Central retinal artery occlusion in eosinophilic granulomatosis with polyangiitis (Churg-Strauss Syndrome): the first case report in South Korea
Jungyul Park, Up Huh, Hee-young Choi, Seunggeun Lee, Miyeun Han, Sungwoon Chung,Hyerim Kim
1Department of Ophthalmology, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan 49241, Republic of Korea 2Department of Thoracic and Cardiovascular Surgery, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan 49241,Republic of Korea
3Department of Rheumatology, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan 49241, Republic of Korea 4Department of Nephrology, Pusan National University School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan 49241, Republic of Korea
5Department of Laboratory Medicine, Pusan National University School of Medicine, Biomedical Research Institute,Pusan National University Hospital, Busan 49241, Republic of Korea
Dear Editor,
I am Dr. Jungyul Park from the Department of Ophthalmology, Pusan National University Hospital,Busan, Korea. I am writing to present a case of eosinophilic granulomatosis with polyangiitis (EGPA) with central retinal artery occlusion (CRAO). It provides important information about the relationship between ANCA and CRAO in a patient who was diagnosed with EGPA who had ophthalmic symptoms. We believe that our study makes a significant contribution to the literature because to our knowledge, the literature of EGPA with CRAO are rare worldwide and this is even the first case of EGPA with CRAO in Republic of Korea.Allergic granulomatosis, also known as EGPA, is closely related to systemic vasculitis[1]. This autoimmune vasculitis is associated with eosinophilia, previous or existing airway allergic hypersensitivity, and positive anti‐neutrophil cytoplasmic antibodies (ANCA) titers[2]. It is considered a Th2‐mediated disease with CD4 T cells, resident endothelial and epithelial cells promoting allergic and eosinophilic reactions[3].
EGPA usually affects medium and small blood vessels,and the most commonly affected organs include the lungs,gastrointestinal tract, skin, and heart. It occasionally shows orbital or ophthalmic involvement, and Takanashiet al[4]classified ocular manifestations in EGPA into ischemic vasculitis and inflammatory pseudotumor types. However, only few cases of ophthalmic involvement including CRAO have been reported[4‐5]. CRAO in EGPA is classified as the ischemic vasculitis type and it is associated with a positive ANCA status and sudden onset of vision loss.
Herein, we report a patient with EGPA who developed CRAO with sudden vision loss. To our knowledge, this is the first report of EGPA associated CRAO in the South Korean population and it provides important information about the relationship between ANCA and CRAO in a patient who was diagnosed with EGPA who had ophthalmic symptoms.
Ethical ApprovalThe study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the institutional review board of our Hospital(IRB No.H‐1905‐004‐079). Informed consent for publication was obtained from the family of the patient in this case report,as potentially identifying information may be included in this article.
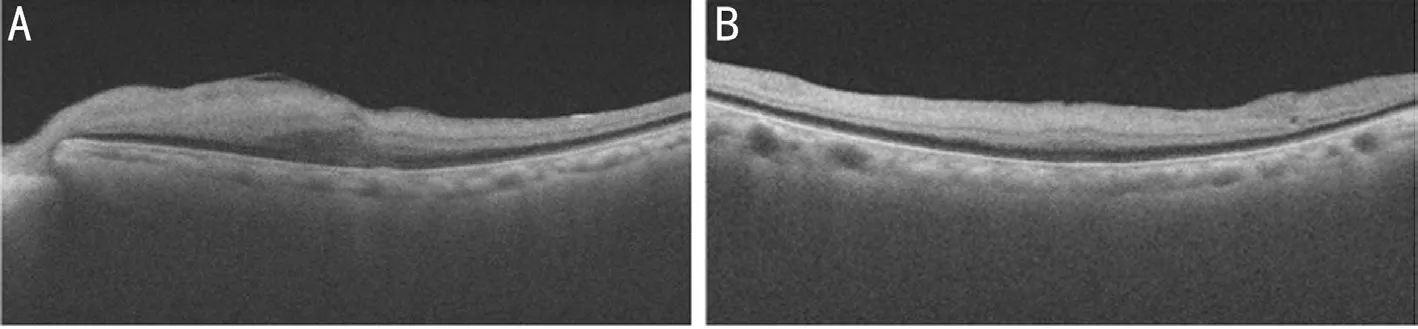
Figure 1 Optical coherence tomography shows disfiguring and edematous changes in the entire retinal layer on her left eye A: Vertical image; B: Horizontal image.
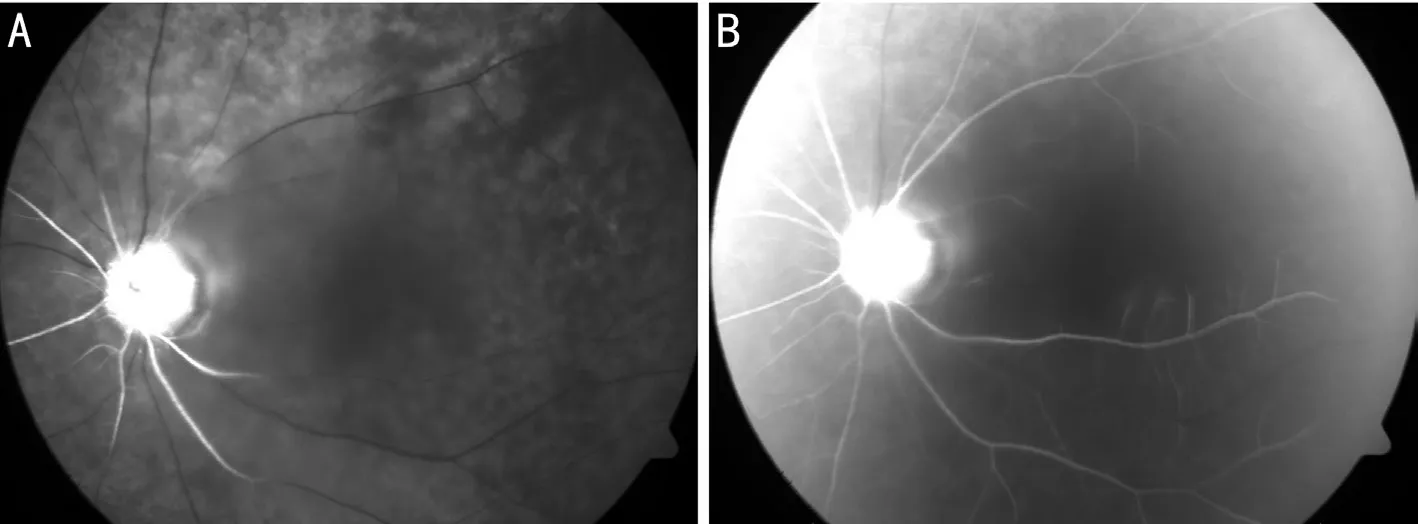
Figure 2 Fundus fluorescent angiography showed a multiple filling delay of the retinal artery and choroidal filling defect (A); and late filling of the cilioretinal artery was observed at >30s (B).
A 69‐year‐old woman was hospitalized with one‐month history of tingling sensation on both legs and left hand and generalized weakness. She had no previously diagnosed disease. Spine magnetic resonance imaging (MRI) revealed a bulging disc in C4‐5 and L4‐5. Right saphenofemoral junction and femoral vein,left saphenofemoral junction and saphenopopliteal junction reflux were observed on Doppler ultrasound of the lower limb.
The initial blood test revealed elevated white blood cell count(15 190 cells/μL), C‐reactive protein (11.32 mg/dL), erythrocyte sedimentation rate (ESR; 120 mm/h), and eosinophils (13.6%).Estimated glomerular filtration rate was 36.7 mL/min·1.73 m2and hyponatremia (128.7 mmol/L) was present. A low‐grade fever(37.5℃) was observed every morning on the vital signs chart after hospitalization; hypertension was also confirmed. Chest computed tomography (CT), abdominal CT, and transthoracic echocardiography were performed. Sensory abnormalities were assessed using nerve conduction velocity test to diagnose peripheral nerve abnormalities. Abdominal CT, transthoracic echocardiography, and nerve conduction velocity test were not found abnormal.
On chest CT, multifocal centrilobular nodules were observed in both lungs. Bronchopneumonia, parasitic infection, and EGPA were suspected. Because community acquired pneumonia was possible, levofloxacin was used as an empirical antibiotic;toxocariasis Ab IgG and ANCA quantitative test were additionally performed. Toxocariasis Ab IgG was identified as positive and albendazole 400 mgb.i.d.for 5d was prescribed.Sputum induction test showed positive bronchial asthma and airway eosinophilic inflammation. Myeloperoxidase antibody(9.1 U/mL) was confirmed using ANCA quantitative test. In paranasal sinuses Water’s view, chronic maxillary sinusitis was diagnosed.
During evaluation, the patient complained of decreased visual acuity in the left eye. On initial examination in the ophthalmology department, there was no abnormal findings on ophthalmic examination. The fundus examination of her left eye showed a whitish retinal discoloration with marked pallor on the disc and cherry red spot in the macular region. The ophthalmic computed tomography (OCT) showed a disfiguring and edematous change in the entire retinal layer of her left eye(Figure 1). Fundus fluorescent angiography showed a filling delay of the retinal artery. Late filling of the cilioretinal artery was observed at >30s, and a spotted appearance with choroid perfusion defect (Figure 2). No leakage secondary to vasculitis from the posterior pole retinal vessels (both arteries and veins)or optic disc was observed and eventually CRAO on the left eye was diagnosed.
Brain MRI, carotid artery Doppler ultrasonography, trans‐esophageal echocardiography, and Holter monitoring were performed to identify the cause of the central retinal artery occlusion; however, no evidence of thromboembolism was found. A biopsy of the left kidney was performed to confirm the EGPA. The biopsy showed Pauci‐immune and ANCA‐mediated crescentic glomerulonephritis (Figure 3).
Cyclophosphamide pulse therapy with steroid (methylprednisolone 60 mgq.d.) was administered because EGPA complicated with CRAO was diagnosed and kidney involvement was advanced.A month after treatment, there was marked pallor of the retina with ischemic change on her optic disc. On the OCT of her left eye, the entire retinal layer showed atrophic change on the macular region and cystic change around the macular area(Figure 4). During the 6‐month follow‐up period, the final vision on her left eye was light perception and was not improved even after steroid pulse and immunosuppressant therapy.

Figure 3 The microscopic findings Up to 25 glomeruli are present in this biopsy, of which 8 (32%) show global sclerosis. In the remaining glomeruli, segmental loop necrosis and fibrin deposits are focally seen. Eleven glomeruli (44%) exhibit cellular or fibrocellular crescents.

Figure 4 Fundus photograph shows marked pallor of the retina with ischemic change on her optic disc (A); On the optical coherence tomography of her left eye, the entire retinal layer showed atrophic change on the macular region and cystic change around the macular area (B; vertical image and horizontal image).
EGPA diagnosis, per the American College of Rheumatology,requires the presence of ≥4 of the following 6 conditions:asthma, eosinophilia of >10%, neuropathy, migratory or transient pulmonary opacities, abnormalities of paranasal sinuses, and extravascular eosinophils on biopsy[6]. Herein,EGPA was confirmed with the presence of all the 6 criteria.EGPA usually manifests in 3 phases. The first phase is the prodromal asthmatic and allergic phase, usually occurring in the second and third decades of life. The second eosinophilic phase includes peripheral blood eosinophilia and eosinophilic infiltration of multiple organs. This typically affects the lungs and the gastrointestinal tract, presenting as pulmonary opacities, asthma, or gastroenteritis. The third and final phase is the life‐threatening vasculitic phase, involving small‐ and medium‐sized vessels[5]. During the third phase, patients with EGPA may experience fever, weight loss, and lack of energy[7].This case corresponds to the third phase.
The data on epidemiology is limited; however, based on several reports, the prevalence and annual incidence of EGPA is 2‐22 and 0.5‐3.7 per million, respectively. Regarding cases with ophthalmic manifestations, from complete review of the English literature, only 46 cases were reported[5]. The cases were divided into 2 groups: idiopathic orbital inflammation presentation and ischemic vasculitis presentation. Twenty‐five patients had the ischemic vasculitis type, 20 patients had the idiopathic orbital inflammation type, and 1 patient had both types. The manifestations of the orbital inflammation type include conjunctival nodules, orbital myositis, orbital inflammatory syndrome, or dacryoadenitis. In many of these cases, aside from a background history of asthma or rhinitis,the orbital disease was the first symptom[4]. Ischemic vasculitis type is usually unilateral, tends to older age than inflammatory type, is a more aggressive disease, and patients often have a poor visual outcome. Interestingly, some patients who eventually had permanent vision loss experienced prodrome such as transient amaurosis prior to symptoms onset. The manifestations of the ischemic vasculitis type include retinal artery and vein occlusions, ischemic optic neuropathy, and retinal vasculitis or retinal edema[5]. Herein, the patient had CRAO with ischemic vasculitis type EGPA; it was unilateral,of sudden onset, aggressively progressed, and eventually had a poor visual outcome of light perception on her left eye.However, she had no history of amaurosis or any prodromal symptoms. Perinuclear anti‐neutrophil cytoplasmic antibodies(P‐ANCA) was positive in this patient and she had a treatment of high dose steroid of 60 mg/d and immunosuppressant cyclophosphamide pulse therapy 2d after her symptoms onset;however her final vision and retinal ischemia did not improve.About 30%‐40% of EGPA patients are known to be ANCA positive[8]. In ocular cases, Akellaet al[5]reported similar rates of ANCA positivity of 33.3%. The most common subset is P‐ANCA; ANCA‐positivity should not be used to make a definitive diagnosis. However, ANCA‐positive patients are more likely to present with the ischemic vasculitis type and may be at risk for sudden visual loss; therefore,prophylactic steroid therapy may be indicated[4]. From the recent literature, regarding the ischemic vasculitis type, out of 8 patients who received a combination therapy of steroids and cyclophosphamide, 4 patients showed improvement in vision[5]. Authors also started combination therapy of steroids and cyclophosphamide pulse therapy as soon as she was diagnosed with EGPA based on the kidney biopsy; however, it was commenced 2d after the onset of symptoms of CRAO; her final visual acuity 1mo later was light perception. Almost all CRAO with EGPA cases eventually show poor visual outcome;the ischemic vasculitis‐type ophthalmic presentations have a less effective response to steroids. However, interestingly,some authors have reported a good visual recovery after an early high dose intravenous steroid therapy[9]. They reported that steroid pulse therapy before the occurrence of CRAO may be effective for CRAO with EGPA patients. This might indicate that ischemic vasculitis‐type benefits from aggressive intravenous steroid therapy.
Based on these reports, it is very important to enquire of prodromal symptoms of amaurosis and blurred vision and consider a diagnosis of EGPA when approaching a patient with CRAO; to commence early treatment and give the patient an opportunity of having a good visual outcome. Therefore,since intensive treatment should be administered as early as possible to improve the prognosis of vision, rheumatologists and ophthalmologists should be aware of the presence of EGPA‐associated CRAO without overlooking any prodrome.Ophthalmologists should consider EGPA as a differential diagnosis for CRAO patients. EGPA has a 50% risk of death within 3 months when it is not treated and diagnosed properly;therefore, early diagnosis is key to improving the survival rate from 70% to 90% at 5y[10].
ACKNOWLEDGEMENTS
Conflicts of Interest:Park J,None;Huh U,None;Choi H,None;Lee S,None;Han M,None;Chung S,None;Kim H,None.
 International Journal of Ophthalmology2021年6期
International Journal of Ophthalmology2021年6期
- International Journal of Ophthalmology的其它文章
- A decrease in macular microvascular perfusion after retinal detachment repair with silicone oil
- Surgical outcomes in acute dacryocystitis patients undergoing endonasal endoscopic dacryocystorhinostomy with or without silicone tube intubation
- Dr. Father Wacław Szuniewicz, a forgotten pioneer in refractive surgery and his work in China
- Deterioration of Avellino corneal dystrophy in a Chinese family after LASlK
- A mutated CRYGD associated with congenital coralliform cataracts in two Chinese pedigrees
- Autophagy dysregulation mediates the damage of high glucose to retinal pigment epithelium cells
