Intraoperative thromboelastography-guided transfusion in a patient with factor XI deficiency: A case report
INTRODUCTION
Hemophilia C, or factor XI (FXI) deficiency, is a rare autosomal coagulation disorder[1]. Patients may be asymptomatic until they are hemodynamically challenged following trauma or surgery. In other cases, these coagulopathies are discovered as incidental laboratory findings along with other medical conditions. The unpredictability of bleeding patterns often poses perioperative challenges for clinicians[2]. Thromboelastography (TEG) is a method that is used to monitor and analyze the viscoelastic properties of blood clot formation and lysis. It has the advantages of working with the patient’s whole blood, providing real-time quantitative results on global hemostasis assessments[3]. Its adaptability for point-of-care (POC) testing makes this test particularly useful for intraoperative blood transfusion guidance. Here, we present a case in which the patient was diagnosed with FXI deficiency during a preoperative workup for macrodactyly reconstructive surgery. POC-TEG monitoring was successfully used to help assess the need for intraoperative transfusion.
CASE PRESENTATION
Chief complaints
A 21-year-old man was scheduled to undergo reconstructive surgery for macrodactyly of the left foot under general anesthesia.
Then, at last, I found a dish their mama didn t make – one both the kids liked – banana pudding. They helped me in the kitchen. Chuck beat the egg whites for the topping while Cheryl carefully lined the pan with vanilla14() wafers. I cut up the bananas and prepared the filling. They both licked the bowl. We all had fun. It was a time of sharing and laughter.
History of present illness
The patient presented with significant enlargement of his left foot since birth, complicated by recurrent episodes of paronychia. He was scheduled to have reconstructive surgery at a local hospital. However, the surgery was deferred due to the unexpected perioperative discovery of abnormal coagulation studies.
History of past illness
The patient denied a previous history of easy bleeding or bruising.
Preoperative hematology consultation suggested empirically giving fresh frozen plasma (FFP) as prophylactic FXI replacement at a dose of 15-20 mL/kg body weight (patient weight 60 kg, prophylactic dose 900-1200 mL FFP) before surgery. Subsequent FFP transfusion would be adjustedsurgical need. Oral tranexamic acid was suggested for one week postoperatively.
Physical examination
“My dear goose and gander, our kingdom is in danger. Take my daughter to a safe place on top of the tallest hill, said the king. So the grey goose and gander flew the princess who sat in a red sheet over the one-strand river to the top of the tallest hill.
The youngest, however, said, Dear father, that must be a good man to have helped you out of your trouble, so if you have promised him a bride for doing it, your promise must be kept
Laboratory examinations
The diagnosis of FXI deficiency was confirmed by a hematologist.
FINAL DIAGNOSIS
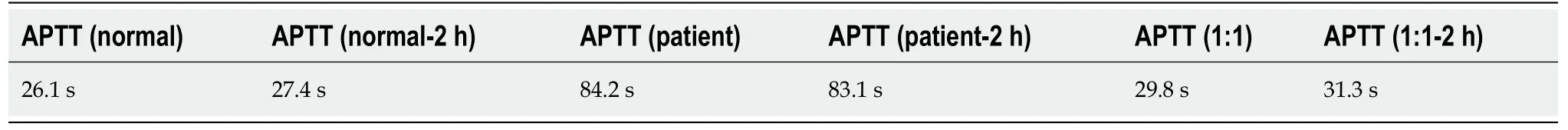
Preoperative laboratory workup showed an increased activated plasma thromboplastin time (APTT) of 83.9 s (reference: 23.3-32.5 s), a normal prothrombin time (PT) of 12 s (reference: 10.4-12.6 s), and an internationalized normal ratio (INR) of 1.04 (reference 0.86-1.14). Further workup revealed the patient’s FXI activity to be 3%. The mixing study (Table 1) showed that the patient’s APTT could be corrected by mixing his plasma 1:1 with normal serum to achieve normalization of coagulation function.
TREATMENT
I can still hear her voice encouraging me on my first date. “Go,” she ordered. “Have fun,” she smiled. “And don’t let him touch you,” she warned. And when I was older, and a date had left me waiting while he went out on the boardwalk with someone else, my mother found him and later told me, “I gave him a piece of my mind.” Though mortified8 at the time by her behavior, it is a memory I cherish9.
Hemophilia C caused by a deficiency of FXI is a rare autosomal inherited coagulopathy. FXI plays an important role not only in initiating clot formation but also in supporting clot consolidation. Conventional coagulation tests such as PT and APTT are less than satisfactory in the assessment of hemophilia C patients’ clinical profiles and bleeding risks. These tests are limited because they are endpoint assays that test only the speed of blood clot formation. However, they cannot reflect the process of further thrombin formation involved in clot consolidation and maintenance. Compared with hemophilia A and B, the clinical profile and bleeding management of hemophilia C is less clearly understood (Table 2). The relationship between bleeding phenotypes and baseline FXI level is poor, making perioperative bleeding risk hard to predict and manage[4].
OUTCOME AND FOLLOW-UP
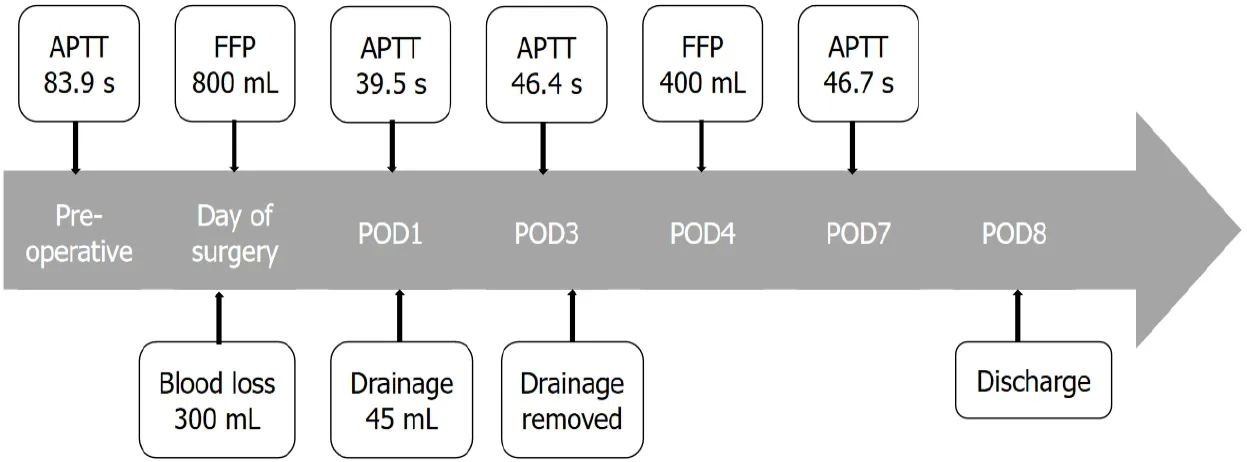
The patient had an uneventful postoperative course (Figure 2). Oral tranexamic acid 0.5 g three timesday was prescribed for one week. Surgical site drainage was 45 mL on postoperative day (POD) 1 and then decreased to a minimal level. The drain was removed on POD3. The patient received 400 mL FFP on POD 4 due to concerns of prolonged elevation of APTT levels (46.4 s, reference: 23.3-32.5 s), while the surgical dressing remained dry and clean. He was discharged on POD 8.
DISCUSSION
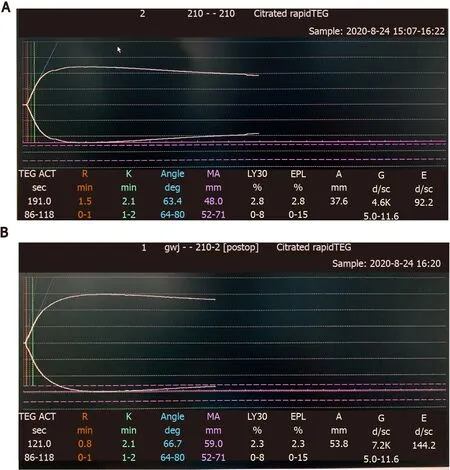
On the day of surgery, the patient received 400 mL FFP preoperatively. The first set of TEGs (Figure 1A) performed immediately after FFP transfusion showed moderately increased activated clotting time (ACT), R time, K time, max amplitude (MA), and alpha angle. The operation was performed under general anesthesia and lasted approximately 4 h. A tourniquet was applied above the knee to minimize blood loss. Continuous nasal temperature monitoring was used to ensure no intraoperative hypothermia was experienced. The patient received 2000 mL of Ringer’s lactate and 400 mL FFP intraoperatively. Urine output was 1400 mL, and blood loss was estimated to be approximately 300 mL. The second set of TEGs (Figure 1B) performed toward the end of surgery showed improvements in all parameters.
There was significant swelling of the patient’s left foot without erythema, rash, or discoloration. The bilateral lower extremity pulses were equal. The patient had a normal gait. Motor and sensations were intact.
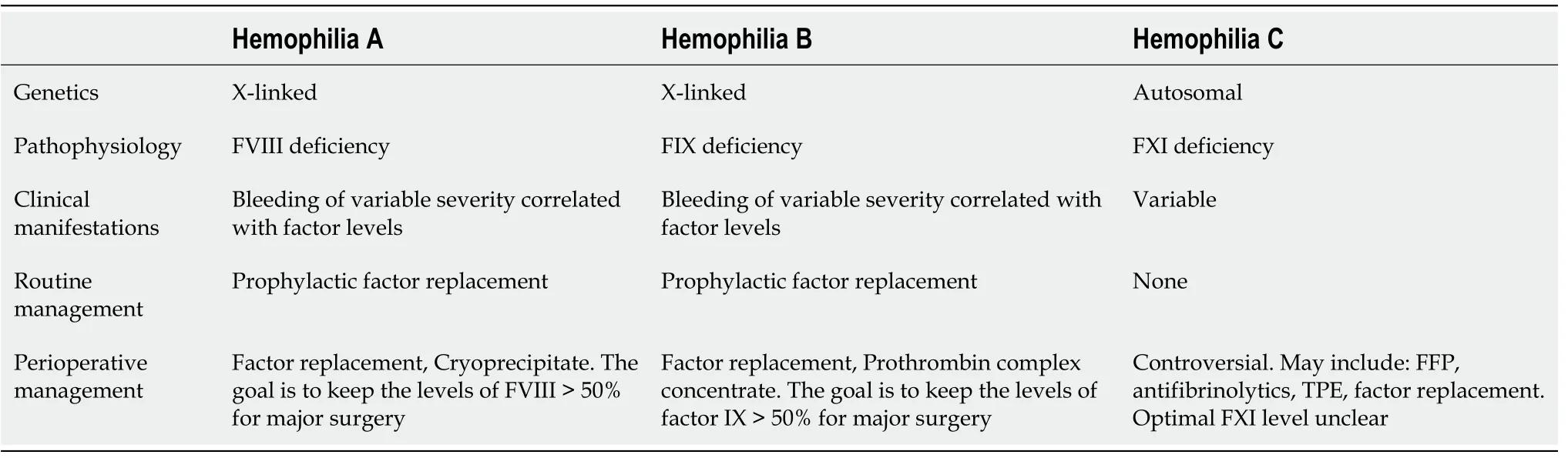
TEG is a method of testing the efficiency of blood coagulation using a whole bloodbased, viscoelastic hemostatic assay. It can provide a continuous assessment of the elastic properties of clot formation and lysis in both graphics and numbers. TEG measurements collected for analysis include reaction (R) time, coagulation (k) time, α angle, and maximum amplitude (MA), which are reflections of clotting factors, circulating inhibitory activity, fibrinogen and platelet levels and function,[5] TEG’s short turnaround time makes it a promising measurement tool for the assessment of global hemostasis in trauma or perioperative settings. It is better than conventional coagulation tests in monitoring coagulation profiles and predicting transfusion requirements[5]. It reduces the total amount of blood products transfused compared with an empiric transfusion policy or a transfusion protocol guided by conventional coagulation tests[6]. Study results from trauma[7], liver transplant[8] and cardiac surgeries[9] have shown that the goal-directed allogeneic transfusion strategy is believed to provide better hemostatic competence. This was possibly due to the more timely administration of blood products such as plasma and platelets, which in turn resulted in less blood loss[3], reduced blood transfusion needs[10], lower costs, and fewer adverse events[11] in the TEG-guided transfusion group than in the conventional transfusion group. One study also suggested that TEG-guided transfusion could substantially affect patient outcomes, including length of hospital stay, odds of reoperation, and short-term mortality[9]. For inherited coagulopathies such as hemophilia A and B, a combination of standard coagulation laboratory tests and TEG tests results in a better understanding of hemostasis in an individual patient, giving insights into their long-term hemostatic management[12], as well as providing vital insights in more pressing situations such as traumas or surgeries. In later cases, studies from hemophilia A and B patients suggested that TEG could be successfully used in perioperative settings to evaluate the efficacy of various hemostatic agents, such as factor VIII concentrate, cryoprecipitate, and prothrombin complex concentrates[3]. TEG has the potential to assess the role FXI plays in global hemostasis. However, its application in perioperative transfusion management for hemophilia C patients has not been extensively studied.
Normally, FXI-deficient patients will require careful, individualized and multidisciplinary preprocedural planning. Such planning starts with a meticulous assessment of the patient’s bleeding history and bleeding pattern. This is followed by thorough laboratory tests, including basic coagulation function tests, such as PT, APTT, and FXI levels, and mixing studies. Moreover, the nature of the scheduled procedure must also be taken into consideration. Operations on sites with higher fibrinolytic activities, such as the pharynx and urinary tracts, put patients at higher risk for bleeding[13]. The use of antifibrinolytic medication may help improve overall hemostasis[14]. For major procedures in individuals with severe FXI deficiency or with a significant bleeding phenotype, prophylactic replenishment using FXI concentrates or FFP is recommended in the preoperative period[1]. FXI concentrate has been associated with a higher thrombotic risk than FFP[15]. Some practitioners have suggested a “wait and watch” attitude with factor replacement, giving FXI concentrate only when excessive bleeding occurs. Prophylactic FFP replacement is the most commonly used option in our institute. However, this comes with the risk of volume overload. Because FXI levels do not correlate well with bleeding phenotypes, replacement therapy remains somewhat empirical. Therapeutic plasma exchange (TPE) may lower the risk of circulatory volume overload[16]. However, this is a complicated procedure with other transfusion-related adverse effects, and the added costs cannot be overlooked.
The patient we present here had no history of spontaneous bleeding and had no surgical history. This made the perioperative bleeding risk hard to predict and the prophylactic transfusion management strategy hard to plan. The consulting hematologists suggested a FFP loading dose of 15-20 mL/kg body weight to bring the FXI level within a satisfactory range (FXI: C, 30%-45%), which inevitably resulted in the need for a large volume of FFP. It is in this kind of situation that TEG monitoring is especially useful. TEG-guided prophylactic FFP replacement may allow for a more parsimonious use of replacement therapy in patients with severe FXI deficiency undergoing surgery. It can reduce the risks of volume overload, transfusion-related acute lung injury, transmission of infectious diseases, thrombosis, allergic reactions, and the development of inhibitors to FXI[13].Empirically, our patient was to receive a loading dose of 900-1200 mL FFP according to preoperative hematology consultation. In practice, however, based on the results from the intraoperative TEG monitoring, our patient received 800 mL FFP in total before and during the whole procedure with minimal blood loss and uneventful postoperative recovery. This experience is limited to a single case report. However, we believe that with improved TEG technology and accessibility, anesthesiologists and other medical practitioners will be able to provide transfusion therapy tailored to the need of each patient with FXI deficiency.
CONCLUSION
FXI deficiency is an underrecognized disorder with a wide range of clinical presentations and a poor correlation with coagulation studies. It poses great challenges for perioperative management. FXI concentrates, FFP, TPE and antifibrinolytic therapies are the mainstream treatments for FXI patients with surgical needs. POC-TEG could be readily applied in the perioperative period to individualize transfusion requirements on a case-by-case basis, providing guidance regarding the appropriate amount of blood products to be administered and thus minimizing transfusion needs and the associated risks. Further large-scale studies are needed to assess the potential for using TEG for perioperative transfusion guidance in the treatment of FXI patients.
 World Journal of Clinical Cases2022年1期
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity,transmission, and vaccine resistance
- Clinical manifestations and prenatal diagnosis of Ullrich congenital muscular dystrophy: A case report
- Lunate dislocation with avulsed triquetral fracture: A case report
- Protein-losing enteropathy caused by a jejunal ulcer after an internal hernia in Petersen's space: A case report
- Eustachian tube teratoma: A case report
- Cerebral venous sinus thrombosis in pregnancy: A case report
