A decrease in macular microvascular perfusion after retinal detachment repair with silicone oil
Wei Fang, Jing Zhai, Jian-Bo Mao, Hai-Dong Li, Zhen-Bin Qian, Chao-Qiao Chen, Jia-Hao Xu,Li-Jun Shen, Yi-Qi Chen
The Eye Hospital of Wenzhou Medical University, School of Opthalmology & Optometry, WMU, Zhejiang Eye Hospital,Hangzhou 310000, Zhejiang Province, China
Abstract
● KEYWORDS: macular perfusion; vessel density; silicone oil; optical coherence tomography angiography; retinal detachment
INTRODUCTION
In advent of medical silicone oil (SO), many complicated vitreoretinal cases were successfully treated with vitrectomy and SO tamponade, such as severe proliferative vitreoretinopathy (PVR), retinal detachment with large tears,choroidal detachment or macular holeetc. However, elongated tamponade of SO could do harm to many intraocular or extraocular tissues[1‐5]. After retinal detachment repair and SO tamponade, retinal and choroidal tissues have proved to be damaged by high resolution optical coherence tomography(OCT)[1,3,6‐8], but it remains unclear whether retinal vascular perfusion would be affected under this circumstance. Optical coherence tomography angiography (OCTA) is a novel non‐invasive technique that can depict retinal microcirculation and is already widely used in detecting macular perfusion,optic papillary perfusion and choroidal circulation[9‐15]. So far, several retrospective studies showed that after successful retinal reattachment with SO or long‐standing gas tamponade,superficial or deep retinal circulation obviously reduced when compared to the fellow eye or healthy controls[16‐18].However, as we know many factors, like retinal detachment,surgical procedure or tamponade substance texture, may contribute to the retinal damage process, so it is difficult to extrapolate whether SO is independently involved in this process if we only compare postoperative retinal changes to the intact contralateral eye. During the past years, because of the shortage of longstanding gas in our institute, many retinal detachment repair surgeries were successfully completed with only air tamponade. Empirically, this short‐absorbed tamponade substance could to maximally extent lessen the retinal damage, therefore it is a more ideal control for this comparison research. So, in this study we try to observe the SO’s effect on retinal microcirculation over air tamponade.
Usually in retinal detachment cases, preoperative retinal vasculature could not be evaluated precisely in the affected eye. So, in this prospective observational case‐control study,we aimed to investigate the probable toxicity of SO on macular perfusion, through comparing OCTA findings between the SO and air tamponade after retinal detachment repair surgery.Two postoperative visits were planed (1 and 3mo). Meanwhile,retinal thickness changes were also evaluated simultaneously.
SUBJECTS AND METHODS
Ethical ApprovalThe study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of The Eye Hospital of Wenzhou Medical University (No.2019‐220‐K‐197). All patients had signed a written consent document in this study.
Patients SelectionPatients diagnosed with primary macular off rhegmatogenous retinal detachment undergoing successful retinal repair surgery (defined as complete anatomical retinal reattachment without any postoperative complication or subretinal fluid) were selected between January 2019 and April 2020. Inclusion criteria: 1) age from 18 to 60 years old; 2) macular detachment demonstrated by OCT, ultrasonic scans or intraoperative findings; 3) retinal detachment repair was completed by vitrectomy with SO or air tamponade.Exclusion criteria: 1) PVR severer than C2 (the classification of the Retina Society Terminology Committee in 1983);2) perfluorocarbon liquid introduced intraoperatively; 3)recurrent retinal detachment; 4) chronic retinal detachment defined as previously published; 5) macular hole, epimacular membrane, macular degeneration; 6) postoperative high intraocular pressure (>21 mm Hg) more than 1mo; 7) trauma or other intraocular surgical history, intraocular anti‐vascular endothelial growth factor injection; 8) pathological myopia;9) hypertension, diabetic mellitus or other vasculopathies that would affect retinal circulation. Patients with SO tamponade were classified in the study group while those with air tamponade were in the control group.
Basic information of the patients included: age, sex, axis length, macular‐off duration, best corrected vision, detached extension, detached location, PVR, surgery type. Patients undergoing pars plana vitrectomy (PPV) with simultaneous or subsequent phacoemulsification and intraocular lens (IOL)implantation were classified as PPV+Phaco+IOL subgroup,otherwise they were labeled as PPV subgroup. Retinal detached location was defined as superior or inferior area according to the major detached area involved. One case with 4 quadrants detached was classified in the inferior subgroup due to much higher elevation and proliferation of the inferior retina.
Surgical ProcedureAll patients were under retrobulbar anesthesia and a standard three ports 23G PPV was performed(Constellation, Alcon Laboratories, Inc., TX, USA). After completely removal of the core and peripheral vitreous body,gas‐fluid exchange was performed to reattach the retina,followed by laser endocogulation around retinal tears and degenerative regions. Vitreous cavity was left with sterile air tamponade, or with SO jell (5000CS, Carl Zeiss Meditec AG, Jena, Germany) injection, depending on retinal tear size,location, degree of PVR, and detached extensionetc. The 3 scleral incisions were sutured with 8‐0 absorbable Vicryl to maintain a normal eye pressure. Phacoemulsification and IOL implantation were performed in selected cases depending on severity of lens capacity.
OCTA Examination and Measures SelectedOCTA images were acquired 1 and 3mo after surgery. A scanning area of 3×3 mm2was performed automatically centered on the fovea using RTVue XR Avanti device (Optovue Inc., Fremont, CA, USA).The grid was composed of two circles: an inner circle with a diameter of 1 mm and an outer circle with a diameter of 3 mm.The parafoveal region was defined as the ring zone between the inner and outer circle. Automated segmentation of the full thickness retinal layer was performed by built‐in software program to generate en face projection images. The full retinal thickness was defined as the distance between the internal limiting membrane and the retinal pigment epithelial cell. The segmentations of all examination were manually rechecked before any measurement was performed. The parafoveal perfusion parameters, including the superficial vessel density(PFSVD) and deep vessel density (PFDVD) were analyzed.Parafoveal full retinal thickness (PFRT) was simultaneous calculated automatically using the system’s software. Those measures were subgrouped in four quadrants as temporal,superior, nasal, inferior area. Tropicamide/phenylephrine (0.4%Mydrin P; Santan Pharmaceutical Co., Ltd., Osaka, Japan) was used to dilate the pupil 30min before examination. Images with scanning quality ≥5/10 were chosen in this study.
Statistical AnalysisThe Shapiro‐Wilk test (W score) was used to verify the normal distribution of the quantitative data. Student’st‐test or Wilcoxon two sample test was used to compare the differences in variables between the study and control group. Pairedttest was used to compare the measures between the first and second visit. Chi‐square or Fischer’s exact test was used to compare the categorial data.All quantitative data were expressed as mean±SD, and all tests were two‐sided. Statistical significant level was accepted atP<0.05. All analyses were performed using SAS 9.2 (SAS Institution Inc., Cary, NC, USA).
RESULTS
Patients’ Demographics and Ocular CharacteristicsThirty‐seven cases of patients undergoing rhegmatogenous retinal detachment repair with vitrectomy were preliminary screened in this study. After surgery, two cases had recurrent retinal detachment and three cases were complicated with epimacular membrane. One case had higher intraocular pressure longer than one month, while two cases lost follow up. So, 29 patients(29 eyes, 12 left, 17 right) were finally enrolled in this study.Thirteen case were males and 16 were females. Twenty cases had SO tamponade while 9 cases were with air tamponade.Patients’ demographics were shown in Table 1. Most clinical variables were evenly distributed in the study and control group except the factor detached extension.
Quantitative Analysis of OCTA DataAt the first visiting point, compared with the air group, PFSVD significantly decreased in the SO group, especially in the superior quadrant or superior‐hemi area. However, PFDVD in all quadrants had no difference between two groups. At the 3 months’visiting point, all quadrants of PFSVD decreased significantly in the SO group, but PFDVD remained no different in the two groups. All quadrants of PFRT in the SO group reduced significantly at both visiting points, while foveal avascular zone (FAZ) area showed no difference between the two groups(Table 2).
Regarding the recovery process, in the air group all areas of PFSVD showed significantly improving from the first visit to the second visit postoperatively, but PFRT, FAZ area, and almost all quadrants of PFDVD showed no changes between the two visits (Table 2). On the contrary, in the SO group, all of those measures showed no obvious changes between the two visiting points.
DISCUSSION
In this study we found that after SO tamponade, retinal superficial vessel density decreased at both 1 and 3 months’visits, when compared to those with air tamponade in the control cases, especially in the superior area. But FAZ and deep vessel density showed no difference between the two groups during the 3 months’ follow up period. This result was similar with Maet al’s[17]research, in which the authors focused on 7 cases of retinal detachment repair with vitrectomy and SO tamponade whose postoperative visual acuity was more than two lines lost unexplainably. They found that in those casessuperficial vessel density decreased and this deterioration was parallel with ganglion cell complex layer thickness, when comparing them to the contralateral eye. However, another study by Leeet al[16]only deep vessel density decreased but without any superficial vessel changes. The authors compared the macular perfusion status of a group of 38 patients, who had undergone SO tamponade (mean 4mo) and removal (mean 7mo follow up), with the contralateral eye. In our opinion,in Leeet al’s[16]cross‐sectional research it might not truly reflect the macular condition under SO tamponade, for the patients had received consecutive vitrectomy, SO implant and extraction procedure, which might cause the discrepancy. By contrast, as we know, intraocular air could be mostly absorbed in one week, so we compare the macular perfusion status of SO tamponade simultaneously to the cases with air tamponade,which could to maximal degree exclude any other bias factors such as retinal detachment, vitrectomy procedure and the probable effect of longstanding intraocular gas. Therefore, in this study, at both visiting points, the loss of superficial vessel density under SO tamponade was probably confirmed.
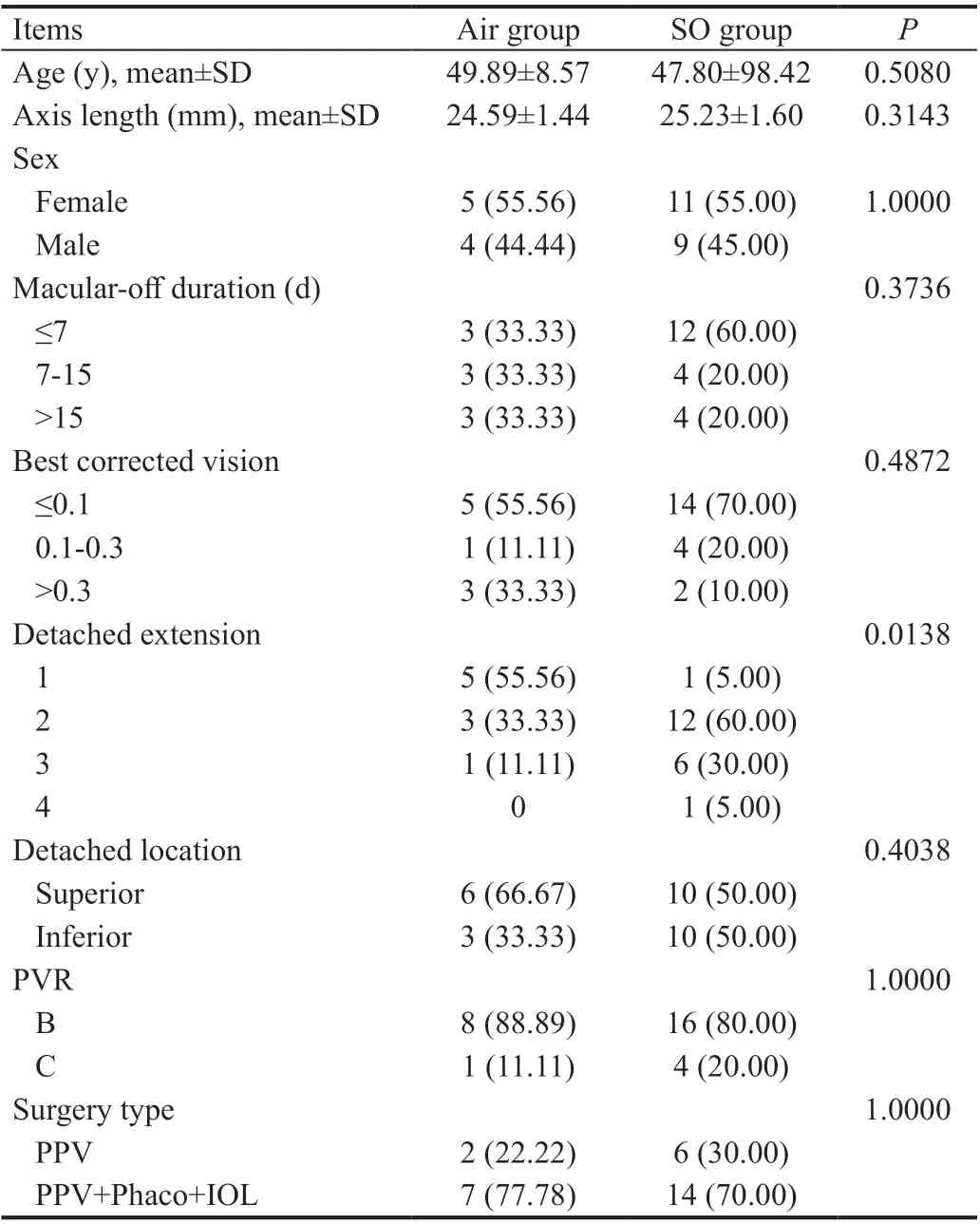
Table 1 Patients’ demographics and ocular characteristics in the air and SO group n (%)
When comparing the first and second follow up points, in terms of the retinal recovery process, we found that in the SO group, all macular features including vessel density and retinal thickness had no obvious changes, which was in accordance
with Xianget al[18]. On the contrary, macular superficial vessel density improved significantly in the air group in the two months’ period. Several other studies focusing on patients undergoing retinal reattachment surgery but without SO tamponade also showed retinal vessel density improving over time. Those findings would to some degree support the idea of SO’s toxicity on the retinal superficial vascular structures.

Table 2 Parafoveal perfusion evaluation between the air and SO group in 1 and 3mo
Although retinal detachment extension was unevenly distributed in the two groups (P=0.0138) and correlated with the deep vessel density at the second visit in SO group(r=‐0.4589,P=0.0418, Spearman correlation test, data not supplemented), it was not significantly correlated with superficial density at both visits or deep vessel density at first visit in both groups (data not supplemented). Meanwhile, we found no deep vessel density difference in the two groups at both visits. Furthermore, retinal detached location showed no differently distribution (66.67% superiorly located in the air groupvs50% in the SO group,P=0.4038) in the two groups.So, we majorly ascribed the superior area vessel density decreasing after retinal repair surgery to the process of SO tamponade. As Leeet al[16]reported, SO tamponade duration was the main independent risk factor for reduction of vessel density, not any other factors like age, detached extension,PVR, lens status, operation time or SO volume injected.
It is still controversial to clarify the mechanism of SO’s effects on retinal vascular structures and nerve fibers. As we know,SO has lower specific gravity than aqueous humors in vitreous cavity, so SO exerts pressure on the retina in sitting, lateral and prone positions, even more in the superior part. In this study, we inferred that SO could compress the inner retina to damage superficial vascular structures (especially in superior part), and decrease the full retinal thickness, but the specific mechanism still needs further investigation. Other explanations included slight to moderate immunologic inflammation of SO microbubble in different area as proved by Wickhamet al[19], and the ions exchange defunction of the Müller cells between retina and vitreous fluid by the SO, which constricts the little space between these two interfaces, reportedin vitroexperiments[20].
The first limit in this study was a relatively small sample of cases, which weakened the evidence of the research. Second,we did not specify the retinal thickness segmentation, so it was unable to evaluate the correlations between the vessel density and retinal thickness. Third, it would be better to take into account the macular vessel density changes after SO extraction. So, more advanced researches should be carried out in the future.
In conclusion, after retinal detachment surgery with vitrectomy and SO tamponade, superficial macular perfusion and full retinal thickness could decrease obviously when compared to air tamponade. This reduction process could persist throughout the tamponade period.
ACKNOWLEDGEMENTS
Foundation:Supported by Wenzhou Municipal Science and Technology Bureau (No.Y20180730).
Conflicts of Interest: Fang W,None;Zhai J,None;Mao JB,None;Li HD,None;Qian ZB,None;Chen CQ,None;Xu JH,None;Shen LJ,None;Chen YQ,None.
 International Journal of Ophthalmology2021年6期
International Journal of Ophthalmology2021年6期
- International Journal of Ophthalmology的其它文章
- Role of bevacizumab intraocular injection in the management of neovascular glaucoma
- Surgical outcomes in acute dacryocystitis patients undergoing endonasal endoscopic dacryocystorhinostomy with or without silicone tube intubation
- Dr. Father Wacław Szuniewicz, a forgotten pioneer in refractive surgery and his work in China
- Deterioration of Avellino corneal dystrophy in a Chinese family after LASlK
- A mutated CRYGD associated with congenital coralliform cataracts in two Chinese pedigrees
- Autophagy dysregulation mediates the damage of high glucose to retinal pigment epithelium cells
