Research advances concerning the mechanism of glucocorticoid resistance in relation to traditional Chinese medicine for patients with chronic obstructive pulmonary disease
Wei Yu,Peng-Cheng Zhou
1Clinical Medical School, Chengdu University of Traditional Chinese Medicine, Chengdu 610072, China.2Department of Respiratory Medicine, Hospital of Chengdu University of Traditional Chinese Medicine,Chengdu 610072,China.
Abstract Chronic obstructive pulmonary disease is a common, highly disabling, and burdensome disease.Anti-inflammatory glucocorticoid medication plays a key role in its treatment; however,glucocorticoid resistance in patients with chronic obstructive pulmonary disease considerably weakens the effects of the treatment.Despite recent advances in determining the mechanism of glucocorticoid resistance in patients with chronic obstructive pulmonary disease, the role of traditional Chinese medicine in treating such patients remains unclear.In this review, we reviewed the mechanism of chronic obstructive pulmonary disease-related glucocorticoid resistance with reference to the glucocorticoid receptor, the important signaling pathways(phosphatidylinositol-3-kinase/protein kinase B signaling pathway, p38 mitogen-activated protein kinase signaling pathway, and interferon-γ/Janus kinase/stransducer and activator of transcription signaling pathway), histone deacetylase, nuclear transcription factor-κB,exosomes,and microRNA.Moreover, the methods of establishing the glucocorticoid resistance model associated with chronic obstructive pulmonary disease and advances in therapeutic approaches including traditional Chinese medicine to restore chronic obstructive pulmonary disease glucocorticoid sensitivity have also been reviewed.This review shows that traditional Chinese medicine reverses glucocorticoid resistance mainly by regulating the expression of glucocorticoid receptor, p38 mitogen-activated protein kinase signaling, histone deacetylase 2,and nuclear transcription factor-κB in chronic obstructive pulmonary disease models.Future research is suggested to evaluate traditional Chinese medicine understanding of chronic obstructive pulmonary disease-related glucocorticoid resistance in relation to exosomes,microRNA, and other signaling pathways.
Keywords: chronic obstructive pulmonary disease; glucocorticoid resistance; traditional Chinese medicine; glucocorticoid receptor; PI3K/AKT signaling pathway; exosome
Tradition
Traditional Chinese medicine,which has a long history,is widely used in the treatment of respiratory diseases.Licorice,as one of the most representative commonly used Chinese herbal medicine with anti-inflammatory properties,was first recorded in theCode of Hammurabi(the earliest code in the world written around 2100 B.C.E.).Shennong’s Herbal Classic of Materia Medica,China’s earliest pharmacological book(written between about 200 and 250 C.E.,the Eastern Han Dynasty of China),categorized licorice as a top-grade medicine and recorded its various effects.In 652 C.E.,Sun Simiao,a famous physician of the Tang Dynasty of China,used licorice to treat pulmonary fibrosis,which was fully described in his book,Essential Formulas for Emergencies Worth a Thousand Pieces of Gold.With the development of modern medicine,licorice was widely used to treat several types of lung diseases,such as chronic bronchitis,asthma,chronic obstructive pulmonary disease,tuberculosis,etc.In 2013,Kao demonstrated that licorice could restore glucocorticoid sensitivity by depleting reactive oxygen species through heme oxygenase-1 expression,decreasing the phosphorylation of p38 mitogen-activated protein kinase,and preventing the phosphorylation of the glucocorticoid receptor at Ser211.Nowadays,licorice is one of the pharmacopeia drugs of China,which is approved to treat various respiratory disorders.
Background
Chronic obstructive pulmonary disease (COPD), a preventable,therapeutic disease and one of the most common diseases of the airway system, is characterized by persistent respiratory symptoms and airflow limitation resulting from abnormal airways and/or alveoli due to toxic particles or gases [1].Globally, the burden of the disease is heavy, and disease prevention and control remain challenging.The World Health Organization has predicted that by 2020, this disease will be the third leading cause of death and the fifth leading cause of disease worldwide [1].In 2018, an epidemiological COPD survey undertaken in China showed that the prevalence of COPD among Chinese individuals aged 40 years and above was as high as 13.7%,indicating that nearly 100 million people had COPD in China [2].This survey found that the annual direct costs for patients with COPD in China accounted for approximately 40% of family income and the per capita economic burden of disease amounted to 20,107.58 Yuan, with between 24.4% and 24.8% of patients with COPD at high risk of being financially challenged [3, 4].In patients with COPD, the occurrence of acute exacerbations has been reported to range between 0.5% and 3.5%annually,and this is a significant cause of death in these patients.More than 3 million people worldwide die each year from COPD, and 6% of all-cause mortality is due to COPD [5].In 2013, COPD-related deaths in China amounted to approximately 910,000, with COPD ranking third in the single disease category, and COPD accounted for 11% of all-cause mortality in China and 31.1% of COPD deaths globally [6].
COPD is a chronic inflammatory respiratory disease, and anti-inflammatory medication plays a central role in its treatment.Glucocorticoids are powerful anti-inflammatory drugs; however,glucocorticoid resistance can determine treatment success or failure,and this remains an ongoing challenge for patients with COPD.Unlike asthma, COPD airway inflammation predominately involves neutrophil and macrophage infiltration, and eosinophils are rare,which diminish anti-inflammatory effects or induce glucocorticoid resistance.The degree of glucocorticoid resistance found in different stages of COPD has been reported to be inconsistent and closely related to lung function.The lower the forced expiratory volume in 1 second/forced vital capacity ratio, the more serious the glucocorticoid resistance is likely to be [7].Uncontrolled airway inflammation can recur and progress.Frequent acute exacerbations accelerate lung function decline, worsen clinical symptoms and quality of life, and increase the risk of disability and death.Moreover, acute exacerbations also result in a considerable social and economic burden in relation to family expenditure and medical insurance costs.While the severity and challenges of glucocorticoid resistance for patients with COPD have previously been reported, the mechanism of glucocorticoid resistance in COPD is unclear, and effective treatment medications currently remain limited.
Traditional Chinese medicine (TCM) is widely used in the treatment of COPD.Many studies have shown that it not only has an anti-inflammatory effect, but also reduces the side effects caused by glucocorticoids, such as osteoporosis [8–10] and abnormal fat metabolism [11].The reported mechanism of action is the glucocorticoid receptors(GR) binding activity of part of a TCM or herb extract which can induce GR nuclear translocation, but does not induce glucocorticoid response element (GRE)-driven gene expression and preadipocyte differentiation [11].For example, licorice, one of the most representative commonly used Chinese herbal medicine with anti-inflammatory properties, was first recorded in theCode of Hammurabi(the earliest code in the world written around 2100 B.C.E.)[12].Hippocrates (400 B.C.E.) recommended licorice for injuries and inflammation [13].Shennong’s Herbal Classic of Materia Medica, China earliest pharmacological book (written between about 200 and 250 C.E., the Eastern Han Dynasty of China), categaried licorice as the top-grade medicine and recorded its various effects [14].Around 200 to 210 C.E., Zhang Zhongjing, a famous physician of the Eastern Han Dynasty of China, used licorice to treat pulmonary abscess, which was recorded in the book namedEssential Prescriptions from the Golden Cabinet[15].In 652 C.E., Sun Simiao, a famous physician of the Tang Dynasty of China, used licorice to treat pulmonary fibrosis, which was fully described in his book namedEssential Formulas for Emergencies Worth a Thousand Pieces of Gold[16].With the development of modern medicine, licorice has been widely used for the treatment of several types of lung diseases, such as chronic bronchitis, asthma,COPD, tuberculosis, etc.In 1999, Liu showed that licorice can reverse glucocorticoid resistance by upregulating GR in patients with COPD(this study is published inChin J Tuberc Respir Dis.)[17].Subsequently,in 2013, Kao revealed that licorice can restore glucocorticoid sensitivity by depleting reactive oxygen species (ROS) through heme oxygenase-1 expression, decreasing the phosphorylation of p38 mitogen-activated protein kinases (MAPK), and preventing the phosphorylation of the GR at Ser211 (this study is published inPhytomedicine.) [18].Nowadays, licorice, which was approved for the treatment of various respiratory disorders, is one of the pharmacopeia drugs of China [19].
This review will reveal detailed information about the mechanism of COPD-related glucocorticoid resistance and advances of therapeutic approaches including TCM to restore COPD glucocorticoid sensitivity.
Mechanism of glucocorticoid resistance in COPD
COPD is a chronic heterogeneous lung disease characterized by persistent excessive inflammation that leads to tissue remodeling,alveolar damage, airflow limitation, and an accelerated decline in lung function.While inflammation-based airway injury has been recognized as a core feature of COPD, its exact mechanism in relation to glucocorticoid resistance remains unclear.Recently, it has been found that glucocorticoid resistance in COPD is closely related to the isoform and expression of GR in airway epithelial cells.When GR-α expression is downregulated or GR-β is upregulated, the anti-inflammatory effect of hormones will be significantly weakened,and vise versa, this effect will be strengthened; excessive activation of the phosphatidylinositol-3-kinase (PI3K)/protein kinase B (AKT)signaling pathway, p38 MAPK signaling pathway, and interferon-γ(IFN-γ)/Janus kinase (JAK)/signal transducer and activator of transcription (STAT) signaling pathway in COPD can also cause glucocorticoid resistance.These signaling pathways either phosphorylate or nitrate histone deacetylase (HDAC) 2 or regulate the expression of GR, which lead to a significant insensitivity to glucocorticoids.Nuclear transcription factor-κB (NF-κB) is the switch of cellular inflammatory response, and which is often out of control in COPD-related glucocorticoid resistance.The continuous inflammation waterfall weakens the anti-inflammatory effect of glucocorticoid.Besides, the role of exosome and its microRNA in COPD inflammation and airway remodeling has received more and more attention, which will provide new ideas for studying the mechanism of COPD-related glucocorticoid resistance.This article will review the mechanism of glucocorticoid resistance in COPD from the above content.(Figure 1)
Figure 1 Mechanism of glucocorticoid resistance in COPD.COPD, chronic obstructive pulmonary disease; Gc receptor, glucocorticoid receptor;HDAC2, histone deacetylase 2; NF-κB,nuclear transcription factor-κB;×, cannot exert a therapeutic effect.
GR and COPD-related glucocorticoid resistance
The expression and activity of GRs are essential for glucocorticoid-mediated anti-inflammatory function.GRs are intracellular receptors paired with heat shock protein 90.When glucocorticoids bind to GRs, heat shock protein 90 is released to promote the nuclear translocation of the glucocorticoid-GR complex,in which the complex binds to the GRE and activates related transcription factors, thereby playing an anti-inflammatory role.There are two GR subtypes, namely GR-α and GR-β.GR-α is mainly concentrated in the cytoplasm.When activated, GR-α can form a complex by recruiting HDAC2 and inhibiting the formation of the NF-κB/histone acetyltransferase complex, thus exerting an anti-inflammatory effect.
Conversely, GR-β is a GR-α antagonist with low content that can directly bind to GRE and can weaken the anti-inflammatory activity of GR-α.In peripheral blood mononuclear cells (PBMCs), tumor necrosis factor α (TNF-α), interleukin (IL)-1, IL-17, and IL-23 can upregulate the expression of GR-β [20].Multiple stimuli, such as proinflammatory cytokines and oxidative stress, can regulate GR activity through post-translational modifications such as phosphorylation, acetylation, and ubiquitin-like modifications [21,22].One study showed that the expression and activity of GR-α in alveolar epithelial cells and macrophages significantly decreased after exposure to cigarette smoke (CS) [23].Reddy found that both GR-α expression and activity are downregulated in bronchial epithelial cells from patients with COPD compared with the those of healthy individuals, whereas the activity of proinflammatory NF-κB p65 was elevated, and that of roflumilast stimulated both GR-α mRNA synthesis and GR-α’s transcriptional activity in COPD bronchial epithelial cells.This study demonstrated that roflumilast can mitigate glucocorticoid resistance by enhancing dexamethasone’s ability to suppress proinflammatory mediator production in a GR-α-dependent manner [24].Milara found that peripheral neutrophils from patients with COPD showed an increase in GR-β expression compared with those in healthy individuals, and dexamethasone cannot downregulate it, which indicates a COPD-related glucocorticoid resistance.Roflumilast N-oxide can reverse corticosteroid resistance and shows strong anti-inflammatory effects alone or in combination with dexamethasone by downregulating the expression of GR-β [25].Therefore, GR isoforms influence glucocorticoid sensitivity and play an important role in COPD-related glucocorticoid resistance.
Signaling pathway and COPD-related glucocorti- coid resistancePI3K/AKT signaling pathway and COPD-related glucocorticoid resistance.The PI3K/AKT signaling pathway plays an important role in airway inflammatory diseases by regulating the release of inflammatory mediators, activating inflammatory cells, and in airway remodeling.In recent years, the role of this PI3K/AKT signaling pathway in relation to the inflammatory mechanisms of COPD,glucocorticoid resistance, and anti-inflammatory therapy has been widely studied.Exploring how the emergence of varying signaling molecules that intervene in the PI3K/AKT signaling pathway to prevent and control the occurrence and development of COPD is a key research focus [26, 27].PI3K is a family of proteins that catalyzes the phosphorylation of the 3-OH phosphoric acid inositol and can be divided into three classes, among which the most widely studied is type I.AKT is a key signal transduction molecule in the PI3K signaling pathway.A large number of oxidative stress products exist in COPD.PI3K is activated by the superoxide anion, hydroxyl free radicals, and through oxidative stress products, which then produces the second messenger, phosphatidylinositol-3,4,5-triphosphate.Phosphatidy-linositol-3,4,5-triphosphate binds to the intracellular signaling proteins AKT and phosphatidyl kinase-dependent kinase 1 containing the PH domain, prompting phosphatidyl kinase-dependent kinase 1 phosphorylated AKT protein Thr308 and eventually leading to AKT activation [28].Activated AKT activates downstream target proteins such as NF-κB and caspase through phosphorylation, which regulates the proliferation, differentiation, apoptosis, and migration of proinflammatory factors [29], whereas the expression of HDAC2 has also been shown to be downregulated, leading to a decrease in the anti-inflammatory effects of glucocorticoids.Marwick’s study [30]found that oxidative stress induces PI3K-dependent AKT phosphorylation and reduced glucocorticoid function in vitro, which is restored by PI3K inhibitor.
In vivo, cigaret smoke exposure in mice increased tyrosine nitration of HDAC2 in the lung, correlating with reduced HDAC2 activity and reduced glucocorticoid function.HDAC2 activity and the anti-inflammatory effects of glucocorticoids were restored in PI3K delta kinase-dead knock-in(PI3KδD910A/D910A) but not PI3Kgamma knock-out (PI3Kγ-/-) smoke-exposed mice compared with wild type mice, correlating with reduced HDAC2 tyrosine nitration.Yasuo et al.[31]found that the 50%inhibitory concentration of dexamethasone of PBMCs of COPD were less corticosteroid sensitive than those of nonsmoking and smoking control subjects.PI3K-δ is activated in COPD lungs (in vivo) and by oxidative stress (in vitro).Corticosteroid resistance and reduced HDAC2 activity were reversed by a selective PI3K inhibitor (LY294002).
p38 MAPK signaling pathway and COPD-related glucocorticoid resistance.It has been reported that the basal and lipopolysaccharide(LPS)-induced CXCL8 and p38 MAPK levels were higher in PBMCs from COPD patients as compared to healthy smokers.IL-8 and IL-6 production induced by LPS was more resistant to the suppressive effect of dexamethasone.GW856553, a selective p38 MAPK inhibitor,reverses the anti-inflammatory effect of dexamethasone on LPS-induced CXCL8 and IL-6 release in COPD by preventing phosphorylation of serine 211 on GR.These findings revealed that p38 MAPK-induced GR phosphorylation could contribute to glucocorticoid resistance in COPD [32].
IFN-γ/JAK/STAT signaling pathway and COPD-related glucocorticoid resistance.A study [33] has revealed that IFN-γ levels are increased in patients with COPD compared with healthy subjects.Besides, IFN-γ augmented the effects of LPS on IL-6 and TNF-α production and increased toll-like receptor 2 and toll-like receptor 4 expression in alveolar macrophages (AM) of COPD.Cytokine induction and STAT1 activation by IFN-γ were insensitive to dexamethasone for all groups.The inhibition of JAK and STAT1 reversed all these IFN-γ effects.These findings demonstrate that IFN-γ induced STAT1 signaling contributes to corticosteroid resistance in AMs of COPD and that targeting IFN-γ signaling by JAK inhibitors could restore the anti-inflammatory of dexamethasone in COPD.
Overall, activation of PI3K/AKT signaling pathways was critical for steroid resistance in COPD.PI3K/AKT signaling can decrease the expression of GR, whereas p38 MAPK signaling can impair GR nuclear translocation by phosphorylating the GR at Ser211.IFN-γ signaling increased the steroid resistance by activating STAT phosphorylation.Moreover, PI3K signaling can dampen the level of HDAC2 by activating and heightening oxidative stress, thus aggravating steroid resistance in COPD.
HDAC and COPD-related glucocorticoid resistance
HDAC is an inflammatory gene regulatory enzyme in the body that jointly maintains the dynamic balance of acetylation and the deacetylation of histones in the nucleus and plays a key role in the transcription and silencing of inflammatory genes.Elevated histone acetyltransferase levels or decreased HDAC levels have been shown to significantly upregulate inflammatory gene expression [34].In addition to forming complexes with receptors and moving them into the nucleus, glucocorticoids also need to recruit HDAC in specific regions to work.If HDAC expression is reduced, the anti-inflammatory effect of glucocorticoids can be significantly reduced or resistance can develop.In recent years, several studies have found that HDAC2 was closely associated with COPD-related glucocorticoid resistance.Kazuhiro revealed [35] that there is a graded reduction in HDAC activity and increase in IL-8 messenger RNA and histone-4 acetylation in the lung tissue obtained from patients with COPD, and this decrease of HDAC is correlated with the clinical stages of COPD.The reduction in expression of HDACs in the lung tissue of patients with COPD is selective with a marked reduction in HDAC2, but the other HDACs such as HDAC5 and HDAC8 were less reduced or normal.Decreased HDAC activity is related to corticosteroid resistance, which is a characteristic feature of COPD.John observed [36] that the decreased HDAC2 activity in the lungs of rats is due to protein modification by aldehydes and nitric oxide products present in cigaret smoke and corticosteroid treatment has no effect on smoke-induced proinflammatory mediator release.The possible mechanism of reduction in HDAC2 of patients with COPD may be that [37]: first,HDAC2 is inactivated by peroxynitrite, generated by an interaction of nitric oxide and cigaret smoke and superoxide anions; then,peroxynitrite nitrates tyrosine residues on HDAC2, and this may block HDAC2 activity and also mark the HDAC2 for ubiquitination or destruction by the proteasome; finally, the loss of HDAC2 leads to amplification of the inflammatory response and resistance to corticosteroids.
NF-κB and COPD-related glucocorticoid resistance
NF-κB plays an important role in the immune response, inflammati on,and tumor development, and is therefore considered to be an ideal target for the regulation of immune response, and the prevention and treatment of tumors and inflammation [38].It has been shown that NF-κB can upregulate the expression of inflammatory genes such as IL-1, IL-6, CXCL8 (IL-8), and nitric oxide synthase-2 in the airways of patients with COPD.NF-κB is also a key transcription factor that contributes to increased mucin synthesis [39, 40].Therefore, NF-κB is a key regulator of elevated levels of inflammatory cytokines and mucin in airway epithelium.
Several studies have reported that PI3K and AKT phosphorylation expression levels in pulmonary macrophages and peripheral blood monocytes in patients with COPD were significantly enhanced and that NF-κB, IL-6, IL-8, and TNF-α levels were significantly increased.Conversely, HDAC2 expression and activity were significantly decreased.Forced expiratory volume in 1 second reference percent predictive values positively correlated with HDAC2 expression [7,41].In vitro and in vivo experimental results confirmed that HDAC2 activity and the efficacy of glucocorticoids can be significantly improved by inhibiting inflammatory response under oxidative stress,thus blocking or removing PI3K [25, 42].Further studies have shown that oxidative stress is a key mechanism of COPD-related glucocorticoid resistance by activating PI3K/AKT signaling and downregulating HDAC2 [21, 23] (Figure 2).
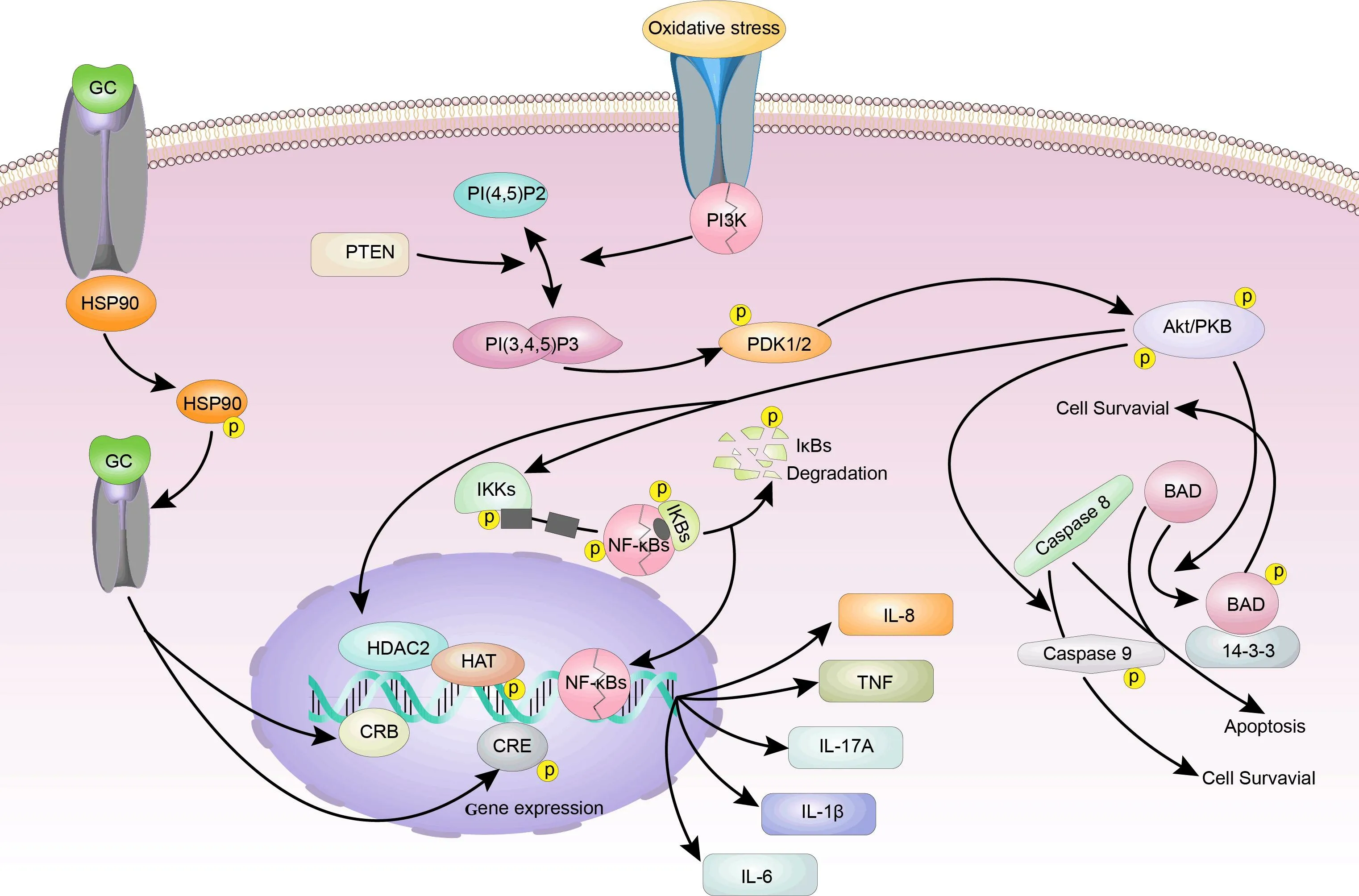
Figure 2 The mechanism of oxidative stress in COPD-related glucocorticoid resistance.COPD, chronic obstructive pulmonary disease; PI3K,phosphatidylinositol-3-kinase; NF-κB, nuclear transcription factor-κB; HAT, histone acetyltransferase; HDAC2, histone deacetylase2; GRE,glucocorticoid response element; IL, interleukin; TNF, tumor necrosis factor; AKT, protein kinase B.
Exosome and COPD-related glucocorticoid resistance
The exosome is a 40–100 nm bilipid nanomembrane vesicle mainly comprised of proteins, RNA (miRNA, lncRNA, and circRNA), DNA,and a small number of lipid molecules.Lung exosomes can be derived from different types of cells of which bronchial epithelial cells and AM are the main sources.CS exposure and air pollution have been shown to change the composition and secretion of lung exosomes [43].In vitro studies have shown that IL-13 stimulation of exosomes secreted by bronchial epithelial cells can promote monocyte proliferation [44].In COPD, the number of macrophages significantly increases.Alveolar macrophage-derived exosomes can inhibit the transport of cytokine signal proteins and the transcription and translation of signal sensors induced by IFN-γ, all of which indicate that macrophage-derived exosomes play an important role in chronic airway inflammation[45].Studies have shown that exosomes are an important medium for cell-cell signal transmission and play an important role in the occurrence and development of COPD by transporting bioactive substances in the cytoplasm to target cells and mediating information exchange between cells [46].For example, Kristopher [47] revealed that exosomes derived from activated polymorphonuclear leukocytes can bind and degrade the extracellular matrix via the integrin Mac-1 and neutrophil elastase, respectively, causing the formation of COPD.These exosomes have the characteristics of extracellular matrix targeting and α1AT resistance, which exist in clinical specimens from subjects with COPD but not healthy individuals, and are capable of transferring a COPD-like phenotype from humans to mice in a polymorphonuclear-driven manner.Exosomes are just delivery vehicles, which act by transporting the cargo they contain, such as miRNAs, to target cells.Although advances have been made in understanding the role of exosomes in COPD, there is almost no published literature about the exosome and COPD glucocorticoid resistance.Because glucocorticoid resistance is widespread in COPD and studies have reported the roles of exosomes in COPD, we speculate that exosomes are also closely related to glucocorticoid resistance in COPD;however,the specific mechanism remains unclear.
MicroRNA and COPD-related glucocorticoid resistance
MicroRNAs stored in exosomes are a class of non-coding RNAs of approximately 22 nucleotides in length, and their main role is to negatively regulate gene expression at the post-transcriptional level by binding to target gene mRNA [48–50].Studies have shown that there is a close relationship between miRNAs and COPD.Smoking can lead to significant changes in miRNA expression in AM and bronchial airway epithelial cells of patients with COPD [51].For example, Graff et al.compared the expression of miRNAs in AM between smokers and non-smokers and found that the expression of 11 miRNAs, including miRNA-132 and miRNA-139, in the AM of smokers were increased,whereas the expression of 43 miRNAs, including miRNA-452 and miRNA129-3P, were decreased.Compared with light smokers,individuals with a history of heavy smoking had more changes in miRNA expression levels, suggesting a correlation between miRNA differential expression and smoking history [52].Heliot et al.also reported that compared with non-smokers, exosome miRNA-21 levels in the bronchoalveolar lavage fluid of smokers were increased,whereas let-7e and let-7g levels were decreased [53].
Currently, although the mechanism between miRNAs and COPD-related glucocorticoid resistance remains unclear, the role of miRNAs in the steroid resistance of COPD has begun to attract attention.Stolzenburg et al.showed that miRNA-223 was increased in the lungs of smokers, and the increased expression of miRNA-223 was related to the decreased expression of HDAC2, which would lead to the expansion of inflammation and corticosteroid resistance[54].
In COPD models, the mechanism of glucocorticoid resistance is very similar to that of severe asthma.Studies have shown that miRNA-21 was upregulated in a severe, steroid-insensitive experimental asthma model.MiRNA-21 antagomir can reverse steroid resistance by increasing the expression of miR-21 target phosphatase, tensin homolog, and HDAC2 levels, thus reducing PI3K activity [55].Exposure to IFN-γ/LPS can upregulate the expression of miR-9 expression of lung macrophages, which induces glucocorticoid resistance by reducing levels of its target transcript, protein phosphatase 2 regulatory subunit B isoform, and attenuating protein phosphatase 2A activity and inhibited dexamethasone-induced GR nuclear translocation.MiRNA-9 antagomir increased both protein phosphatase 2A activity and GR nuclear translocation in macrophages and restored steroid sensitivity in steroid-resistant airway hyperresponsiveness [56].Moreover, there is a mutual regulatory relationship between miRNAs and NF-κB.Studies have shown that miRNA-218 uniformly downregulates lung tissue or circulating body fluids in patients with COPD [57–59].MiRNA-218 binds to tumor necrosis factor receptor 1, blocks the release of tumor necrosis factor receptor 1 induced IL-6 and IL-8, and reduces the activity of NF-κB,thereby reducing airway inflammation [59].In vitro studies have shown that miRNA-218 plays an important role in the antagonism of andro against the inflammatory response and oxidative stress of alveolar epithelial cells [60].
The potential mechanism of exosomes and miRNA in glucocorticoid resistance in COPD can be seen in Figure 3.
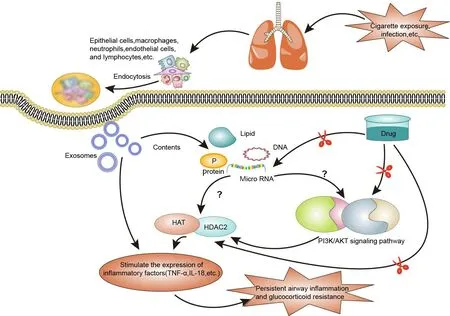
Figure 3 The potential mechanism of exosomes and miRNA in COPD-related glucocorticoid resistance.COPD, chronic obstructive pulmonary disease; HAT, histone acetyltransferase; HDAC2, histone deacetylase2; TNF, tumor necrosis factor; IL, interleukin; PI3K,phosphatidylinositol-3-kinase; AKT, protein kinase B.
The approaches to establish the glucocorticoid resistance model associated with COPD
Glucocorticoid resistance is primary in COPD and is positively correlated with disease severity and lung function.Currently, there is no special protocol for establishing the glucocorticoid resistance model associated with COPD.Frequently, a common COPD model is used to represent the COPD-related glucocorticoid resistance model in literature reports.The most common method to establish a model in vitro is to continuously expose the mouse to cigaret smoke or combine it with LPS tracheal instillation; in in vivo models, researchers often expose PBMCs or airway epithelial cells of a patient with COPD to cigaret smoke extracts to prepare glucocorticoid resistance models[31,32, 36].For example, Marwick et al.established a glucocorticoid resistance model in vivo by exposing mice to cigaret smoke (5 × 1 R3F cigarets/day) on three consecutive days.Meanwhile, they exposed U937 cells to H2O2, a product of oxidative stress, to prepare an in vitro model of glucocorticoid resistance related to COPD [30].
Therapeutic approaches to reverse corticosteroid resistance in COPD
Recently, Western medicine has made great advances in the mechanism of glucocorticoid resistance in COPD.Studies have shown that clarithromycin, erythromycin, aminophylline, phosphodiesterase 3/phosphodiesterase 4 inhibitors (roflumilast), tiotropium bromide,carboxysteine, progesterone, and ubiquitin-specific peptidase 17 have glucocorticoid sensitivity restoring effects in in vitro experiments by regulating GR activity or isoform, or inhibiting the PI3K/AKT signaling pathway, or increasing the expression of HDAC2 [13, 18, 19, 61–66] (Table 1).
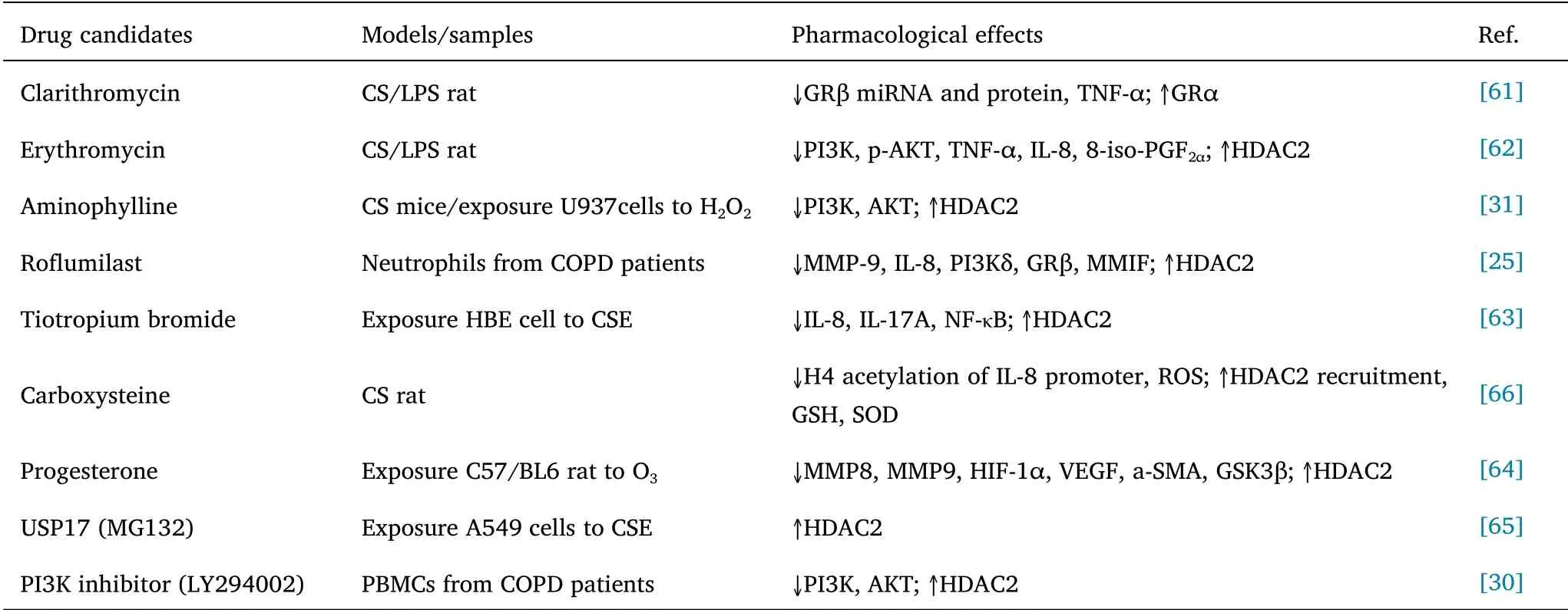
Table 1 Therapeutic candidates capable of reversing corticosteroid resistance in COPD
Although there is much drug discovery effort to identify novel therapeutics to restore GR in experimental models of COPD, few clinical drug trials are aiming to develop this aspect of therapy.Many drugs, such as aminophylline, however, have demonstrated GR reversing effects in COPD models.A recent randomized clinical trial showed that adding theophylline to inhaled corticosteroid failed to reduce the number of COPD exacerbations and improve health status,modified medical research council, dyspnea score, and COPD assessment test as compared to corticosteroid treatment alone [67].Moreover, long-term use of these above drugs also needs to overcome related adverse reactions.Therefore, there is currently a lack of evidence-based research on medication that can effectively address COPD-related glucocorticoid resistance in the clinical setting.
TCM has been considered to have a definite therapeutic effect on COPD by reducing airway inflammation and improving clinical symptoms and quality [68–72].The combination of glucocorticoids and TCM not only enhances the efficacy, but also reduces the side effects of glucocorticoids, such as osteoporosis and fat metabolism disorders [8–11].Recent studies have shown that TCM or the herb′s extract can regulate the expression of GR, p38 MAPK signaling,HDAC2, and NF-κB in COPD models to reverse glucocorticoid resistance(Table 2).
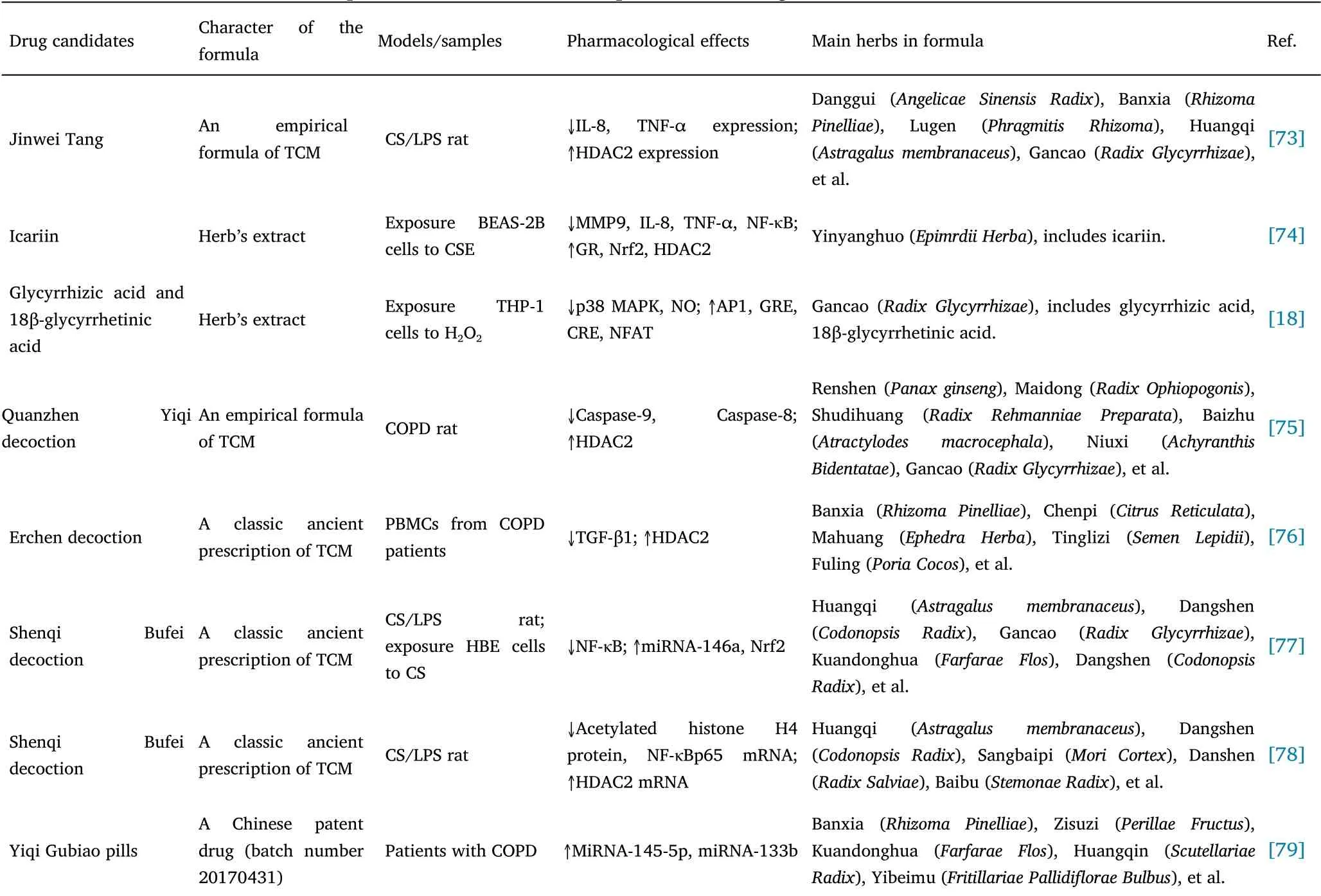
Table 2 Therapeutic candidates of TCM capable of reversing corticosteroid resistance in COPD
For example, Wu found that the empirical formula of the Chinese medicine Jinwei Tang combined with budesonide inhalation could improve the therapeutic effect in treating COPD-related glucocorticoid resistance by upregulating HDAC2 expression and lowering TNF-expression [73].Hu revealed that icariin, a major component of flavonoids isolated fromEpimedium brevicornumMaxim.can exert a positive effect on glucocorticoid resistance by regulating the expression of glucocorticoid resistance-related factors, such as GR,HDAC2, nuclear factor erythroid-2-related factor 2, and NF-κB [74].Glycyrrhizic acid and 18β-glycyrrhetinic acid, two bioactive compounds isolated from licorice can restore glucocorticoid sensitivity by depleting ROS through heme oxygenase-1 expression, decreasing the phosphorylation of p38 MAPK, preventing the phosphorylation of GR at Ser211, and activating PI3K-induced activator protein 1, GRE,cyclic adenosine monophosphate response element, and nuclear factor of activated T-cells [18].An empirical formula of the Chinese medicine Quanzhen Yiqi decoction has been reported to induce the apoptosis of AM in COPD, regulate the expression of HDAC2, and produce an overall anti-inflammatory effect [75].Chen et al.found that a classic ancient prescription of the Chinese medicine Erchen decoction may play a role in protecting lung tissue by upregulating HDAC2 gene expression in PBMCs and inhibiting transcription and translation of the transforming growth factor beta1 gene, thereby working to suppress airway inflammation in rats with COPD [76].Moreover, TCM can also improve inflammation levels in patients with COPD by regulating miRNA expression.Shenqi Bufei decoction, a classic ancient prescription of Chinese medicine, could increase the expression of miRNA-146a, HDAC2, and Nrf2 in the lung tissue of model rats with COPD, and reduce NF-κB, thereby showing anti-inflammatory effects[77,78].Jin et al.found that the Chinesepatent drug Yiqi Gubiao pills (produced by Xinjiang Pharmaceutical Factory, provided by the central pharmacy of the Affiliated Traditional Chinese Hospital of Xinjiang Medical University, batch number: 20170431) could effectively alleviate the clinical symptoms of patients with stable COPD, improve the levels of miRNA-145-5p and miRNA-133b in peripheral blood, and reduce the systemic inflammatory response in these patients [79].Although the above studies have shown that TCM has made some advances in the treatment of GR, the exact mechanisms remain unclear.Whether TCM can improve COPD-related glucocorticoid resistance by regulating the PI3K/AKT and other signaling pathways, even targeting the exosomes and microRNA remains unclear.
Summary and future perspectives
GR remains an ongoing challenge and is key to the clinical management of COPD.Currently, the role of exosomes and miRNAs in COPD has received increasing attention; however, the mechanism of their role in COPD-related glucocorticoid resistance remains unclear.TCM has many advantages in treating COPD, as we mentioned in the background of this article, it is worth exploring.The characteristics of exosomes, such as cellular origin, wide distribution, biocompatibility,biological function, and targeted transport all meet the material requirements of the TCM theory.Exosomes can be regarded as a targeted messenger between Zang-fu organs (Zang-fu organs are functional entities stipulated by traditional Chinese medicine),secreted by various Zang-fu cells, along Zang-fu-related routes,targeting specific entities, and regulating the function of target organs.Moreover, it is possible to predict the targeted movement and biological function of exosomes using the Zang-fu-related theories of TCM.Therefore, exosomes can be used to interpret the material basis and molecular mechanism of Zang-fu-related theories [80].In relation to COPD, the TCM theory related to the lung and kidney is consistent with the characteristics of exosome targeted regulation and long-distance transmission, which suggests that TCM can be studied in terms of “regulating lung and kidney therapy” for COPD-related glucocorticoid resistance alongside an exosome perspective.
GR receptor activity or phenotype, activation signaling pathway of PI3K/AKT, p38 MAPK, and IFN-γ/JAK/STAT, and downregulation of HDAC2 expression through CS exposure are the core mechanisms involved in COPD-related glucocorticoid resistance.Furthermore,exosomes and miRNAs produced by airway epithelial cells and macrophages are closely related to steroid resistance in COPD.However, the role of exosomes and miRNAs in COPD-related glucocorticoid resistance and their relationship with the PI3K/AKT signaling pathway and HDAC2 remain unclear.Further studies investigating the mechanism of their interaction in COPD-related glucocorticoid resistance may help to identify new intervention targets and reveal the molecular basis of TCM in improving COPD-related glucocorticoid resistance.
 Traditional Medicine Research2021年5期
Traditional Medicine Research2021年5期
- Traditional Medicine Research的其它文章
- The protective effect of a standardized hydroalcoholic extract of Prosopis farcta(Banks&Sol.)J.F.Macbr.fruit in a rat model for experimental ulcerative colitis
- Neuroprotective effect and mechanism of daidzein in oxygen-glucose deprivation/reperfusion injury based on experimental approaches and network pharmacology
- Understanding the prevention and cure of plagues in Daoist medicine
- Efficacy of Xianglian pill for antibiotic-associated diarrhea:a protocol for systematic review and meta-analysis
- Effects of Dendrobium candidum polysaccharides on microRNA-125b and mitogen-activated protein kinase signaling pathways in diabetic cataract rats
- Light and color therapy: the role of light and color in architecture from the perspective of traditional Persian medicine
