Relationship between molecular changes in epidermal growth factor receptor (EGFR)and anaplastic lymphoma kinase (ALK)mutations in lung adenocarcinoma *
Rina Na ,Wei Luan (Co-first author),Yinzai He ,Yanwei Gao ,Nier Cha ,Baoqin Jia (✉)
1 Department of General Surgery,Inner Mongolia People's Hospital,Hohhot 010017,China
2 Department of Oncology,Inner Mongolia People's Hospital,Hohhot 010017,China
3 Department of Surgical Oncology,Inner Mongolia People's Hospital,Hohhot 010017,China
Abstract Objective This study aimed to analyze the relationship between the mutations in epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) and their impact on the prognosis and treatment of lung adenocarcinoma.Methods A total of 158 cases of lung adenocarcinoma reported between January 2007 and January 2014 were retrospectively analyzed.These tumors were resected using radical pneumonectomy and underwent pathology-based diagnosis at our institution (Inner Mongolia People’s Hospital,Hohhot,China).The tissue sections were evaluated using the updated World Health Organization classification of lung adenocarcinomas (2015 version),with each histological component recorded in 5% increments.The histological subtypes were classified,and any surviving cases were followed up.The reverse transcriptionpolymerase chain reaction (RT-PCR) and direct DNA sequencing were used to evaluate mutations in exons 18,19,20,and 21 in the EGFR gene,and the echinoderm microtubule-associated protein-like 4 gene-ALK variant (EML4-ALK) fusions were detected using sequencing.Results Our cohort included 25 patients with pre-invasive adenocarcinoma,13 patients with lepidic,66 patients with acinar,13 patients with papillary,and 25 patients with solid infiltrative adenocarcinoma with the remaining cases presenting with a variety of pathological subtypes.The prognosis of each histological subtype was different with the 5-year disease-free survival and 5-year overall survival (OS) of pre-invasion adenocarcinoma at 100%;the 5-year OS of lepidic,acinar,and papillary adenocarcinoma patients was only 84.6%,72.7%,and 76.9%,respectively.The 5-year OS of solid and mucinous adenocarcinomas were 32.0% and 36.4%,respectively.EGFR mutation was detected in 69 cases with a mutation rate of 43.7% and majority of these mutations were found in exons 19 (50.6%) and 21 (37.9%),with women and non-smokers shown to experience a higher mutation rate (P <0.05).However,histological subtype analysis showed that EGFR mutations were primarily found in adenocarcinomas.Most of these mutations were found in lepidic(53.8%) or acinar adenocarcinomas (50.0%),whereas these mutations were rare in both solid (28.0%) and mucinous adenocarcinoma (27.2%).The fusion mutation rate in the EML4-ALK gene was 5.69%,and was most common in young,nonsmoking patients (P <0.05).Conclusion The prognosis of patients in each lung adenocarcinoma subtype is different,and these outcomes are likely related to mutations in the EGFR and EML4-ALK genes.EGFR mutation rates are higher in lepidic and acinar adenocarcinomas,whereas EML4-ALK gene fusion mutations are more common in solid and mucinous adenocarcinoma.EGFR mutations are more common in female and nonsmoking patients,whereas EML4-ALK fusions are more common in young,non-smoking patients.
Key words: lung cancer;histological subtypes;prognosis;the echinoderm microtubule-associated protein-like 4 gene-ALK variant (EML4-ALK);epidermal growth factor receptor (EGFR)
More than half of all newly diagnosed non-small cell lung cancer is lung adenocarcinoma that has variable genetic and morphological patterns and presents with a variety of clinicopathological characteristics.The World Health Organization (WHO) published a new classification system for lung tumors in 2015 which relies on histologybased classification terms[1].Epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK)have been identified as the critical genetic drivers for lung adenocarcinoma,and both act as critical prognostic factors in this disease.This study aimed to explore the relationship between the various histological types of lung adenocarcinoma and common gene mutations,as well as the clinicopathological characteristics of these patients in an effort to provide new insights into individualized treatments for this disease.
Materials and methods
Tissue samples
We collected the data from 158 cases of lung adenocarcinoma treated at the Department of Oncology,Inner Mongolia People’s Hospital,Hohhot,China,between January 2007 and January 2014.All patients signed an informed consent and both the clinical and pathological data of the patients were reviewed,and the relevant information was recorded,including gender,age,smoking history,tumor size,tumor location,and tumor stage.Any patients receiving preoperative adjuvant radioor chemotherapy were excluded,and staging (tumor,lymph node,and metastasis) was performed according to the guidelines established in the 7th edition of the United States Joint Committee on lung cancer staging system.The follow-up information collected for surviving patients included preoperative staging,surgical methods and the treatment outcome of patients after operation,etc.
Pathological examinations
Hematoxylin and eosin (H&E)-stained sections from each of the tissue samples were re-examined by two experienced pathologists and classified using the new WHO lung adenocarcinoma classification system(2015).These reexaminations included a reevaluation of the e morphological standard and the histological subtype of the tumor which were then classified as:in situadenocarcinoma (AIS),minimal invasive adenocarcinoma (MIA),lepidic adenocarcinoma (LPA),acinar adenocarcinoma,papillary adenocarcinoma,solid adenocarcinoma with mucus formation,micropapillary adenocarcinoma,invasive mucinous adenocarcinoma,enteric adenocarcinoma,and colloidal carcinoma.Each histological component was recorded in 5% increments and the degree of tumor differentiation,tumor thrombus,mitotic number (/10 hpf),necrosis and the relationship between the tumor and pleura were evaluated and recorded.All diagnostic criteria were then omitted.
Specimen preparation
All samples were fixed in neutral formaldehyde and embedded in paraffin.The blocks with tumor tissue were selected and each paraffin block was cut into 4-micronthick sections,subjected to H&E staining and evaluated under a microscope.A block with a tumor component ratio of greater than 75% was selected for each case.Four to five 5 µM thick sections were placed into a 1.5 mL tube and then subjected to genetic evaluation.Genetic analysis of the tumor was performed in 158 patients.EGFRmutations were detected by Sanger sequencing or amplification refractory mutation system,as previously described.ALKalterations were detected by fluorescencein situhybridization with ALK break apart probes and/or immunohistochemistry (IHC) staining with Ventana anti-ALK antibody as previously described.Mutations in exons 18,19,20 and 21 of theEGFRgene and the echinoderm microtubule-associated protein-like 4 gene-ALK variant(EML4-ALK)fusions were analyzed by reverse transcription-polymerase chain reaction (RTPCR) and direct DNA sequencing.
Statistical analysis
SPSS 22.00 (IBM Corp.,Armonk,NY,USA) was used to analyze the data.Chi-square analysis was used to evaluate the correlation betweenEGFRandALKmutations and associated information,and the log-rank test was used to evaluate the survival rate in each group.APvalue of <0.05 was set as statistically significant.
Results
Our cohort comprised of 70 males and 88 females at an average age of 59.1 years (30–77 years),with these 158 participants including 120 nonsmokers (75.9%).Our participants spanned various tumor types and stages,with 63 participants in stage I,44 in stage II,41 in stage III,and 10 cases at stage IV.These included 25 cases of pre-invasion adenocarcinomas,including lepidic adenocarcinoma(13 cases),acinar adenocarcinoma (66 cases),papillary adenocarcinoma (13 cases),solid adenocarcinoma (25 cases),and other pathological subtypes.The follow-up time spanned between 22–112 months,and four cases(one lepidic,two acinar,one papillary) were lost to follow up.A total of 119 patients survived their initial disease with 13 experiencing tumor recurrence and metastasis,and 35 dying before the end of the study.The prognosis of each histological subtype was different (Table 1),with the 5-year disease-free survival and overall survival (OS) at 100% forin situand minimally invasive adenocarcinoma,and 84.6%,72.7%,and 76.9% for lepidic,acinar,and papillary adenocarcinoma,respectively.The 5-year OS rates in solid and mucinous adenocarcinoma were only 32.0% and 36.4%,respectively.
Of the 158 samples,69 exhibited detectable mutations in theEGFRgene,making the overall mutation rate for this gene 43.7%.The majority of these mutations were found in exons 19 (50.6%) and 21 (37.9%),and these mutation rates were significantly higher in female patients (54.5% for women and 30% for men;P<0.05).The mutation rate in the non-smoking group (49.2%)was higher than that of the smoking group (26.3%),with this difference also demonstrating statistical significance (P<0.05).However,age,tumor size,stage,pleural involvement,and lymph node metastasis werenot found to be related toEGFRmutation rates in these patients.Histological subtype analysis showed thatEGFRmutation was more common in lepidic (53.8%) and acinar type adenocarcinomas (50.0%),whereas these mutations were rarer in solid tumors (28.0%) and mucinous adenocarcinomas (27.2%).Fusion mutation,EML4-ALK,was identified in 5.69% of the samples and was found to be more common in young and non-smoking patients (allP<0.05).This fusion was also more common in mucinous and solid adenocarcinomas (Table 2).
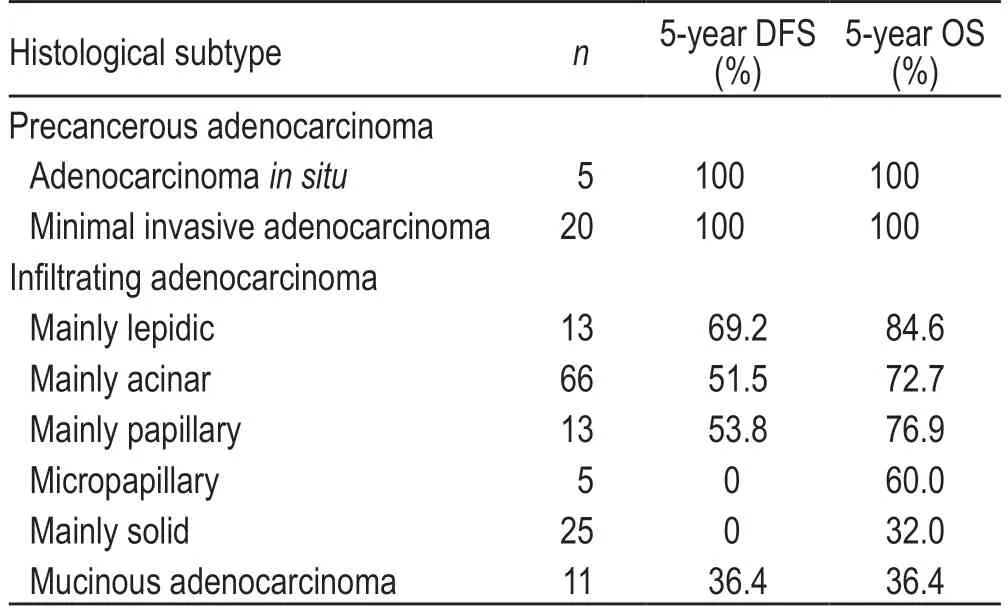
Table 1 Survival and histological subtype of lung adenocarcinomas

Table 2 Mutational analysis of 158 cases of lung adenocarcinoma [n (%)]
Discussion
This study demonstrates that the new classification method for lung adenocarcinomas may be predictive for curative effect,prognosis,and tumor metabolism[2–5],and suggests that this new classification method can be used to supplement clinical treatment decision-making using tumor staging.The prognosis of each histological subtype of lung adenocarcinoma is different.Bothin situand minimally invasive adenocarcinoma have a 5-year diseasefree survival of 100% and a 5-year total survival of 100%,suggesting that these patients may only need surgical resection without adjuvant treatment;the prognosis of lepidic,acinar,and papillary adenocarcinoma is moderate;however,solid and mucinous adenocarcinomas have a 5-year OS of 32.0% and 36.4%,respectively,with very poor prognosis.This suggests that some of these patients may need adjuvant treatment after surgery and a growing number of studies have confirmed that both the micro papilla and solid components are directly related to poorer prognosis[6–7],which has the added value of helping to predict the survival odds of patients independent of tumor stage.The appearance of solid components also indicates that the tumor is more invasive,rendering it necessary to include the micropapillary and solid elements in the pathological report using 5% increments.
Recent evaluations have continued to expand our understanding of the genetic origins and drivers of lung cancer and molecular typing,based on genetic characteristics,helps to take the treatment of advanced lung cancer into the realm of individualized treatment.EGFRmutations are an important predictor of targeted therapy in lung adenocarcinoma and have been widely applied in clinical intervention trials.TheEGFRmutation rate in lung cancers in Caucasian patients is approximately 10%,whereas in Asian patients,it can be as high as 30% to 40%[8].Most of these mutations occur in young,female,non-smokers and the majority of theseEGFRmutations have been linked to the clinical characteristics of the tumor,including histology,race,gender,etc.The results of this study showed that theEGFRmutation rate in this cohort was 43.7%,with majority of mutations in exons 19 and 21.Women and non-smokers had a higher mutation rate,which is similar to other reports,but there were no correlations betweenEGFRmutation and age,tumor size,stage,pleural involvement or lymph node metastasis.Histological subtype analysis showed that majority ofEGFRmutations were identified in lepidic and acinar adenocarcinoma,whereas these mutations were rarer in the solid and mucinous adenocarcinoma samples.Histological features such as lepidic structure and acinar structure may predictEGFRmutation better than other clinical parameters.It was also found that theEGFRmutation rate in mucinous adenocarcinoma was lower(27.2%) than that of non-mucinous adenocarcinomas with lepidic structure (53.8%).
ALKfusions have been shown to define a unique molecular subtype in lung adenocarcinomas.Our data revealed a 5.69% occurrence ofALKfusion mutations in the lung adenocarcinomas of this cohort,with the average age of these patients being significantly lower than theALK-negative group,which was consistent with other results in the literature[9].The relationship between smoking history andALKfusions is controversial,with several studies suggesting thatALKfusions are more common in nonsmokers,but several other papers reporting that smoking history is not a significant factor inALKfusion mutations.This study shows thatALKfusions were significantly more common in nonsmokers in this cohort,but the specific mechanism underlying this correlation requires further study.There was no significant difference in theALKfusion rate between the sexes which is significantly different from theEGFRgene,where these mutations are generally believed to be more common in women.Studies from western countries have suggested thatALKfusion-positive cases are more common in acinar like tumors[10],whereas others have found that Japanese patients with mucus secretion and cribriform-like lung adenocarcinomas have higherALKpositive rates[11].However,studies in China show that theALKmutation rates are significantly higher in infiltrating mucinous and solid infiltrating adenocarcinomas in Chinese patients.There were no fusion mutations in preinvasion adenocarcinomas,suggesting that these fusions may be a late event in the development of lung cancer.Early detection is one of the most relevant limiting factors in the treatment of lung cancer.This work may contribute to the early detection of lung cancer.
Conflicts of interest
The authors indicated no potential conflicts of interest.
 Oncology and Translational Medicine2021年4期
Oncology and Translational Medicine2021年4期
- Oncology and Translational Medicine的其它文章
- Mechanism of tumor synthetic lethal-related targets
- Relationship between miR-7-5p expression and 125 I seed implantation efficacy in pancreatic cancer and functional analysis of target genes*
- The clinical efficacy of percutaneous ethanol-lipiodol injection (PEI) combined with high-intensity focused ultrasound (HIFU) for small hepatocellularcarcinoma in special or high-risk locations*
- Enhancing the treatment effects of tumor cell purified autogenous heat shock protein 70-peptide complexes on HER-3-overexpressing breast cancer *
- Efficacy and adverse reactions of apatinib as secondline or later-line treatment in advanced lung cancer
- The expression of vascular endothelial growth factor (VEGF)/ endostatin (ES) and VEGF receptor 2(VEGFR2)/ES is associated with NSCLC prognosis *
