A study of the potential adverse effects of electrosurgical smoke on medical staff during malignant tumor surgery*
Zhaoxia Luo,Xiuze Li,Shuhua Li,Bo Hou (✉)
1 Operation Room,Mianyang Central Hospital,Mianyang 621000,China
2 Department of Anesthesiology,Mianyang Central Hospital,Mianyang 621000,China
3 Department of Otolaryngology,Mianyang Central Hospital,Mianyang 621000,China
Abstract Objective The aim of this study was to investigate the potential adverse effects of electrosurgical smoke on medical staff performing malignant tumor surgery.Methods This study was divided into two parts:in vitro and in vivo experiments.The human thyroid cancer cell line,ARO,was cultured and passaged.The tumor cells were burned with an ultrasonic scalpel,and the surgical smoke was absorbed by a transwell membrane.The captured particles were diluted in 3 mL of culture medium,and cell survival was assessed under a microscope.DNA was extracted from the cells for genotyping.BALB/c mice were used to construct thyroid cancer xenograft models.The tumor tissues were dissected on day 14 using an ultrasonic scalpel.The smoke from the electrosurgical procedure was collected on a transwell membrane.The membrane was washed in 2 mL of rinsing solution,and the solution was then injected into the right armpit of 10 mice.After sacrifice,the tumor tissues were removed and stained with hematoxylin and eosin (HE).Results Viable ARO cells could be seen on the first day after culturing cell fragments from surgical smoke,and vigorous cell proliferation could be seen on the 17th day of incubation.The genotype of the cells cultured in the presence of smoke particles was identical to the genotype of the original cells.Tumor growth was observed in four out of 10 mice injected with the smoke particle rinse.HE staining showed a significantly increased number of nuclei in the tumor tissue,which was consistent with the general morphological characteristics of malignant tumors.Conclusion Viable tumor cells were detected in surgical smoke generated by ultrasonic scalpel dissection,and these cells had growth activity.Thus,it is necessary to protect patients and medical staff from electrosurgical smoke.
Key words: electrosurgery;ultrasonic scalpel;malignant tumor;smoke
Electrocautery,radiofrequency ablation,and ultrasonic scalpels are the commonly used electrosurgical techniques and tools for cutting,dissecting,and solidifying tissues during surgery[1].Operating rooms do not have special devices to protect against electrosurgical smoke,even though patients and the operating room medical staff are exposed to surgical smoke generated by electrosurgical equipment[2].Surgical smoke is composed of the gaseous by-products of evaporated tissues and is mainly composed of 95% water vapor and 5% combustion particles,which contain a large number of chemical substances,blood and tissue particles,viruses,or bacteria[3].The nature of surgical smoke differs according to differences in the energy of the device being used and the tissue being cut[4].Other possible influencing factors include the type of operation,the skill of the surgeon,and the power level of the instruments and devices.Surgical smoke can produce irritating gases and release potentially harmful substances[5].Previous studies have raised concerns about the risk of infection,mutation,and the diffusion of malignant cells during electrosurgical procedures[6].Exposure to surgical smoke has adverse effects on the cardiovascular and respiratory systems.Surgical smoke has been shown to be cytotoxic,genotoxic,and mutagenic,and it is also a potential biological hazard[7].However,there are few studies on the potentially harmful effects of residual malignant tumor cells in surgical smoke.Therefore,the purpose of this study was to explore the effects of residual malignant tumor cells in surgical smoke on medical staff and determine whether these cells still have growth potential.
Materials and methods
Experimental cells,animals,and instruments
The human thyroid cancer cell line,ARO,was purchased from the Kunming Cell Bank,Chinese Academy of Sciences.Roswell Park Memorial Institute(RPMI) 1640 medium was purchased from Wuhan Sanying Biotechnology Co.,Ltd (Wuhan,China).Fetal bovine serum was purchased from Hangzhou Sijiqing Company (Hangzhou,China).Hematoxylin and eosin and immunohistochemical staining kit purchased from Beijing Jin Zijing Biomedical Technology Co.,Ltd.(Beijing,China).A Reflex Ultra 45 radiofrequency ablation system and an ultrasonic scalpel were purchased from Shanghai Zhiheng Medical Device Co.,Ltd.(Shanghai,China).Semi-permeable polyester membranes were purchased from Shenzhen Boanno Technology Co.,Ltd (Shenzhen,China).Twenty SPF BALB/c mice were obtained from the Institute of Field Surgery,the Third Affiliated Hospital of the Third Military Medical University,China (animal certificate no.:0001517,laboratory animal license no.:syxk [Yu] 2017-0005).Adaptive feeding was performed for 2 weeks,with free access to food and drinking water.All experiments were conducted in accordance with the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health.
In vitro experiments
In vivoandin vitroexperiments were performed in a standard animal operating room.ARO cells were cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS) and 1% penicillin and streptomycin.All tumor cells were maintained in an incubator at 37°C,with 5% carbon dioxide.The cells were passaged every 3 days.Cells were digested with 25% trypsin for 3 min,and then,the single cell suspensions were obtained by pipetting.Cells were passaged at a concentration of approximately 2 × 106cells/mL.The tumor cells in the culture medium were burned with an ultrasonic scalpel,and the resulting surgical smoke was absorbed by a vacuum pump (15 cmHg) connected to a syringe equipped with a transwell membrane.The membrane was located 5 or 10 cm away from the target cell line (Fig.1).The smokecollection membrane had a dense double-layer structure to effectively separate the gaseous smoke.The particles captured on the transwell membrane were diluted with 3 mL of RPMI medium.The diluted medium was cultured in an incubator at 37 °C,and cell survival was assessed by observation under a microscope.Genotyping was performed to determine whether the cells in the surgical smoke were the same as the original tumor cells.
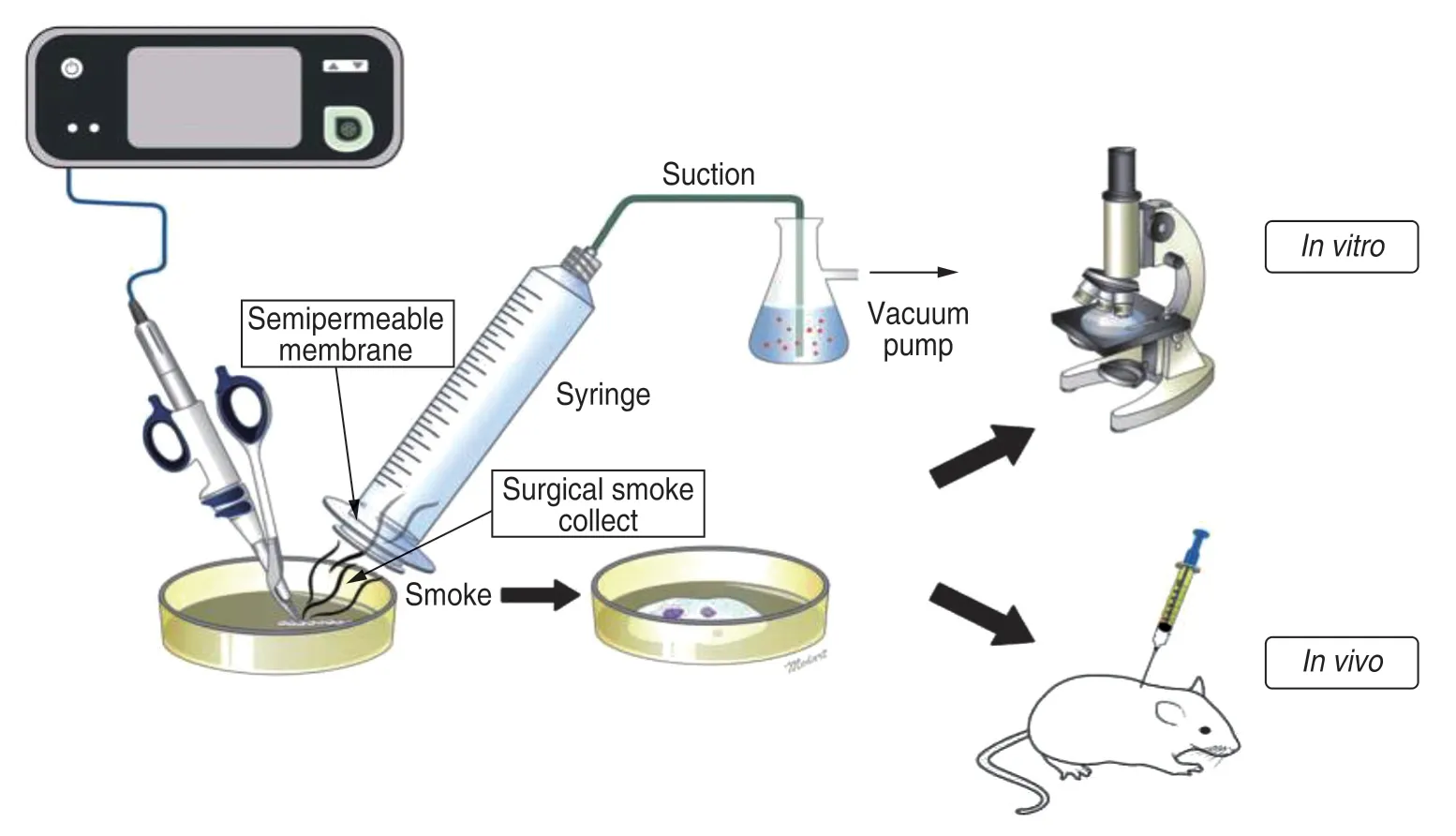
Fig.1 In vitro and in vivo experimental models
In vivo experiments
In vivoexperiments were divided into two parts.In the first part,1 × 105ARO cells were injected into the right armpits of 10 BALB/c mice.The growth of cancer cells was then observed in these mice.After 14 days,the tumor tissue was dissected with an ultrasonic scalpel,under 3%halothane anesthesia administered using a mask.The tumor tissue was dissected with an ultrasonic scalpel according to the standard procedure used for human malignant tumor surgery.The tumor tissue was dissected with 2 cm of normal tissue around the tumor tissue.A transwell membrane system was used to collect the electrosurgical smoke generated during the procedure.After collection,the smoke was eluted in 2 mL of TBST(Tris-buffered saline with Tween solution).In the second part of the experiment,the collected rinsing solution was injected into the right armpits of 10 BALB/c mice,and tumor growth was observed over a period of 3 weeks.At the end of the experimental period,the anesthetized mice were sacrificed via an intraperitoneal injection of pentobarbital.The site of the tumor was scraped clean,the subcutaneous nodules were fully exposed,and the tumor tissue was completely removed.
Hematoxylin and eosin (HE) and immunohistochemical staining
Tumor tissue was embedded in paraffin,sectioned,baked,and cryopreserved after cooling (each piece was cut at 4 μm thickness intervals and baked at 60 °C in 30 min).Tissue sections were dewaxed with xylene and then hydrated through an ethanol gradient.They were then stained with hematoxylin for 30-60 s,washed for 5 min,stained with eosin for 30 s,and washed again for 5 min.After dehydration through an ethanol gradient,the sections were dried,incubated in xylene,and sealed with neutral gum.Stained sections were observed under an Olympus®Bx50 optical microscope (Olympus,Tokyo,Japan),and images were captured.
Results
Result of in vitro culture of membrane particles
After culturing cell fragments within surgical smoke,viable ARO cells could be seen on the first day.On the 17th day,vigorous cell proliferation could be seen,and the cells almost entirely covered the surface of the culture plate (Fig.2).This indicated that a certain number of tumor cells survived in surgical smoke,and as they were not completely inactivated,they had strong growth potential.
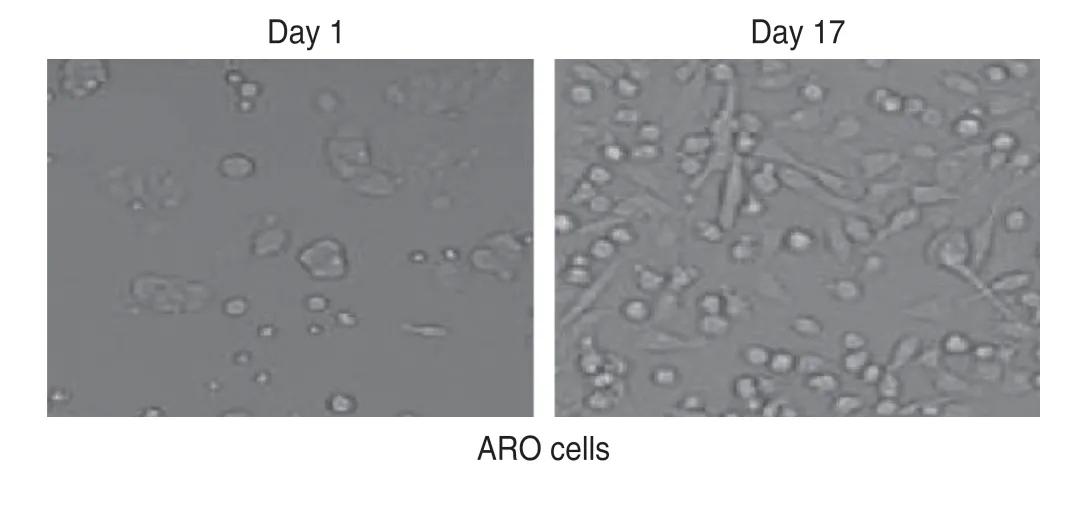
Fig.2 Cultured cells from membrane particles
Genotyping analysis
Genotyping analysis showed that the cells in the smoke particles collected using the membrane system were genetically identical to the original ARO cells (Fig.3).
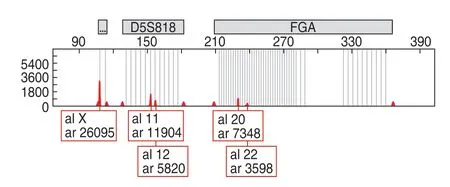
Fig.3 Alleles detected in the ARO cell line
Tumor growth and HE staining in mice
Tumor growth was observed in four out of 10 mice injected with the smoke particle rinse.All palpable masses were biopsied for morphological evaluation.HE staining showed abnormal nuclei and a rough cytoplasm (Fig.4).
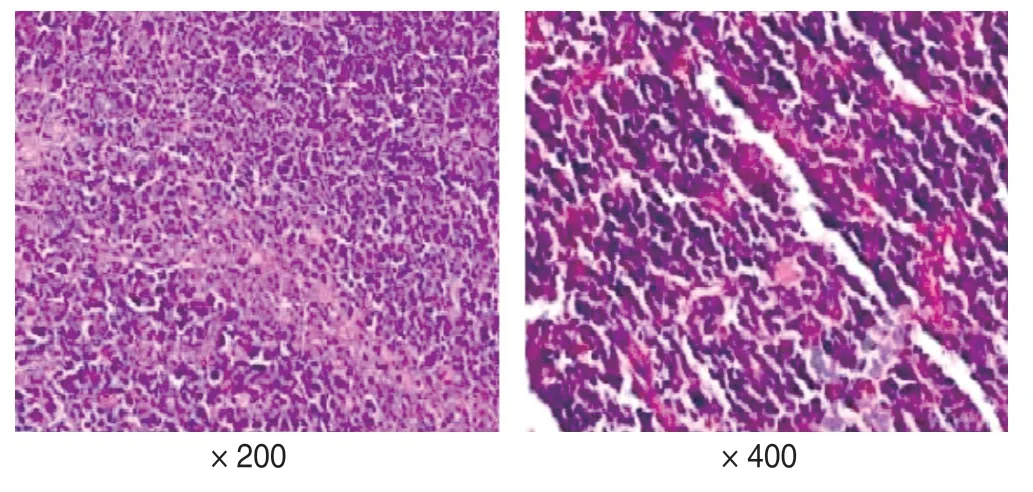
Fig.4 Hematoxylin and eosin staining of mouse tumor tissue
Discussion
More than 600 different organic compounds are contained in the smoke produced by instruments used in surgical procedures.Most of these compounds have adverse effects on human health.Long-term exposure to this polluted environment may induce the development of various diseases of the respiratory,digestive,reproductive,nervous,blood,and immune systems.Surgical smoke may also have bioactive substances,such as virus particles,active cell fragments,and DNA fragments.HIV can remain active for 14 days in surgical smoke and only becomes completely inactive after 28 days.
The working principle of the ultrasonic scalpel involves the conversion of electrical energy into mechanical energy through a special conversion device.The high-frequency ultrasonic vibration of the ultrasonic knife head can vaporize water in the contact tissues and cells,break the hydrogen bonds in proteins,and cut the tissue after solidification[8].Ultrasonic scalpels have fast and slow gears.The fast gear is mainly used for tissue cutting,and the slow gear is mainly used for hemostasis.Its application in laparoscopic surgery has obvious advantages,and it is the main surgical instrument used in laparoscopic surgery,especially for gastric and colorectal cancer,for which it is used in more than 95%of the cases[9].During high-temperature operation,the target cells are heated to the boiling point,resulting in membrane rupture and the dispersion of fine particles in the surrounding area.Ultrasonic scalpels use ultrasonic energy to destroy tissue through cavitation,and they produce a dense cloud of cell debris,which may contain living cells[10].The heat generated by the ultrasonic scalpel is the result of internal friction caused by highfrequency vibration (approximately 55 000 times/s).Hightemperature aerosols are more likely to carry infectious and active substances than low-temperature aerosols[11].The present study demonstrated that there may be viable malignant cells in the surgical smoke produced by ultrasonic scalpels.This suggests that malignant tumor cells can be atomized onto tumor-bearing tissues via the use of an ultrasonic scalpel,and to some extent,it explains the recurrence of tumors at sites distant from the tumor extraction site after laparoscopic resection[12].
There is evidence that live bacteria and viruses are present in surgical smoke.Capizzi and others[13]reported that 5 strains of coagulase-negativestaphylococcigrew after laser resurfacing,among the 13 strains of bacterial culture.Garden[14]detected complete viral DNA sequences in smoke collected during the laser treatment of human papilloma virus-infected verrucae.The infectivity of these particles was confirmed by inoculating them onto the skin of calves.It has been reported that a surgeon was infected with laryngeal papilloma after using a surgical laser to treat condyloma acuminata of the anus and genitalia[15].Although there are still disputes about the existence of living cells in surgical smoke,some studies have failed to screen out atomized cells in the peritoneal cavity during laparoscopic surgery.Other studies have shown that there are cell-sized fragments with intact morphology,but not viable cells,in surgical smoke.According to Johnsonet al[16],in the surgical smoke generated by an ultrasonic scalpel,there are almost no intact cells,and no living cells.Fletcher[17]found that melanoma cells survive in the smoke produced by the electric cauterization of mouse melanoma cells.Therefore,many researchers believe that living cells,especially malignant cells,which have greater vitality,may survive in surgical smoke.Previous studies have used surgical fumes inhaled directly through long tubes.However,in the present study,transwell membranes with a pore size smaller than the size of cells,were used to increase the number of cells collected.When surgical smoke passes through the membrane,the gas is collected by a vacuum pump,and cells larger than the pores are filtered out and collected.Because of this,cell collection may be more efficient in this study than that in the previous studies.
Even with the use of smoke extractors,operating room staff can usually detect the smell of burnt tissue when performing electrical dissection procedures.This indicates that the surgical smoke is not fully removed from the room.The direct resection of a tumor mass is rare,because surgeons usually dissect the tumor tissue along with normal tissue 5 cm from the edge of the tumor[18].However,owing to a distorted surgical field,an extensive malignant tumor,or surgical error,tumor masses may be directly removed.Therefore,it is necessary to control surgical smoke and use smoke extraction systems to protect the surgical team members and patients.At the same time,surgical fumes from the scalpel may contain viable tumor cells,and there is a theoretical risk of metastasis to anyone in close vicinity of the procedure.
In conclusion,this study found that there are viable tumor cells in the surgical smoke generated by ultrasonic scalpel dissection,and these cells have growth activity.Therefore,it is necessary to protect patients and medical staff from electrosurgical smoke.
Conflicts of interest
The authors indicated no potential conflicts of interest.
 Oncology and Translational Medicine2021年3期
Oncology and Translational Medicine2021年3期
- Oncology and Translational Medicine的其它文章
- Construction and validation of an immune-related lncRNA prognostic model for rectal adenocarcinomas*
- Antitumor and vascular effects of apatinib combined with chemotherapy in mice with non-small-cell lung cancer
- Diagnostic value of lncRNAs as potential biomarkers for oral squamous cell carcinoma diagnosis:a meta-analysis*
- Recombinant human vascular endostatin injection to synchronize craniospinal radiotherapy for the treatment of recurrent medulloblastoma in children:A retrospective clinical study*
- Seroprevalence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in patients with cancer and the impact of anti-tumor treatment on antibodies*
- Future of targeted therapy for gastrointestinal cancer:Claudin 18.2
