右美托咪定不同时间给药在小儿斜视矫正术中的应用
刘晶莹 苏小虎 吴磊 田宇峰 吴浩

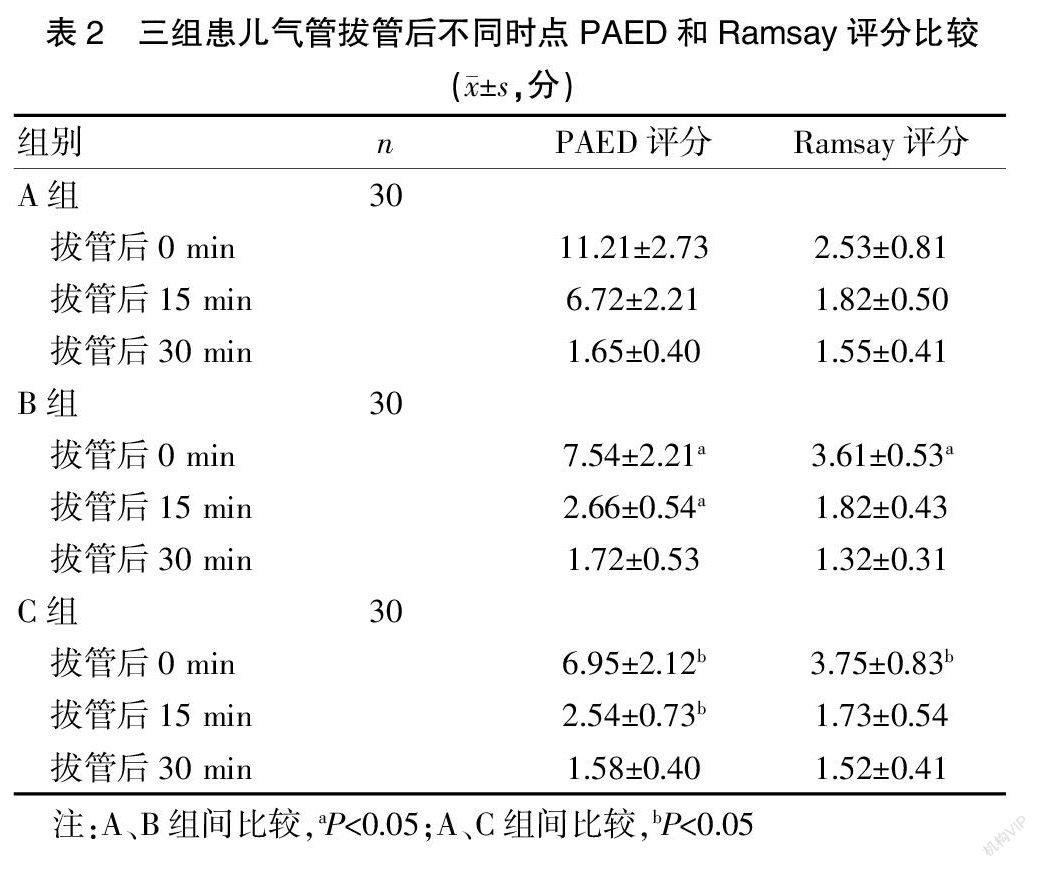

[摘要] 目的 探讨右美托咪定不同时間给药对患儿术后躁动、眼心反射及恶心呕吐发生率的影响。 方法 选取2017年5月至2020年7月我院斜视手术的患儿90例,按照随机数字表法将患儿分为A组、B组和C组,每组各30例,A组给予的5 mL 0.9%氯化钠注射液。B组在麻醉诱导时给予右美托咪定0.5 μg/kg(10 min泵注完毕),C组手术结束眼肌操作后给予右美托咪定0.5 μg/kg(10 min泵注完毕),记录三组患儿手术时间、拔管时间、麻醉后恢复室(PACU)停留时间,对比三组患儿拔管后0、15、30 min躁动评分(PAED)、Ramsay镇静评分、眼心反射发生率、恶心呕吐的发生率和右美托咪定补救次数。 结果 三组患儿性别、年龄、体重和手术时间比较,差异无统计学意义(P>0.05)。C组拔管时间(15.55±3.34)min、PACU停留时间(43.25±10.86)min,长于A组(9.07±2.21)min、(31.27±8.43)min和B组(9.38±2.54)min、(32.43±7.36)min,差异有统计学意义(P<0.05)。A组拔管后0 min PAED评分为(11.21±2.73)分、15 min(6.72±2.21)分,高于B组(7.54±2.21)分、(2.66±0.54)分和C组(6.95±2.12)分、(2.54±0.73)分,差异有统计学意义(P<0.05)。B组拔管后0 min Ramsay镇静评分为(3.61±0.53)分,C组拔管后0 min Ramsay镇静评分为(3.75±0.83)分,均高于A组的(2.53±0.81)分,差异有统计学意义(P<0.05)。B组眼心反射发生率为80.00%,明显高于A组(56.67%)和C组(60.00%),差异有统计学意义(P<0.05)。A组恶心呕吐发生率为66.67%,明显高于B组(33.33%)和C组(43.33%),差异有统计学意义(P<0.05)。A组右美托咪定补救次数(18例)明显高于B组(3例)和C组(0例),差异有统计学意义(P<0.05)。 结论 小儿斜视手术在眼肌操作结束后应用单剂量的右美托咪定可降低术后躁动的发生率,而不增加眼心反射的发生。
[关键词] 斜视手术;右美托咪定;术后躁动;眼心反射
[中图分类号] R614 [文献标识码] B [文章编号] 1673-9701(2021)24-0145-04
Application of dexmedetomidine administered at different times in pediatric strabismus surgery
LIU Jingying SU Xiaohu WU Lei TIAN Yufeng WU Hao
Department of Anesthesiology, Suqian First People′s Hospital Affiliated to Nanjing Medical University, Suqian 223800, China
[Abstract] Objective To explore the effects of dexmedetomidine administered at different times on the incidence of postoperative agitation, oculocardiac reflex and nausea and vomiting in children. Methods A total of 90 children who underwent strabismus surgery in our hospital from May 2017 to July 2020 were evenly divided into group A, B and C(n=30) by using the random number table method. Group A was given 5 mL of 0.9% sodium chloride injection, group B was given dexmedetomidine 0.5 μg/kg at the induction of anesthesia (with a pumping completion time of 10 min), and group C was given dexmedetomidine 0.5 μg/kg (with a pumping completion time of 10 min) at the end of surgery after eye muscle operation. The of three groups time of surgery, time of extubation, and length of stay in the postanesthesia care unit (PACU) were recorded. The agitation scores at 0, 15 and 30 min after extubation PAED, Ramsay sedation score, incidence of oculocardiac reflex, incidence of nausea and vomiting, and number of dexmedetomidine remedies of three groups were compared. Results There were no statistically significant differences in gender ratio, age, weight and surgery time among the three groups(P>0.05).The time of extubation (15.55±3.34)min and length of stay in PACU (43.25±10.86)min in group C were longer than those in group A (9.07±2.21) min, (31.27±8.43) min and group B (9.38±2.54) min, (32.43±7.36) min,with statistically significant differences (P<0.05). The PAED scores at 0 min (11.21±2.73)points and 15 min (6.72±2.21) points after extubation in group A were higher than those in group B (7.54±2.21)points, (2.66±0.54) points and group C(6.95±2.12)points, (2.54±0.73) points, with statistically significant differences(P<0.05). The Ramsay sedation score at 0 min after extubation in group B (3.61±0.53) points and group C (3.75±0.83) points were higher than that in group A (2.53±0.81) points, with statistically significant difference(P<0.05). The incidence of oculocardiac reflex in group B was 80.00%, which was significantly higher than that in group A (56.67%) and C (60.00%), with statistically significant difference(P<0.05).The incidence of nausea and vomiting in group A was 66.67%, which was significantly higher than those in group B(33.33%) and group C(43.33%), with statistically significant difference (P<0.05). The number of dexmedetomidine remedies in group A was 18 cases, which was significantly higher than that in group B (n=3) and group C(n=0), with statistically significant difference(P<0.05). Conclusion The application of a single dose of dexmedetomidine at the end of eye muscle operation in pediatric strabismus surgery can reduce the incidence of postoperative agitation without increasing the incidence of oculocardiac reflexes.