Exploring the impact of COVID-19 on the movement behaviors of children and youth:A scoping review of evidence after the first year
Derek C.Pterson,Ktelynn Rmge,Srh A.Moore,Negin Rizi,Mrk S.Tremly,Guy Fulkner,*
a School of Kinesiology,Faculty of Education,University of British Columbia,Vancouver,British Columbia V6T 1Z4,Canada
b School of Health and Human Performance,Dalhousie University,Halifax,Nova Scotia B3H 4R2,Canada
c Children’s Hospital of Eastern Ontario Research Institute,Ottawa,Ontario K1H 5B2,Canada
d Department of Pediatrics,University of Ottawa,Ottawa,Ontario K1N 6N5,Canada
Abstract
Keywords: Pandemic;Physical activity;Screen time;Sedentary;Sleep
1. Introduction
The health-enhancing benefits of physical activity (PA), sleep,and a reduction in sedentary behavior and screen time have been well documented across all age groups and developmental stages,with specific and distinct implications for the healthy growth and development of children and youth.1-3This body of evidence has supported international (e.g., World Health Organization4) and national organizations worldwide in publishing clear guidelines stipulating the recommended volume and nature of movement behaviors (PA, sleep, and sedentary behavior/screen time) for all age groups,including school-aged children and youth(5-17 years old),for optimal health benefits.
A 2020 systematic review of national PA guidelines for children and adolescents identified 50 verified national and international guidelines.5All but 1 recommended 60 min of daily movement (with the majority referring to moderateto-vigorous physical activity (MVPA)), whereas 22 included sedentary behavior, and 3 included sleep recommendations.5A 2017 Canadian cross-sectional study examined the extent to which meeting the Canadian 24-h movement guidelines was associated with health outcomes in children.6It was found that meeting all 3 daily movement guidelines(≥60 min of MVPA,≤2 h of screen time,and 9-11 h of sleep(5-13 years old)or 8-10 h of sleep (14-17 years old)) was positively associated with improved aerobic fitness, lower body mass index, lower systolic blood pressure,and better overall health.6However,it was reported that only 17%of Canadian children were meeting the guidelines.6,7
On March 11, 2020, the World Health Organization declared the outbreak of coronavirus disease 2019 (COVID-19) a global pandemic.8In order to mitigate the spread and reduce the rates of transmission,governments across the world imposed varying lockdown measures, mandating the closure of many institutions, programs, facilities, and other community spaces as well as limitations on public use of community outdoor spaces.The duration, scale, enforcement, and adherence to these measures varied by jurisdiction and according to government mandates. Previous evidence concerning the correlates and determinants of PA,screen time/sedentary behavior,and sleep in children and youth suggests that it is likely that the restrictions imposed by the pandemic would result in adverse effects on these movement behaviors.9-12
A review of the evidence regarding children’s movement behaviors on structured school days as compared to during summer vacation and weekends found that children were more inactive on weekends and during summer vacations and exhibited greater usage of screens and electronic devices.13Additionally, later bed/wake times were reported on weekends when compared with weekdays.13Given that traditional stay-at-home conditions (i.e., weekends and summer breaks)eliminate daily structure for school-aged children and adolescents, it is reasonable to assume that similar effects would be observed during the COVID-19 pandemic and that they would fluctuate based on changes in those restrictions.
Given the extent and intensity of global lockdown measures,there is a need for research on the long-term consequences of pandemic-related restrictions on the movement behaviors of children and youth.Also of interest is the development of strategies to attenuate any undesirable changes in PA, sedentary behavior/screen time, and sleep during the ongoing pandemic.To date,2 reviews exist summarizing some movement behaviors during the pandemic.14,15Both examined populations across the lifespan, only one examined sedentary behavior,and neither included sleep studies;because of their focus on the entire lifespan,neither provided a comprehensive list of child and youth studies.That said,a review of all existing literature examining the relationship between COVID-19 and the movement behaviors of children and youth is important and required,and a scoping review is of particular relevance to the task.For Munn et al.,16a key difference between scoping reviews and systematic reviews is that in terms of a review question,a scoping review has a broader“scope”and more expansive inclusion criteria than does a traditional systematic review.As cited by Arksey and O’Malley,17a scoping review “aims to map rapidly the key concepts underpinning a research area and the main sources and types of evidence available” (p.194).18Arksey and O’Malley’s17methodological framework for scoping reviews identifies that scoping reviews may be undertaken to(1)examine the extent and nature of research, (2) summarize and disseminate findings,(3)evaluate the further need for a full systematic review,and(4)identify research gaps.Levac and colleagues,19in their provision of advancements to the scoping review methodology, suggest the relevance of scoping reviews within domains of research that are producing emerging evidence.19
With the recent and ongoing state of pandemic-related restrictions and the developing evidence base regarding COVID-19 and movement behaviors, a scoping review is appropriate as an initial step in comprehensively summarizing the collective evidence regarding the impact of COVID-19 on the PA, sleep, and sedentary behaviors of children and youth.Guiding this process were 2 questions: (1) How has the COVID-19 pandemic and associated restrictions impacted the movement behaviors of school-aged children? And (2) What factors contributed to observed differences in these behaviors during the pandemic?Synthesis of the research related to these questions will identify gaps in knowledge in order to inform further research and policies for health promotion amid the ongoing circumstances of the pandemic.
2. Methods
This scoping review was conducted in accordance with guidance from the Joanna Briggs Institute scoping review development guidelines20and Preferred Reporting Items for Systematic review and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR)/Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P)2015 checklists.21A protocol for this scoping review was registered on Open Science Framework on November 13,2020.22
2.1. Inclusion criteria
2.1.1. Participants
The review focused on school-aged children between the ages of 5 and 17 years. Children 0-4 years were excluded from this review because of distinct differences in 24-h movement guidelines for children and youth 5-17 years4,23vs. those in early childhood (0-4 years),24especially because children and youth may rely more heavily on community structures and programs. Studies that included populations both within and outside of the 5-17-year age range were included at the full-text review if results were separated by age. Studies were included if the age range had some overlap(e.g.,4-6 years or 15-18 years)as long as the majority of the sample was aged 5-17 years.
2.1.2. Concept
All articles that examined movement behaviors(PA,sedentary behavior/screen time, and sleep) in populations 5-17 years of age within the context of the COVID-19 pandemic were included. The behaviors included all forms of PA and related concepts, such as physical fitness and outdoor play. All forms of screen time and sedentary behavior and all measures of sleep habits (e.g., duration, quality, sleep/wake schedule,disturbances)were included.
2.1.3. Context
For inclusion within this scoping review,papers must have been published in English within the period following the World Health Organization’s declaration of COVID-19 as a global pandemic. This included all papers published between the dates of March 11, 2020, and January 27, 2021. Included studies were not limited by country or geographic location.
2.1.4. Types of sources
This scoping review included all primary research studies and study designs,secondary data analyses,other systematic and scoping reviews, commentaries, editorials, and gray literature for the purposes of including preprints or ongoing trials and reports due to the real-time,evolving nature of the COVID-19 pandemic and the need for rapid circulation of timely evidence.
2.2. Search strategy
Initially, limited searches were conducted in Medline and SportDiscus databases.These limited,exploratory searches produced subject headings,key terms,and index terms.In consultation with institutional librarians, a comprehensive search strategy was developed for Medline(Ovid)and Embase(Ovid)using the identified terms and subject headings. These search strategies were then translated for additional databases to be used in conducting the full search. Two searches were conducted. The first search was conducted on November 25, 2020(limited to papers published March 11, 2020, or later), and the second was conducted on January 27, 2020 (limited to papers published on November 25,2020,or later).No papers published after January 27, 2021, were included in the final list. Finally,after performing a study selection for each database, the reference lists of all identified papers were manually searched for additional studies that fit the eligibility criteria.The full search strategies can be found in Supplementary File 1.
2.3. Information sources
Published articles and studies were extracted from Medline(Ovid), Embase (Ovid), Cumulative Index to Nursing and Allied Health Literature(EBSCO),SportDiscus(EBSCO),psychINFO(EBSCO),and Google Scholar.Searches for gray literature and unpublished papers were conducted manually through Google Scholar and Google custom search.
2.4. Study selection
Results were exported to Covidence Systematic Review Software Version 2.0 (Veritas Health Innovation, Melbourne,Australia) for de-duplication and screening. Two reviewers(DCP and KR) independently undertook the initial screening by title and abstract through blind voting based on inclusion eligibility criteria. Full-texts of included studies were then scrutinized for inclusion within the scoping review using custom-created exclusion reasons within the Covidence (Veritas Health Innovation).When a conflict arose in either stage,a discussion between reviewers was needed for resolution, and a third,adjudicating,vote by GF was required to move the citation forward if consensus was not reached.
2.5. Data extraction
Once screening was complete, included articles were processed for data extraction through the Covidence data extraction tool. Using Covidence (Veritas Health Innovation), the custom-created extraction form included all relevant details including the following: identification information (title, first author, date, country, and journal); participants (total number(male/female)), age range (mean); population description;methods (objective, article type, study design, measures, time period of measurement, before-COVID-19 comparison (yes/no)); and results (PA findings, sedentary behavior/screen time findings, and sleep findings). A complete template of the data extraction form can be found in Supplementary File 2. Data extraction was completed for all included articles by the primary reviewer (DCP). A second independent reviewer (KR)completed extractions for one-third (n=50) of the included articles. Once complete, the data gathered by each reviewer for the studies with 2 extractions were compared,and then the consensus data were exported.
2.6. Data charting and presentation
A basic numeric analysis was conducted to describe the characteristics of included studies, such as the number, geographic distribution, populations, and study designs. Next, a content analysis was undertaken to present thematically the findings of the included studies according to outcomes.Results were reported and discussed with respect to their implications for future research,practice,and policy.The results that follow focus on the studies reporting empirical data. The quality of the evidence and studies was not assessed because the objective of this scoping review was to map the nature of research being conducted.
3. Results
A total of 1486 articles were retrieved, 470 of which were removed through de-duplication, and another 786 of which were excluded for irrelevance through title and abstract screening.The remaining 230 articles were full-text reviewed,a process that resulted in the exclusion of an additional 80 articles(reasons are outlined in Fig. 1). The remaining 150 articles were included in this scoping review.
This review sought to map all available literature on the issue at hand, so all article types were included. The final list comprised 110 empirical research studies with 103 original data sets,6 reviews,and 34 commentaries and editorials(these are discussed separately in the Results section and were excluded from data charting).A total of 40 countries were represented in the studies, with China (n=23), the United States(n=10), multicountries (n=10), Canada (n=9), Italy (n=7),Spain (n=7), India (n=6), Australia (n=6), Turkey (n=6),Brazil (n=5), and Croatia (n=3) composing the majority; a complete breakdown is presented in Table 1. Although all included studies examined school-aged children,some specific populations were targeted: 91 articles examined typically developing, apparently healthy children, youth, or both,whereas 4 studies looked at youth athletes, and the remaining 16 included children and youth with specific medical conditions,as outlined in Table 1.
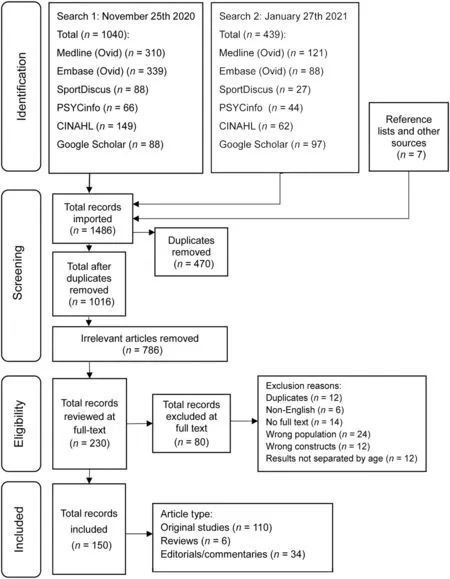
Fig.1. Flow chart of stages of article selection.CINAHL=Cumulative Index to Nursing and Allied Health Literature.TagedEnd
3.1. Editorials,commentaries,and perspectives
Nearly a quarter of the publications found were commentaries25-58in which authors speculated about likely pandemic-related health impacts, presented recommendations for policy makers and parents, or disseminated knowledge or promoted the value of practicing healthful movement behaviors during the COVID-19 pandemic (Supplementary File 3).Nine commentaries25-33discussed potential health impacts of the pandemic generally,including changes in PA,screen time,sleep, bedtime schedules, routines, environmental threats, and obesity risk, whereas four34-37focused in depth on screentime concerns with respect to children and youth during COVID-19-related restrictions. The specific eye and vision health concerns related to increased screen time were detailed,with 4 commentaries38-41focusing on myopia risk and another highlighting potential disruption of oculomotor development.42Five commentaries29,43-46took a stance to promote health within families by highlighting the importance of engaging in healthful movement behaviors43and achieving sufficient PA,29,44especially for those experiencing obesity45or autism spectrum disorder.46
An additional objective shared by many of the commentaries was to outline recommendations for mitigating the collateral health impacts of COVID-19.This included recommendations to governments, policymakers, and researchers47-50for mitigating unhealthful PA,screen time,and sleep trends and for sleep as an effective initiative for combatting the pandemic’s health effects.37,51Recommendations were also made to parents for managing their children’s behaviors34,43,52-54and mental health55and for guidance to media use for children with disabilities.56One commentary57discussed potential long-term implications of the pandemic on youth sport participation and suggested that the COVID-19 pandemic could be an opportunity to create more play spaces and low-cost opportunities for PA engagement by children and youth.
3.2. Reviews
Three systematic reviews,59-612 scoping reviews,62,63and 1 narrative review64were identified. Only 2 of these reviews(1 scoping62and 1 systematic59) focused on movement behaviors. The scoping review62examined only PA, whereas the systematic review59examined PA and sedentary behaviors;both included studies across the lifespan (Supplementary File 4).Both reviews concluded that PA frequency and duration decreased during the pandemic, whereas the systematic review also noted a rise in sedentary behavior.59Both reviews providednoncomprehensive inclusion of literature concerning the movement behavior of children and youth during COVID-19,and all relevant studies were included in the present scoping review. Two other systematic reviews that were published60,61investigated the effects of the pandemic on the lives of schoolchildren and on the psychological and behavioral effects of lockdown on children and youth. One review60included 3 commentary articles on healthy movement behaviors for children during lockdown, but original research relating to PA, sedentary behavior, or sleep was not included.The second review,61which concerned the psychological well-being and behavioral profiles of children,found that 21.3%of children in the included studies were suffering from sleep disturbances during the COVID-19 pandemic.62The final 2 reviews63,64did not include studies about the movement behaviors of children during COVID-19 but did review previous literature on movement behaviors of children in related contexts, such as vacation/weekends and instances of social isolation.Their findings suggested that PA,screen time,and sleep behaviors were likely to change during the pandemic.
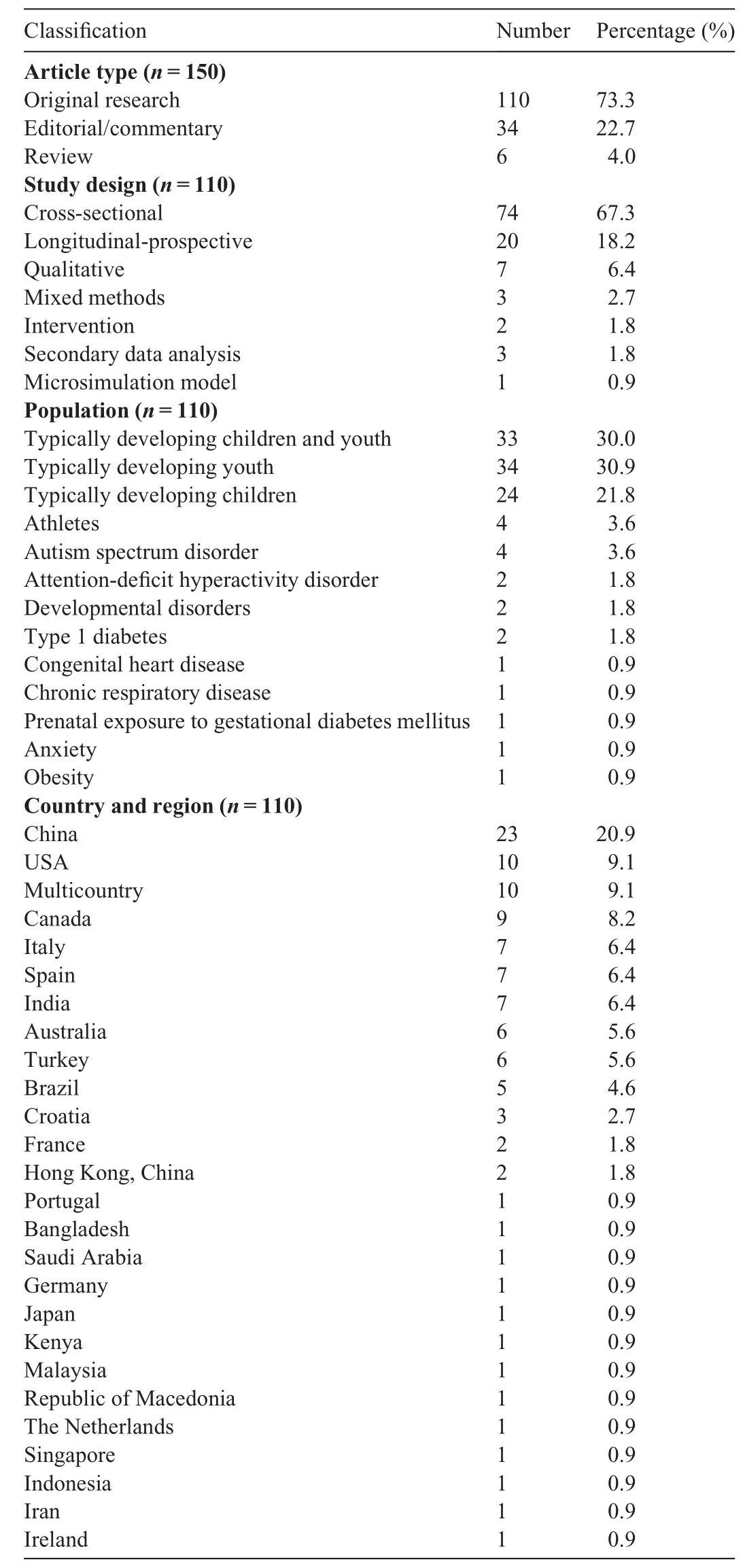
Table 1 Characteristics of included studies.
3.3. Original research
Of the 110 studies reporting original research, a total of 77(70.0%)examined PA,58(52.7%)looked at sedentary behavior or screen time,and 55(50.0%)investigated sleep behavior(Supplementary File 5). Of the studies, 28 measured all 3 movement behaviors, 28 measured 2 movement behaviors,and 50 examined only a single movement behavior. A visual breakdown of which movement behaviors were measured in each included study can be seen in Fig. 2. The majority(67.3%) deployed a cross-sectional design, whereas 20(18.2%) used a longitudinal approach, and 7 studies (6.4%)employed qualitative methods. The remaining study-design counts can be viewed in Table 1, and their organization by movement behaviors measured is available in Fig. 2. Another relevant classification of the included studies pertains to those that attempted to include some form of a comparison of movement behaviors between the time during the COVID-19 pandemic and the time before it. This aspect of the study design was instrumental in demonstrating changes in movement behaviors and, in turn, the effects of the pandemic on the behaviors of children and youth.Strategies employed to assess changes in movement behaviors included cross-sectional items in which participants reported an increase/decrease/no change;repeated cross-sectional designs;retrospective questions;and true longitudinal-prospective studies. Of the empirical studies, 72(65.4%) included a before/during COVID-19 comparison,whereas 38 (34.5%) included only a measure of movement behaviors during the pandemic.A visual breakdown of this attribute in relation to study design and movement behaviors can be seen in Fig.2.The majority of the original studies collected data in the spring of 2020, with most concluding their collection in March (n=14), April (n=25), or May (n=24). However, some studies began in February(n=6)or continued to collect into the summer,finishing in June(n=9),July(n=6),or August(n=2).No studies reported collecting data later than August 2020.
3.3.1. Physical activity
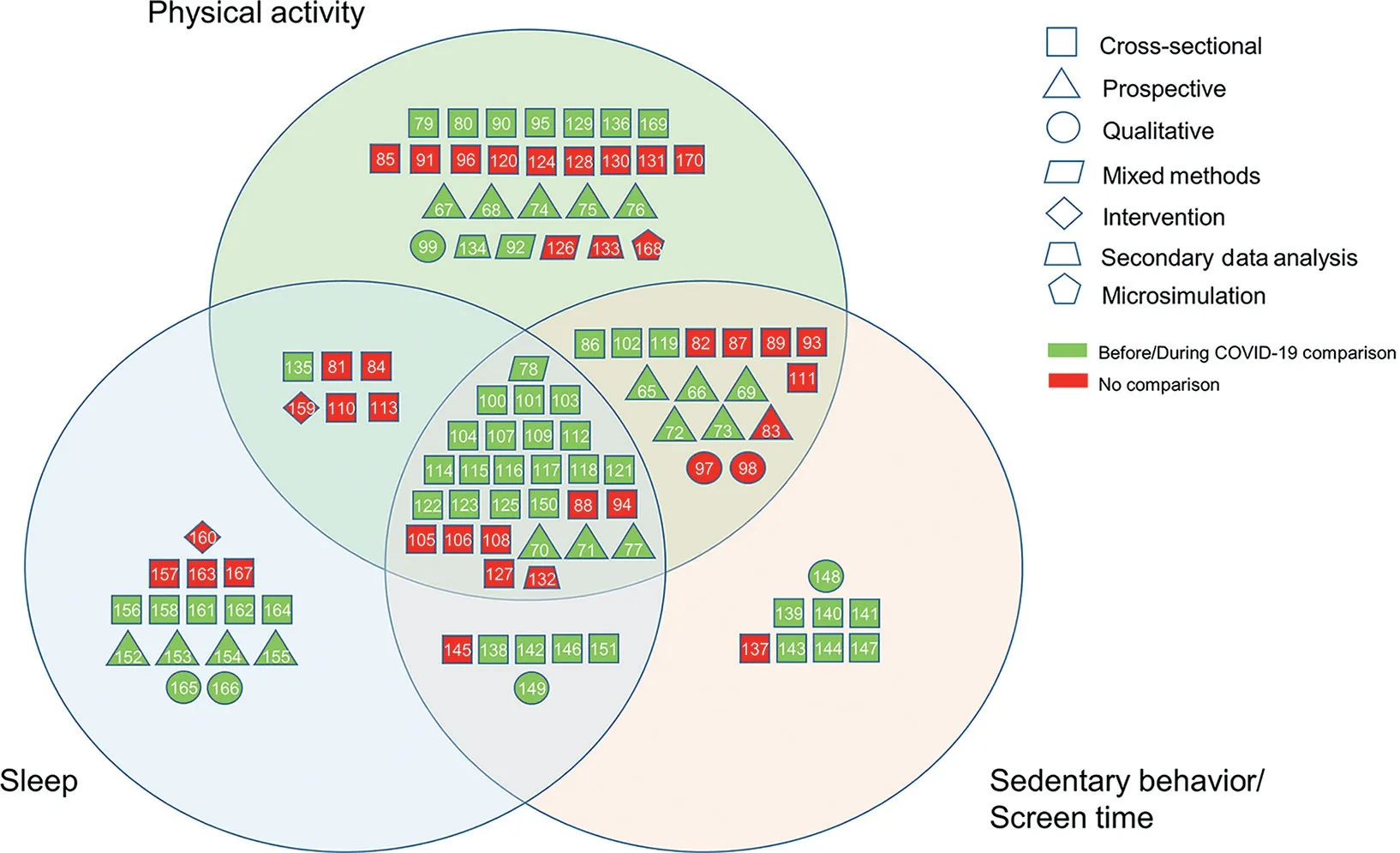
Fig.2. Movement behaviors and study designs of included studies.TagedEnd
A total of 77 original studies examined PA during the pandemic; 44 of them incorporated comparisons with prepandemic behaviors, although only 13 did so through a longitudinal design.65-773.3.1.1. Measures. Due to pandemic restrictions, it is unsurprising that online child/parent-reported questionnaires comprised the majority of PA measures. Of the studies, 37 used validated self-report measures of PA or related constructs,including the International Physical Activity Questionnaire(IPAQ),78-85PAQ-Adolescents,67,68,74,75Global-PAQ,69Godin Leisure Time Exercise questionnaire,86,8724-h PA recall,88,89Pediatric Functional Activity Brief Scale,90,91Youth Activity Profile Questionnaire,70ecological momentary assessments,66MoMo PA Questionnaire,65or other validated questionnaires.73,92Two studies designed and validated new questionnaires for children in lockdown,93,94and 3 studies used device-based measures of PA, including accelerometry73and pedometry.95,96Four studies used qualitative approaches,including interviews,97parent-to-child interviews,98open-ended questions,92and a case study.99The remaining studies relied on nonvalidated measures of PA through self-reported questionnaires constructed by the researchers.These questionnaires quantified PA behaviors using several approaches, including subjective reporting of changes,72,78,100-104daily duration of PA,105-116days per week with at least 60 min of MVPA,71,117-124or frequency of weekly PA,125weekly PA duration,76,77,118,126outdoor activity,78,116,119,127±3 h of PA per week,128,129percentage of time spent in PA,130,131or other means,as detailed in the list of included studies in Supplementary File 5.We identified 3 secondary data analyses.132-134
3.3.1.2. Associations with and impact of COVID-19-related restrictions. Results consistently showed reported decreases in PA time in children and youth, and this was demonstrated repeatedly in both longitudinal66-70,72-75,77and cross-sectional designs.78,80,84,92,102,103,107,109,114,117,118This result was echoed by those of other studies using similar constructs, including exercise time,100,104,115energy expenditure,79and MVPA.116,121-123However, 3 longitudinal research studies reported decreases in sportsrelated PA65,73,77but not in school and leisure-time PA,73habitual activity,65and nonorganized sports-related PA.65It is worth noting that although studies consistently identified overall decreases in PA,there were groups of children and youth in some studies who reported stability125or an increase65,132in unstructured PA.Several studies reported changes in the proportion of children and youth meeting PA guidelines. All reported decreases,66,73,107,109,117,121except for a German longitudinal study that reported an increase in the proportion meeting guidelines65(this appeared to be fueled by an increase in nonorganized sports-related PA and habitual activities).Declines in PA were also repeatedly reported in child/youth populations with medical conditions,including those with chronic heart disease,95Type 1 diabetes,76,129autism spectrum disorder,71prenatal exposure to gestational diabetes mellitus,89and other physical disabilities.135
Three studies73,95,96used device-based measures of PA,although only 2 included a comparison of PA levels.73,95Results from both studies were consistent with self- and proxy-report studies. Compared to before the pandemic, children with congenital heart defects spent less time in light PA and MVPA73and had reduced step counts.95
Regarding changes in the nature of PA during the pandemic,the general theme that emerged from the evidence was that PA shifted from occurring outdoors and in the community to being home based. Several studies reported declines in outdoor time and activity104,116,117,119and active transport,122whereas 2 noted a change of location to more in-home PA.72,119Only 2 studies72,92included a measure of participation in strengthening exercises,and neither assessed changes in this behavior.
Another qualitative study of youth participants in a sportsdevelopment program in Kenya reported that every participant commented on impacts to their fitness levels as well as declines in sport-specific skills due to lack of training.99A study of youth long-distance runners reported decreases in both frequency and distance of weekly running habits.136
3.3.1.3. Factors. At the individual level, several effects were noted regarding gender, age, and prepandemic behavior. Unsurprisingly,boys were engaged in more PA during COVID-19 than girls,on average,75,80,84,85,87,90,91,117,132although 2 cross-sectional studies130,131reported no differences in PA time between boys and girls,and a third study82reported more vigorous PA in boys but more light-to-moderate PA in girls. There were inconsistent findings related to which gender’s movement behaviors were most impacted by COVID-19 restrictions. Several studies reported larger reductions in PA time for girls during the pandemic,72,75whereas others reported similar decreases91or greater decreases in boys.67,74Not surprisingly, many studies, including 2 longitudinal designs,65,72reported greater decreases in PA time inolderchildren/youth.102Theyalsodetermined that younger children were more physically active during COVID-1987,117,130than were their older counterparts and found that grade differences were linked to differences in PA time.85,90Regarding individual behavior and fitness, greater PA92and fitness status67,74before lockdown were associated with higher PA levels during lockdown.Additionally,a study120found that youth who used digital platforms (e.g., streaming services, facilitated online classes,and subscribed fitness programs)to engage in PA during the pandemic were more likely to meet PA guidelines.
At the parental and family level, multiple constructs were associated with both children’s PA levels and pandemic-related changes. Parental support and coparticipation were correlated with greater PA and outdoor time.117Greater PA levels were reported for children and youth from 2-parent homes,105multichild homes,131,133higher-income households,84,133and homes with set routines and task schedules.105On the contrary, lower activity levels during COVID-19 were found in homes where all adults were working from home.131Greater PA decreases were also found in children of parents with high anxiety.119Findings on parental education levels were inconsistent and were associated with greater70or lesser80PA levels or,sometimes,were not shown to be correlated at all.133
Environmental factors were also found to play a role in PA levels and changes. Children and youth in homes with available outdoor spaces reported greater during-pandemic PA70,130,131and lower levels of decline70when compared to their activity before the pandemic.This was paralleled by findings showing greater PA in children living in homes as opposed to apartments.133Additionally, youth in urban areas showed larger decreases in PA,68a finding that aligned with another analysis demonstrating a negative association between outdoor activity and dwelling density and closeness to major roads,with the caveat that likelihood of outdoor time increases when children live within 1 km of a park.133In contrast, a study from China84reported rurality as a risk factor for physical inactivity. A secondary data analysis of regional differences in the outdoor play of Canadian children and youth noted that all regions saw declines in outdoor play; however, the provinces with the greatest declines had the most stringent outdoor restrictions, which also coincided with a greater number of reported COVID-19 cases.134
3.3.2. Sedentary behavior and screen time
Of the 110 empirical studies included in this review,58 examined sedentary behavior/screen time,and 42 of those incorporated a comparison with prepandemic levels. Of the 42 comparison studies, 8 used a longitudinal design65,66,69-73,77to measure screen time/sedentary behavior changes.
3.3.2.1. Measures. Sedentary behavior was most commonly measured through researcher-constructed questionnaires that reported duration of screen time longitudinally69,71,73,77and crosssectionally,78,89,105,107,109,112,115,118,119,122,123,127,137-141although several studies more broadly recorded duration of sedentary/sitting time.69,83,88,89,122-125Screen-time duration was often broken down by device119,121or media usage, including internet or social media86,108,117,142,143and gaming,144,145as well as by purpose,whether for online study73,87,106,112,137or leisure use.65,69,103,111,115A large number of studies simply reported subjective changes of screen time or sedentary behavior.72,78,84,100,101,103,114,117,119,141,146Six studies implemented validated questionnaires that included sedentary behavior/screen time items,66,70,93,94,104,147and 4 studies97,98,148,149used qualitative approaches,including semistructured interviews,97,148focus groups,149and parent-to-child interviews.983.3.2.2. Associations with and impact of COVID-19-related restrictions. Significant increases in screen time compared to prepandemic levels were reported nearly unanimously through longitudinal,69,70,71,77cross-sectional,78,101-104,107,109,116-119,121-123,138-140,147,150and qualitative148designs. At a broader level,increases in general sedentary behavior time were a consistent finding,66,72,73,119,122,123,146although a cross-sectional report actually noted a decrease in overall sitting time despite rises in screen time.125Screen time, when classified by purpose, demonstrated increases in both academic-related use time73,112and leisure-time usage.65,69,115Increases were reported for both weekday73,112and weekend screen time,86,150although a Dutch longitudinal study reported no increases in weekend screen time compared with prepandemic levels.73Regarding more specific device and media usage, children and youth were reported to have developed longer durations of cell phone,114,142computer,114,119,125gaming104,119and online gaming,144TV and digital media,100,104,114,117,119,125,141socialmedia,66,86,104,117and internet66,142,143,151usage. A few studies considered screen-time guidelines,and all reported an overall increase in the proportion of children exceeding these guidelines.117,121Both weekend and weekday screen time increased in a sample of youth with autism spectrum disorder,71a finding supported qualitatively by parents’perceptions that the pandemic had made it more difficult to limit screen time.97Overall screen time also rose in children and youth with prenatal exposure to gestational diabetes mellitus.89
A further possible effect of the conditions imposed on families by the pandemic was a change in the degree of parental mediation of device usage by children and youth. This was examined by a cross-sectional study,137which reported high usage of electronic devices without any parental mediation;however,this was not compared with prepandemic behaviors.
3.3.2.3. Factors. Several factors moderated differences in sedentary behavior/screen time during the pandemic at the level of the individual.Screen time and sedentary behavior were generally found to increase with age,with older age brackets of children and youth repeatedly presenting larger daily and weekly durations of screen usage82,87,103,105,140than their younger counterparts as well as greater increases from prepandemic levels.72,112,117,118Gender differences were also noted,with several accounts of greater sedentary time,123screen-time,82,87,123and increases in social media usage117by girls,although 2 studies103,105reported greater screen time use by boys.
Several parenting and family attributes were associated with screen time during the COVID-19 pandemic.Two-parent families105and families with set routines and task schedules105reported lower levels of screen usage by children.Meanwhile,families where parents displayed irritable behaviors,116aggressive/accusatory problem-solving tactics, or over-reactive and inconsistent parenting practices140were more likely to report higher levels of screen time among children. Interactive parenting practices (parent-child activities) were negatively associated with screen time.140Children and youth of parents under 43 years of age and of those who reported a high capability to restrict screen time were the most likely to adhere to screen-time guidelines.132Finally, significantly greater increases in screen time from prepandemic levels were reported in children and youth who had TVs in the bedroom.70
Although academic screen time/online study were not commonly measured in the literature, a pair of qualitative/mixed-method studies reported that parents commented that online study demands were the primary reason for increased screen time.78,148Still, significant leisure usage increases were also reported in other studies.65,69,115
3.3.3. Sleep
Of the studies, 55 included measurements of the sleep habits of children and youth,and 38 of those studies compared the habits to pre-COVID-19 sleep habits. Sleep comparisons were made using longitudinal data in 7 studies.70,71,77,152-155
3.3.3.1. Measures. Seventeen studies78,81,83,84,104,116,138,145,156-159,160-164tested varying measures of sleep through validated questionnaires,including the Pittsburgh Sleep Quality Index,78,156-159Sleep Disturbance Scale for Children,116,160,161Children’s Sleep Habits Questionnaire,162-164Youth Self-Rating Insomnia Scale,81,83,84Insomnia Severity Index,145Epworth Daytime Sleepiness Scale,138and the broader Coronavirus Health Impact Survey.104Four studies were qualitative and included semistructured interviews148,165,166and focus groups.149The majority of sleep studies implemented researcher-constructed questionnaires that targeted several sleep constructs,includingdailydurationof sleep,77,105-107,109,110,112,113,115,118,122-125,127,152-154bed/wake times,70,71,152-155and subjective sleep quality.152Additionally,many questionnaires simply asked participants about subjective changes in sleep time,78,100,101,103,117,151quality,117or the presence of sleep problems/disturbances.141,146,150,167
3.3.3.2. Impact of COVID-19-related restrictions. The impact of the pandemic on sleep appears to be more variable than its impact on PA or sedentary behavior. Sleep duration was the most widely studied measure of sleep.An increase(of variable amounts)in the sleep duration of children103,151and youth,125or both,70,77,109,115,117,118,121was the most common relevant finding in the included studies. Two articles78,162reported no overall changes in sleep duration. In 1 study,162the lack of change was attributed to an increase in nocturnal sleep along with a decrease in naps.A longitudinal study152of young children reported an initial decrease in sleep duration during the early weeks of lockdown,but the duration later stabilized.Several studies indicated that weekday sleep duration, in particular,showed significant increases,70,107,122,153whereas weekend sleepdurationexhibitedeitherlessconsistent increases70,122,123or comparable levels.153A cross-sectional study154suggested that the prepandemic differences in sleep duration between weekdays and weekends disappeared during the pandemic. This finding was supported by another cross-sectional study81in China that reported decreases in sleep debt and social jetlag; however, simultaneous increases in sleep latency(time of transition from wakefulness to sleeping) and inertia (time of transition from sleep to wakefulness)were also reported.81There was inconsistency with regard to changes in the proportion of children meeting sleep guidelines,with 2 studies104,121finding that more children were meeting guidelines,and another116suggesting the opposite.
Studies that measured timing of bedtime/wake-up were generally in agreement, showing later sleep schedules, with shifts to both later bedtimes and waking times. This finding was demonstrated in both children100,156,162,166and youth151,154,155,165for both weekends and weekdays.156,162
Sleep quality was also frequently assessed.Most commonly reported were negative effects, including decreases in sleep quality in both children and youth,100,101,116or an initial decrease followed by a stabilization,152along with an increase in the prevalence of sleep problems.150However, these findings conflict with qualitative results reporting improved youth sleep quality165and a lower prevalence of sleep disturbance in young children during the pandemic.162
Similar findings were reported in youth populations with diagnosed medical conditions.Children with autism spectrum disorder displayed shifts to later sleep schedules,164increases in sleep problems and disturbance164as well as sleep latency, and significant decreases in duration158(although another study71reported no changes in duration).A sample of children with chronic respiratory diseases displayed deteriorated sleep habits,114and a study of a sample of children with attention deficit hyperactive disorder found that children with later sleep schedules had more traumatic perceptions of the pandemic,perceptions that were themselves thought to be associated with sleep problems.163
Two studies159,160implemented interventions for improving sleep quality during COVID-19. The first deployed an aerobic exercise and peer education intervention for youth and found that sleep quality scores improved in both the intervention and control groups, including greater effects on the intervention group.159A second intervention study tested the effects of a home-based music therapy program on the sleep disturbance and parental stress of children with developmental disorders.160From before treatment to after treatment, significant improvements in sleep disturbance scores were recorded.1603.3.3.3. Factors. The results of the studies indicate greater impacts on the sleep habits of girls compared to boys.Parents reported that girls spent more time sleeping105,117and had greater increases in duration from prepandemic levels,123and girls were more likely to report decreases in sleep quality.101A higher prevalence of insomnia symptoms was also seen in girls,79,84,157symptoms that were even more prevalent among students in cities as compared to those in rural areas.157Greater fear of COVID-19 was associated with greater odds of developing insomnia symptoms,81whereas COVID-19 optimism and social support provided protection against insomnia.157Insomnia was also influenced by sitting time83and degree of internet gaming disorder.145Parents appeared to be influential as well as children with irritable parents generally achieved less sleep and had lower sleep quality.116Lower sleep quality was also associated with children whose mothers showed difficulty regulating emotions.156Longer sleep durations were reported for children and youth in families that did not have set routines and task schedules.105In a nationally representative sample of Canadian families,the group best adhering to sleep guidelines for children were those households with greater than CAD 100,000 yearly income who showed increases in sleep duration during COVID-19.132
3.3.4. Movement behaviors and mental health during COVID-19
Given the potentially stressful nature of the conditions imposed by COVID-19 on children and youth, and the pre-existing body of evidence associating movement behaviors and mental health,many studies that measured the PA,screen time, and sleep habits of children/youth during the pandemic were interested in examining their relationships with mental health outcomes. Greater PA levels during lockdown were found to be correlated with reduced risk of depressive symptoms,83,102,113anxiety symptoms,88,89insomnia symptoms,83or all three.81Furthermore, children engaging in greater PA levels were less likely to exhibit hyperactivity-inattention and more likely to display prosocial behaviors.124PA was positively associated with mood,85,87physical,social,and academic self-concept,128,168and changes in subjective well-being during the COVID-19 pandemic.169
Greater levels of screen time during lockdown were adversely associated with symptoms of depression83,108and anxiety,108although a cross-sectional study88found no association between screen time and state anxiety. Nonacademic screen time showed a negative association with mood.87
Sleep problems of children and youth during the pandemic predicted depressive, anxiety, and irritability symptoms.150Sleep durations longer than 8 h were associated with a reduced risk of anxiety,110whereas durations shorter than 6 h were significantly associated with onset of depression.110,113Other psychological difficulties, such as hyperactivity and emotional symptoms,were predicted by changes in sleep quality.156Children who achieved earlier bedtimes and longer sleep durations had fewer psychosocial problems,112whereas those with shorter sleep durations and late-to-rise patterns had higher odds of mental illness during the pandemic.153
3.3.5. Movement behaviors and other health outcomes during the pandemic
A micro-simulation model study was conducted to project the impact of COVID-19 on the prevalence of childhood obesity in the United States.170Hypothetical school-closure scenarios with a 10% reduction in PA were associated by the model with increased prevalence of obesity and higher mean body mass index z scores.170
Two studies171,172examined the role of the pandemic in declining physical fitness outcomes.A longitudinal study171of French youth elite soccer players reported decreases in aerobic capacity despite the provision of a home training program. A matched-cohort study172of 10 participants reported lower aerobic power scores in all but 1 participant during COVID-19 compared to a group of 10 matched participants measured before COVID-19.
A pair of large-scale studies conducted in China were concerned with the progression of myopia in school-aged children during the pandemic, given increases in screen time and reduced outdoor activity. These studies found significant increases in the prevalence of myopia in children aged 6-8 years173and of myopia progression in primary school children(Grades 1-6).174However,these effects were not found in youth.
As part of a cross-sectional study96examining the impact of social isolation on immune function,researchers used pedometers to classify children as active or sedentary during the pandemic and then compared the groups’ levels of plasma adipokine and lymphocyte cytokine concentrations.The study found that reduced PA during the pandemic may impair the functioning of the immune system and increase vulnerability to inflammatory diseases.96
4. Discussion
This scoping review is the first to present a comprehensive overview of the literature related to healthy movement behaviors—namely, PA, sedentary behavior, and sleep—in children and youth in the context of the first year of the COVID-19 pandemic. The results are not only consistent with initial reports,which pointed to declines in PA alongside increases in sedentary behavior,14,15but they extend our knowledge of the nature of changes in movement behaviors and of the factors contributing to differential impacts. This scoping review is the first to integrate findings related to the pandemic’s impact on sleep behavior.Consistent declines in PA time were observed alongside reductions in outdoor activity and shifts to in-home activity.Sedentary behavior and screen time consistently exhibited large increases across all forms of digital device usage,genders,and ages.Given the significant increases and daily screen times far in excess of guidelines,65,69,71,77,118,122,143along with evidence of an increased prevalence of myopia,173,174this is a particularly concerning finding.Declines in PA and increases in sedentary behavior were both greater among older children and youth.The consistency of results demonstrating reductions in PA and increases in screen time are of considerable concern.Sleep behavior was impacted more variably,seeing shifts to later bed and waking times and both positive and negative changes to sleep duration,sleep quality,and disturbances described.Last,child and youth engagement in healthy movement behaviors was found to be correlated with a range of positive mental health outcomes during the pandemic,further emphasizing the importance of targeted movement behaviors as a health-promotion strategy during the COVID-19 pandemic.
Given the already concerning prepandemic surveillance data on the proportion of children and youth failing to meet movementbehavior guidelines,these results present alarming insight as to current behavior trends and, thus, the potential prevalence of associated health risks. While a quality appraisal of the evidence is beyond the scope of this review,it is worth noting that more than two-thirds(67.9%)of the empirical studies implemented cross-sectional designs with overwhelming use of online self- or proxyreported questionnaires. Relying on this design during a global pandemic is certainly understandable and probably necessary,but it nevertheless highlights the need for caution when interpreting the results, given that conclusions surrounding pandemic impacts were often based on cross-sectional comparisons and parent recall through both validated and nonvalidated measures of PA, screen time, and sleep. There was a high degree of heterogeneity in the use of measurement instruments and items for recording movement behaviors, which may limit the feasibility of conducting meta-analyses.
4.1. Research gaps
Although 20 longitudinal studies were found and included,it is relevant that nearly all of these studies that implemented follow-up tests to compare with prepandemic scores did so in the early phases of lockdown, between March and June 2020.There is a gap in understanding longer-term changes in movement behaviors and a need for further, long-term longitudinal data to describe not just the change from prepandemic to during-pandemic behaviors, but also how behaviors have changed during and,eventually,after the pandemic.
The absence of intervention studies points to a clear gap in the research. Only 2 studies159,160attempted to implement interventions, and both targeted improving sleep quality. It is evident that there has been a widespread prevalence of physical inactivity and sedentary behavior across child and youth populations. Because of the long-term, ongoing nature of the pandemic, it is important that researchers, policy makers, and practitioners work to develop feasible interventions to support healthy movement behaviors, to support families, and to mitigate associated health risks,specifically with respect to screen time and PA. A range of family and environmental factors associated with movement behaviors during the pandemic were reported. Most common were parental practices, dwelling type,household income,family composition,parent working conditions, and the neighborhood built environment. The availability of data associating movement behaviors of children and youth with parental/family factors and practices suggests that this could be a potentially fruitful avenue for behavioral change. Qualitative data can provide detailed accounts of families’ experiences of lockdown restrictions,which would supplement the abundance of descriptive quantitative data and present an opportunity for new theories and inquiry to emerge in what is still a new research area. Further contextual research into families’ experiences and what parents want and need to support their children confidently and sustainably as they learn to engage in a healthy balance of movement behaviors is needed. It remains to be seen whether the “new normal” will be characterized by a child and youth movement behavior profile consisting of greater screen time and lower PA as compared to their prepandemic levels.
Overall declines in PA were reported,but there were longitudinal reports of increases in leisure-time PA,73unstructured sports, and habitual activities.65Other studies indicated within-sample groups of children who increased their PA and outdoor time.119,133These findings suggest the resilience and adaptation of some families during the pandemic,and that the impact of the pandemic has not necessarily been uniform for all children and youth. There is a gap in understanding these differences, and future research should strive to ground itself more strongly in a theoretical understanding of such distinctions in movement behaviors in general. Furthermore, despite clear recommendations for engaging in muscle and bonestrengthening activities among school-aged children and youth,4,23no included studies assessed changes in participation in these types of activities during the pandemic.
There were 2 potential moderators of change that warrant further attention.Changes in PA and screen time were consistently greater among youth as compared to children.PA differences in the literature were attributed to greater time in unstructured and free play in younger children,72,73which may be a developmental preference.175Greater screen time among older children may be due to increased educational demands,considering several studies reported longer periods of online study in older age groups.82,87,137However, increased recreational screen time was also found repeatedly in older age groups, which could be attributable to their greater access to personal devices and media or to less parental regulation.There was also some indication that the negative impact of the pandemic has been greater for girls than boys and has possibly exacerbated the gender disparity in movement behaviors(particularly sedentary/screen time and PA) that already existed among children and youth pre-pandemic,176,177which may be due, in part, to the influence of cultural and family factors.These findings suggest the need for interventions that are gender-sensitive and tailored to various age groups.
4.2. Strength and limitations
To our knowledge,this scoping review is the first to examine all movement behaviors of children and youth within the context of the COVID-19 pandemic.Because this review included all article types and relevant literature, it provides a comprehensive list,including articles related to PA, sedentary behavior/screen time,and sleep in children and youth.This study provides the most current compilation of available research, up to January 27, 2021.This scoping review did not appraise the quality of the evidence it included and must acknowledge the inclusion of preprints as well as some articles lacking peer review. Although findings were remarkably consistent, the extent of physical restrictions were likely to have varied widely,depending on the periods of data collection within the included studies,and this was not accounted for.
5. Conclusion
Globally,pandemic restrictions related to limiting the transmission of COVID-19 have had widespread impacts on the PA,sedentary behaviors,screen time,and sleep of school-aged children and youth. The frequency and duration of PA and outdoor activity have declined, while school-based and recreational use of digital screens has risen significantly across all devices and media.Sleep habits have also been affected, with later bed/wake times and changes in duration,quality,and prevalence of disturbances.There has been an overabundance of cross-sectional measures relying on parent and child recall to form interpretations of the pandemic’s impact. The body of longitudinal research thus far has been focused on a comparison of prepandemic behavior with behaviors during the earliest phases of lockdown,suggesting the need for further longitudinal designs to follow children and youth long-term to understand how movement behaviors change during the pandemic and as restrictions fluctuate.Researchers,policy makers,and practitioners must develop and test strategies for intervening on these behavior changes and mitigating the health risks associated with adverse changes to movement behaviors during the pandemic.Such strategies may need to be tailored based on gender and age.Finally, when developing and implementing restrictive measures,policy makers must consider the indirect, potentially long-term health consequences for children and youth.
Authors’contributions
DCP executed search strategies and carried out screening, full text reviews,data extraction,analysis,and the writing of the initial manuscript; KR performed screening, full text review, and data extraction; SAM conceived the research question, supervised searching and screening,and provided drafting and editorial assistance on the manuscript; NR provided drafting assistance; MST conceived the research question and provided drafting and editorial assistance on the manuscript;GF conceived the research question,supervised screening, reviewing, extraction, and analysis, and assisted in drafting the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.07.001.
 Journal of Sport and Health Science2021年6期
Journal of Sport and Health Science2021年6期
- Journal of Sport and Health Science的其它文章
- The association of grip strength with cardiovascular diseases and all-cause mortality in people with hypertension:Findings from the Prospective Urban Rural Epidemiology China Study
- Cardiorespiratory fitness measured with cardiopulmonary exercise testing and mortality in patients with cardiovascular disease:A systematic review and meta-analysis
- The relationships between step count and all-cause mortality and cardiovascular events:A dose-response meta-analysis
- IGF1-PI3K-induced physiological cardiac hypertrophy:Implications for new heart failure therapies,biomarkers,and predicting cardiotoxicity
- The epigenetic landscape of exercise in cardiac health and disease
- No independent associations between physical activity and clinical outcomes among hospitalized patients with moderate to severe COVID-19
