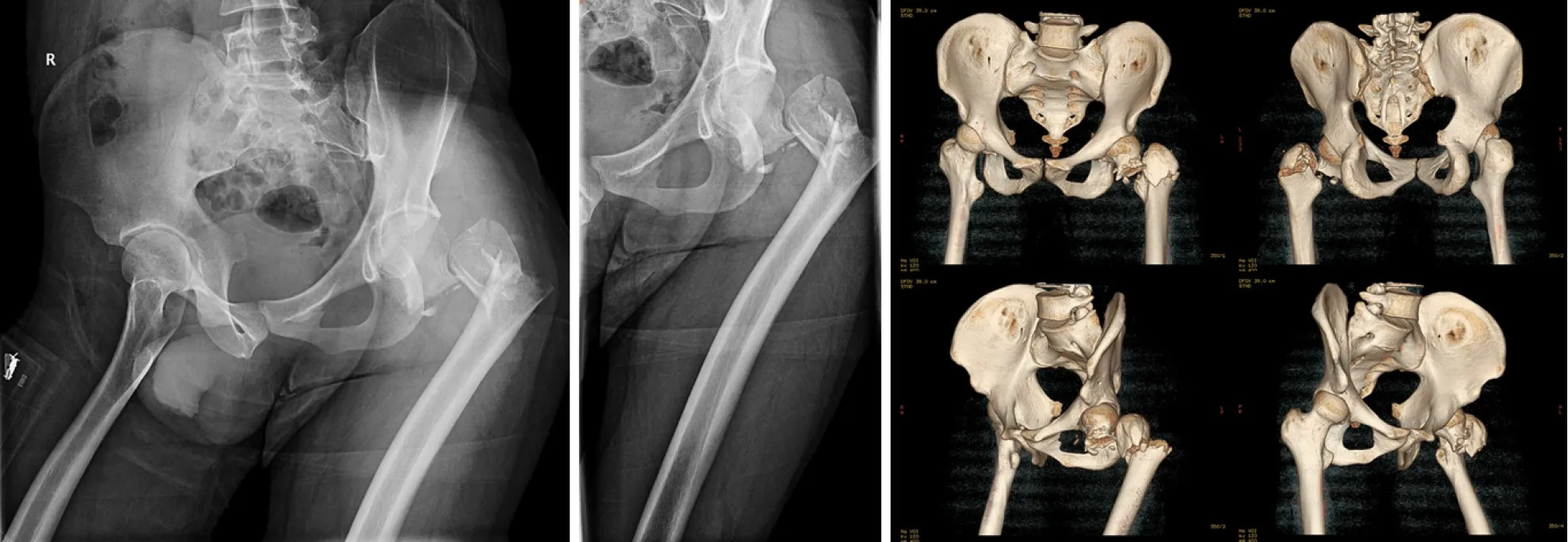
Imaging examinations
Radiological examinations including X-rays and three-dimensional computed tomography of bilateral hips showed that the femoral neck base fracture was accompanied by a greater trochanteric comminuted fracture, and the displacements were obvious (Figure 1).
FINAL DIAGNOSIS
Due to the lack of suitable fracture classification criteria, we defined the patient's fractures as complex proximal femoral fractures.
The patient received symptomatic treatment such as anti-infection and elimination of swelling after surgery. Postoperative X-rays showed that the fractures were well reduced, the cervico-diaphyseal angle of the femur was satisfactory, and the internal fixation position was normal (Figure 2A). The patient was discharged 1 wk after surgery and was instructed to rest in bed, raise the affected limb, strengthen lower limb muscle function by exercising and avoid weight-bearing. He was followed regularly, including physical and radiological examinations.
TREATMENT
Preoperative skeletal traction and symptomatic treatment
No abnormalities were detected on preoperative examinations.
Finally I came to a rest area and pulled in. I sagged23 back in the seat. I unclenched my hands and looked at my fingers, white and bent24. The presence I felt so strongly inside the car began to fade, and with it went the last residue25 of the fear that had gripped me these past several days. It drained from me like a poison. I closed my eyes and said a prayer of thanks before putting the car in gear and returning to the highway.,。,,。,,,。,,。
On Tuesday of that week, while we all ate lunch together, I asked “our family’s” three boys, Josh, Eric and Ryan, What do you want for your new room? Anticipating posters, toys and other gadgets2 that children usually ask for, we were surprised when Josh, the oldest, responded, I just want a bed.
Surgical procedures
A collective discussion on the patient's condition and surgical plan was held which mainly consisted of selection of the internal fixation method. Considering the complicated fractures and obvious displacements, we planned to perform open reduction and internal fixation. The fixation methods for proximal femoral fractures mainly included intramedullary fixation such as proximal femoral nail anti-rotation (PFNA) and extramedullary fixation such as a proximal femoral locking compression plate (PFLCP). In order to ensure the success of the operation, we prepared both intramedullary and extramedullary fixation systems before surgery[5-9].
Following skin and soft tissue incision, the femoral neck base fracture and the greater trochanteric comminuted fracture were found under direct vision. We first used towel forceps and Kirschner wires to sequentially reduce and fix the proximal fractures, including the comminuted intertrochanteric fracture and femoral neck fracture. Then the distal and proximal femoral fractures were reduced by lower limb traction and temporarily fixed with Kirschner wires. The C-arm X-ray machine showed that the fracture reduction and cervico-diaphyseal angle of the femur were satisfactory. Considering that the greater trochanteric comminuted fracture was difficult to maintain by intramedullary fixation such as PFNA, the PFLCP was used. In addition, wire binding was used to strengthen fixation of the intertrochanteric comminuted fracture. Finally, the C-arm X-ray machine was used to further ensure anatomical reduction of the femoral neck and intertrochanteric fractures.
OUTCOME AND FOLLOW-UP
The whole city spoke of the wonderful bird, and when two people met, one said “nightin,” and the other said “gale,” and they understood what was meant, for nothing else was talked of. Eleven peddlers’ children were named after her, but not of them could sing a note.

At 1 mo postoperatively, X-rays showed that a small amount of callus had formed around the greater trochanter, and the internal fixation position was normal. The Harris Hip Score (HHS) was 39. The patient was instructed to perform lower limb functional exercise without weight-bearing in bed.
At 3 mo postoperatively, X-rays showed that the fracture lines were blurred (Figure 2B). The HHS was 62. The patient was permitted to walk with partial weightbearing using a walker, and gradually increase weight-bearing.
There was no previous medical history.
Desiree went off to preschool and I returned to college to finish my degree, and I tried to find myself in the courses I took; I complained with all the other young women on campus about men who are insensitive. Sometimes late at night I cried and begged the whispering darkness to tell me who I really was, and my husband lay beside snoring like a hibernating7 bear unaware8 of my winter.
The patient’s left lower limb showed external rotation malformation, which was shorter than that of the healthy side. The patient's peripheral sensation and blood flow were normal, and there were no clinical manifestations of vascular and nerve damage.
DISCUSSION
Fractures such as PFFs mainly occur in the elderly, mostly due to low-energy injury. However, high-energy injuries, such as car accidents and fall injuries, have led to an increasing number of PFFs in young patients[1,3]. PFFs mainly include femoral head fracture, femoral neck fracture, and intertrochanteric fracture. Cannulated screw internal fixation is most commonly used for femoral neck fracture in young patients[10]. Non-weight bearing is required for at least 8 wk after surgery, and weight bearing is resumed gradually when the radiological examination shows fracture healing progress[10-13]. The most common complications include nonunion, varus collapse, limb shortening, and osteonecrosis[10-13]. PFNA internal fixation is most frequently used for intertrochanteric fracture in young patients, and the patients are advised to get out of bed as soon as possible for gradual weight bearing training[8,9]. The most common complications include limb shortening and coxa vara[8,9]. Anatomical reduction, effective internal fixation, and rehabilitation exercises are the main strategies to avoid complications. The ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare, and there is no good reference for the classification and internal fixation of this complex proximal femoral fracture.
The goal of treatment in young patients with PFFs is to preserve the femoral head and prevent osteonecrosis and pseudoarthrosis to avoid total hip replacement[14]. The early treatment and correct choice of implant to achieve anatomical reduction and effective internal fixation are essential. The fixation methods for intertrochanteric fracture in young patients mainly include PFNA and PFLCP[5-9].
Not a house was to be seen; the only shelter he could get was the hollow trunk of a great tree, and there he crouched19 all the night which seemed to him the longest he had ever known
In 2016, Giancola[14] reported a 39-year-old patient with a complex proximal femoral fracture that involved the neck and trochanteric region. The multifragmentary comminution of the femoral neck associated with rupture of the greater trochanteric region, without involving the lesser trochanter was treated with skeletal traction in the first stage and then implantation of an intramedullary nail. Twenty months after surgery, the fractures were healed and the patient was able to walk and run without pain. Giancola[14] suggested that early surgery and suitable internal fixation options were essential in the treatment of the patient and the transverse component of the proximal femur fracture determined the choice of intramedullary nail.
In 2018, Su[15] reported two cases of ipsilateral femoral neck and intertrochanteric fractures with posterior dislocation of the hip. A 38-year-old patient was diagnosed with femoral neck fractures, intertrochanteric fractures, and dislocation of the hip, and was finally treated with skeletal traction in the first stage and then internal fixation with a LCP. However, one year after surgery, the patient developed hip pain and osteonecrosis of the femoral head. Seven years after surgery, the patient suffered from hip pain and refused further examination and treatment. Another 29-year-old patient was diagnosed with ipsilateral femoral neck fractures and intertrochanteric fractures with posterior dislocation of the hip. Preoperative traction was not used, and the patient was treated with internal fixation using a LCP. After 3 years of follow-up, the patient had good hip function and no complications such as hip pain and necrosis of the femoral head. Su[15] suggested that internal fixation should be selected according to the specific fracture conditions of each patient. The fractures in these two patients were complicated and split vertically. A LCP is a strong structure for stable vertical shear fracture of the femoral neck. In addition, close contact with the bone surface is unnecessary and it can be bent to match the femoral shape, thus protecting the blood supply of the periosteum.
In this study, we report a 27-year-old male patient who was involved in a car accident. The radiological examinations showed that the femoral neck base fracture was accompanied by a greater trochanteric comminuted fracture, and the displacements were obvious. After confirming the patient's fractures, skeletal traction of the left lower extremity tibial tubercle was performed and he received symptomatic treatment such as analgesia and elimination of swelling before surgery. Considering that the greater trochanteric comminuted fracture was difficult to maintain by PFNA, a PFLCP was used[2,16,17]. In addition, a PFLCP can be used as a stress barrier in the lateral wall of the trochanter to prevent lateral movement of the proximal femoral fracture fragments, and has a strong antagonistic effect on the rotation and bending of the femoral neck. The multiple locking screw holes of the PFLCP provide a variety of options to overcome any complex fracture pattern and can minimize pressure on the periosteum, thereby promoting rapid biological healing[3,9,18].
Postoperative X-rays showed that the fractures were well reduced, the cervicodiaphyseal angle was satisfactory, and the internal fixation position was normal. At the last follow-up three years after surgery, the patient had no obvious pain in the hip, and the range of motion of the hip joint was slightly limited, but it met the normal life and work needs of the patient. The HHS was 91. X-ray examinations showed that the fractured end of the femoral neck had collapsed, the cervico-diaphyseal angle had reduced, and a hip varus deformity was observed. However, there were no complications such as necrosis of the femoral head. The patient was satisfied with the prognosis of the fractures.
CONCLUSION
Ipsilateral femoral neck fractures and intertrochanteric fractures in young patients are extremely rare and lack appropriate fracture classification criteria and treatment guidelines. Therefore, this type of case report is of great significance. Early diagnosis and treatment, as well as appropriate internal fixator selection, are essential for the treatment of such complex fractures. As an important treatment before surgery, skeletal traction should be performed as soon as possible. A PFLCP can be used to treat this complex proximal femoral fracture, and selection should be based on the patient's specific fractures.
 World Journal of Clinical Cases2022年1期
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity,transmission, and vaccine resistance
- Clinical manifestations and prenatal diagnosis of Ullrich congenital muscular dystrophy: A case report
- Lunate dislocation with avulsed triquetral fracture: A case report
- Protein-losing enteropathy caused by a jejunal ulcer after an internal hernia in Petersen's space: A case report
- Eustachian tube teratoma: A case report
- Cerebral venous sinus thrombosis in pregnancy: A case report
