Triamcinolone as an adjunct to the combination of anti-VEGF for the management of diabetic macular edema
Ying-Ying Yu, Yong Cheng, Li-Bin Chang, Hui-Ka Xia,3, Xiao-Xin Li,4
1Department of Ophthalmology, Peking University People’s Hospital, Eye diseases and Optometry Institute, Beijing Key Laboratory of Diagnosis and Therapy of Retinal and Choroid Diseases, College of Optometry, Peking University Health Science Center, Beijing 100044, China
2Department of Ophthalmology, Beijing Jingmei Group General Hospital, Beijing 102300, China
3Department of Ophthalmology, Hebei General Hospital,Shijiazhuang 050051, Hebei Province, China
4Xiamen Eye Center of Xiamen University, Xiamen 361003,Fujian Province, China
Abstract
● KEYWORDS: diabetic macular edema; intravitreal triamcinolone; anti-vascular endothelial growth factor
INTRODUCTION
According to statistics, diabetes mellitus (DM) has accounted for large proportions among Chinese adults due to the rapid change in lifestyle. It was estimated from the data published in 2017 among 18y older adults in China that DM prevalence reached 10.9% in the population in 2013,which is the highest number of DM cases in the world[1]. There is a direct proportional relationship between the number of patients with diabetic retinopathy (DR) and the incidence of DM. As one of the typical pathological features of DR in DM,diabetic macular edema (DME) often cause visual impairment,which seriously declines the patients’ living quality.
In clinical, grid/focal laser treatment or drug treatment of using of corticosteroidsviaan intravitreal route or posterior sub‐tenon space were normally used to treat DME. Recently, anti‐vascular endothelial growth factor (VEGF) was considered as the best choice for treating DME and vision impairment[2‐4].Anti‐VEGFs resulted in better best‐corrected visual acuity(BCVA) than laser therapy. Nonetheless, we have to admit that anti‐VEGF agents need be inevitably administered again and again to ensure the initial anatomical and functional success.Because of the long course of disease, every patient must get regular injections every year, which will cause high treatment costs. Thus, studies on the cost‐effectiveness of these agents were extensive in the recent year[5‐7]. In contrast to western countries, anti‐VEGF treatment is currently a heavy burden for DME patients in China. Anti‐VEGF is not yet accepted by any insurance, medicare or commercial. Consequently, a new adjunct therapy has been explored to reduce the frequency of injections and improve the treatment compliance and benefit of anti‐VEGF treatment in DME patients. Based on the RESTORE and REVEAL study[2‐3], combination therapy has been shown to be effective so far. Triamcinolone is currently the most common drug for treating DME in China. On the basis of these findings, this study was aimed to evaluate the clinical effects of the combination of intravitreal triamcinolone(IVTA) and anti‐VEGF for DME treatment in China.
SUBJECTS AND METHODS
Ethical ApprovalAll patients gave informed consent. The study obtained Institutional Review Board approval and adhered to the tenets of the Declaration of Helsinki.
Data were retrospectively collected from the Ophthalmology Department of Peking University People’s Hospital and the Eye Department of Beijing Jingmei Group General Hospital.
A total of 51 patients with pseudophakic eyes who were over 18 years old with type 2 DM (on the basis of the guideline of World Health Organization or American Diabetes Association)with glycosylated hemoglobin levels of 10% or less and visual impairment causing by DME were enrolled in this study from two sites. The inclusion criteria were 1) persistent DME after intravitreal conbercept (IVC) or IVTA; 2) persistent DME after vitrectomy; 3) DME after panretinal photocoagulation (PRP);4) follow‐up for more than 12mo. The exclusion criteria were 1) traction DME; 2) foveal fibrosis; 3) uncontrolled glaucoma in either eye. Participants were divided two groups based on the therapeutic method: IVC combined with focal laser (24 eyes) and IVC combined with focal laser and IVTA (27 eyes).Two groups received IVC first, then focal laser, triamcinolone or IVC were administered as needed. Laser treatment always performed after IVC or IVTA, and the choice of IVC or IVTA depended on the patients. IVTA was also chosen for patients with a poor response to IVC.
In the treatment induction phase, 0.5 mg conbercept (0.5 mg in 0.05 mL) were used for the first injection. Thereafter,patients were evaluated each month whether they need additional injections of conbercept in above mentioned dose or triamcinolone (1 mg in 0.05 mL) in a PRN regimen when central retinal thickness (CRT) was ≥300 μm. On the basis of fluorescein angiography (FA) results, patients may be given the short pulse focal/grid laser photocoagulation 1wk after the initial injection according to the improved Early Treatment Diabetic Retinopathy Study (ETDRS) coagulation guidelines:1) leaking microaneurysms caused by retinal thickening in the area distance between 500 and 3000 microns from the macula’s centre were all directly treated (but not within 500 microns of disc); 2) area with intraretinal microvascular abnormality (IRMA) within macular were treated in a grid pattern; 3) microaneurysms were treated until color darkened;4) the duration was 0.1s; 5) the burn size was 50‐100 microns.BCVA, CRT, the required number of IVCs, and the mean costs of treatment burden and safety were compared over 12mo. The safety assessment included the general and serious adverse events (AEs and SAEs), eye examinations, and intraocular pressure (IOP) changes, vital signs, and laboratory analyses during the period.
Statistical AnalysisSPSS version 18.0 for Windows software (SPSS, Chicago, IL, USA) was used for statistical analysis. If there was missing data, we used the method called a last observation carried forward (LOCF) to fit them.The description of continuous variables is expressed by the mean±standard deviation or median and interquartile range.Numbers and percentages are chosen for describing categorical variables. The differences in BCVA and CRT between these two groups during the 12‐month period were analysed by ANOVA test. Pairedt‐tests or the Mann‐WhitneyUtest were used for continuous variables, and the Chi‐square test or Fisher’s exact test were used for classification analysis. The statistically significantPvalue was artificially set at 0.05.
RESULTS
Patient DemographicsTotally, 51 participants chosen in two hospitals were assigned to perform IVC combined with focal laser (n=24) or IVC combined with focal laser and IVTA(n=27). The included participants’ baseline characteristics are summed up in Table 1.
Efficacy
Best-corrected visual acuityDuring the assessment period,IVC combined with focal laser and IVTA (conbercept +laser+triamcinolone, 5.20±1.28 letters) was superior to IVC combined with focal laser (conbercept +laser, 2.71±1.54 letters) with a significant difference in BCVA (P< 0.001; Figure 1A; Table 2). During the first six months, the mean change in BCVA improved significantly with IVC combined with focal laser and IVTA versus IVC combined with focal laser(5.93±3.63 lettersvs2.27±2.72 letters;P<0.01; Figure 1B). From baseline to month 12, the mean change in BCVA letter score increased significantly with IVC combined with focal laser and IVTA versus IVC combined with focal laser (6.65±3.64 lettersvs3.79±2.61 letters;P<0.05; Figure 1B). At month 6, the rates of participants gain more than 10 BCVA letters was 16.67%in the group of performing IVC combined with focal laser treatment and 33.33% in the group of combination treatment(Figure 1C). Similarly, at the final month, the rates of subjects receiving more than 10 BCVA letters was 20.83% and 37.04%in the IVC combined with focal laser and IVC combined with focal laser and IVTA arms, respectively (Figure 1C; Table 2).No significant difference exists in these two groups.

Figure 1 BCVA’s change, CRT’s change and cost of treatment burden between two groups A: Mean BCVA’s change during the 12‐month period; B: Mean BCVA’s change at months 6 and 12; C: The rates of participants gaining more than 10 BCVA letters at months 6 and 12; D:Mean CRT’s change at months 6 and 12; E: Mean cost of treatment burden for 12mo. aP<0.05, bP<0.01, cP<0.001, paired t‐tests; dP<0.01,ANOVA test.
Central retinal thicknessA greater decrease of CRT was observed in the IVC combined with focal laser and IVTA arm compared with that in the IVC combined with focal laser arm at all assessed time points. In the IVC combined with focal laser and IVTA arm, a plummet in CRT was seen in the month 1 to month 3, and the decrease was kept until the end of the period (Figure 2). At the sixth month, the mean CRT reduced by 262.45±80.61 μm in the IVC combined with focal laser and IVTA arm compared with 102.63±107.80 μm in the IVC combined with focal laser arm (P<0.01; Figure 1D). Similarly,the observed mean CRT from baseline at month 12 decreased by 245.9±93.51 μm in the IVC combined with focal laser and IVTA arm compared with 98.45±139.58 μm in the IVC combined with focal laser arm (P<0.01; Figure 1D; Table 2).
Treatment with Conbercept Injections and Costs of Treatment BurdenThe mean number of focal laser treatments was 2.41±1.05 and 1.25±0.44 in the IVC combined with focal laser and IVC combined with focal laser and IVTA arms, respectively. The mean number of conbercept treatments administered was 6.45±4.3 in the IVC combined with focal laser arm and 1.25±0.44 in the IVC combined with focal laser and IVTA arm. The ratio of injections of conbercept to triamcinolone was nearly 1:1. The mean cost of treatment burden for 12mo was $6247.44±4069.18 in the IVC combined with focal laser arm and $1679.19±542.73 in the IVC combined with focal laser and IVTA arm, with a statistically significant difference (P<0.001; Figure 1E).

Figure 2 Mean CRT’s change during the 12-month period.
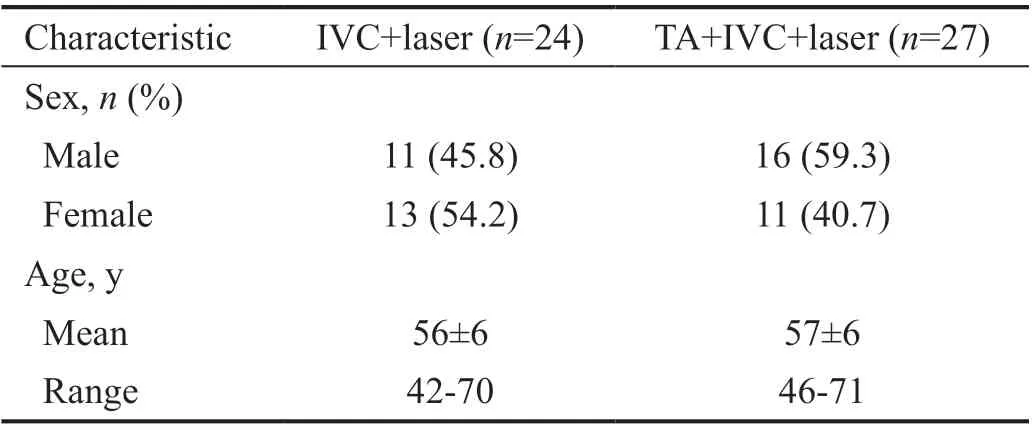
Table 1 Baseline characteristics of the participants
SafetyDuring the period of this study, there was no observed ocular AEs among the participants except for occasional minor subconjunctival hemorrhage. There was no significant difference in these two treatments in IOP, vital signs, or laboratory analyses.
DISCUSSION
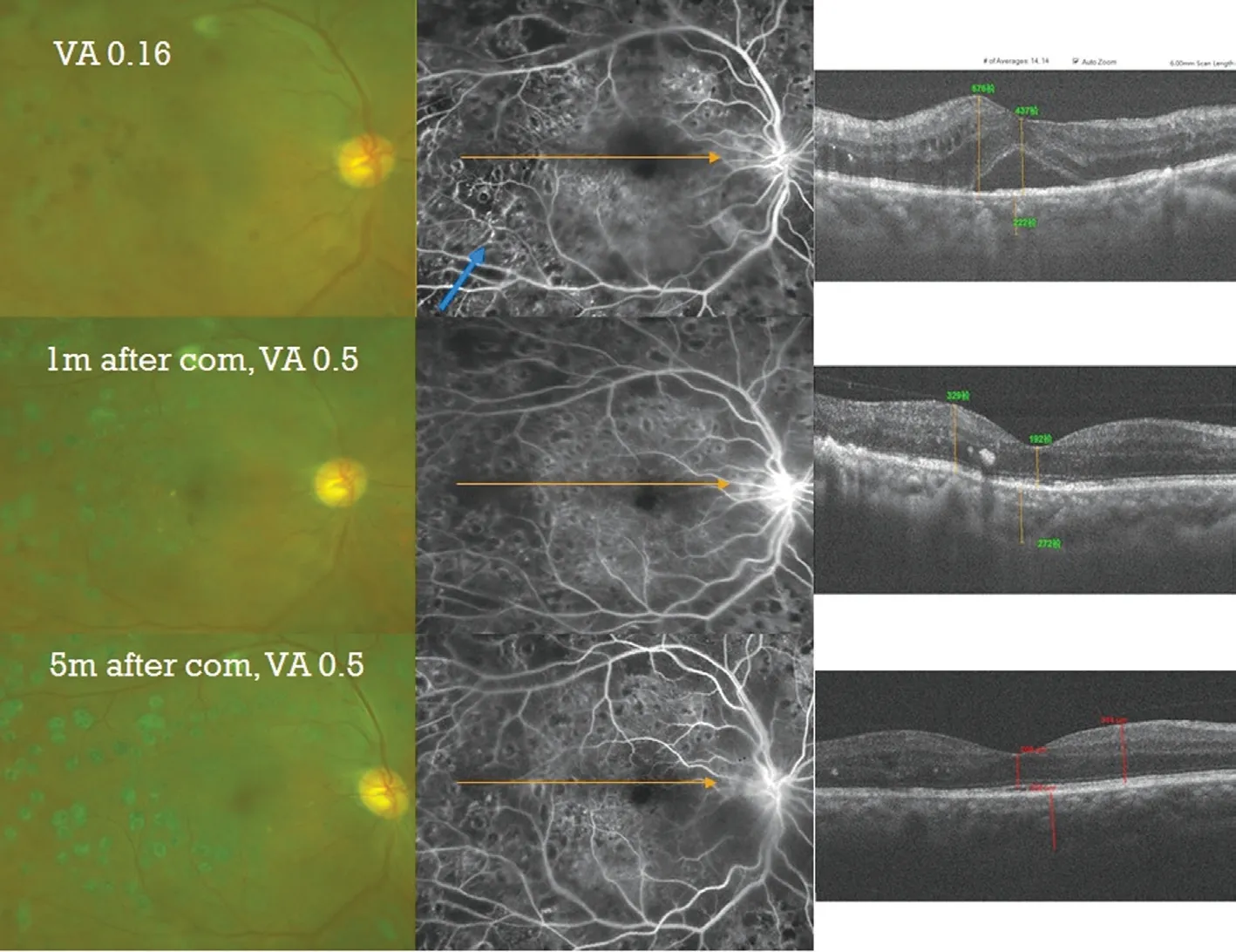
Figure 3 Follow up of treatment of DME by IVC combined with focal laser and IVTA in a 37-year-old man.
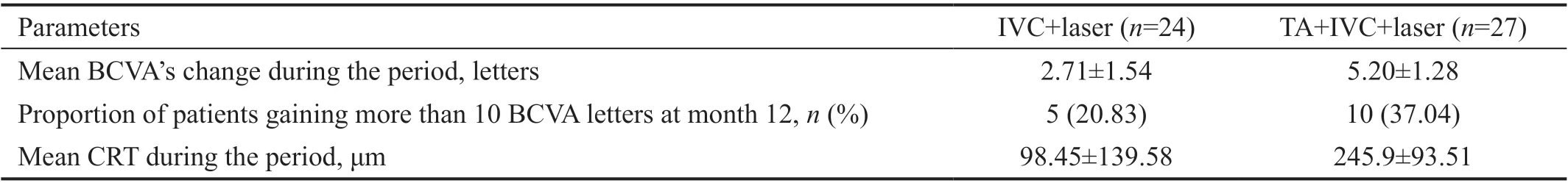
Table 2 BCVA and CRT outcome at 12th month
As the main reason of reducing visual acuity in patients with DR, DME is characterized by fluid accumulations within and under the retina. It is common for breaking the blood‐retinal barrier in most forms of macular edema. Furthermore,the other common complication is the leakage of intraretinal fluid causing by abnormal perifoveal capillary vessels or microaneurysms. The laser therapy in focal and grid has been a standard treatment for DME over 3 decades[8‐9]. However,it is important to note that laser photocoagulation irreversibly damages the focal point of the retina, resulting in reduced visual field[10]. In recent years, anti‐VEGF regimens have gradually used to replace the first‐line treatment, because they can restore and stabilize vision in most DME patients[2‐4].The anti‐VEGF drugs’ clinical effects for treating DME is overshadowed by their high cost. According to statistics, for patients with DME, the median injections were 9‐11 injections in the first year[11]and 17 times over a 5‐year period[12].According to the estimated results from a 15‐year time span simulated model which data from the RESTORE trial, Mitchellet al[7]reported that ranibizumab for DME led to a 0.17 quality‐adjusted life‐year (QALY) gain, with increased cost of £4191.The ratio between incremental cost and effectiveness was about£24 028. Minget al[6]concluded that when compared with the laser group, the intravitreal aflibercept group had better health outcomes (incremental gain of 0.636 QALYs), higher total costs (incremental cost of 82 352 CNY) and increased cost‐effectiveness ratio (ICER of 129 397 CNY or 19 165 USD) per QALY. The cost‐effectiveness research on anti‐VEGF agents in DME treatment urgently necessitates a cheaper alternative,preferably one with similar efficacy and acceptable safety profile as an anti‐VEGF drug.
Because of the anti‐inflammatory properties[13], corticosteroid therapy, including intravitreal triamcinolone and long‐acting dexamethasone implants[14‐15], is an effective therapy for DME. As potent anti‐inflammatory agents, corticosteroids are thought to counteract many of the pathological processes in the development of macular edema[16]. IVTA injections can significantly reduce the levels of IP‐10, IL‐6, MCP‐1, and VEGF in eyes with DME[13]. The efficacy of IVTA in treatment of DME was confirmed firstly in 2001[17]; since then, several clinical trials about IVTA have been performed[18‐19]. In a placebo‐controlled, double‐blind, randomized clinical trial,under the synergistic effect of IVTA and laser, vision increased by two times when compared with the effects of laser only at 24mo[20]. In our study, when compared with IVC combined with focal laser, IVTA combined with both IVC and focal laser improved visual acuity and CRT from baseline to 12mo. Even though the differences in the ratio of patients gaining more than 10 BCVA letters from baseline at month 12 and the average dosage of conbercept injected between the two groups were not significant, the mean costs of treatment burden for 12mo were significantly lower (P<0.001) in the group of IVTA plus IVC and focal laser when compared with those in the group of IVC combined with focal laser group (Figure 3).
AEs of IVTA treatment are related to a high incidence of cataract formation and increased IOP[20]. According to the Diabetic Retinopathy Clinical Research (DRCR) network[21‐25],the incidence of glaucoma treated with 4 mg IVTA for DME was 33%‐50%, 1%‐1.6% cases required glaucoma surgery,and incidence of cataract occurrence was 81%‐83% during the follow‐up of 3‐5y. In a study by Gillieset al[18], the use of 4 mg IVTA for refractory DME resulted in a 68% significant increase in IOP (≥5 mm Hg) and a 54% increase in the incidence of cataracts. Forty‐four percent patients started taking antiglaucoma drugs, and 6 percent required glaucoma surgery. The follow‐up period was 2y. It is reported in a five‐year extension of the same study that the increasement of IOP incidence was 79%, the initiation of IOP‐lowering medication was 56%, 3% of cases called for glaucoma surgery, and the occurrence of cata racts was 71%[26]. In Abdel‐Maboudet al’s[27]Meta‐analysis, at 36 and 48wk follow‐up, the intravitreal bevacizumab (IVB) group was lower IOP than the IVTA group with a statistically significance. In addition, when compared with IVTA or IVB+IVTA, the group who received IVB showed a significant lower intraocular hypertension(IOH) incidence. Even in different IVB and IVTA injections,similar effect seems to be observed. In our study, we used a dose of 1 mg of triamcinolone acetonide, and there was no patient with increased IOP. As we all known, one of the side effects of IVTA was the development of cataracts. However,in this study, IVTA, as an adjunct to the combination of anti‐VEGF with laser, can not only improved the visual acuity and decreased the CRT of the patients with DME but also reduced the number of injections and financial cost when it is administered in the pseudophakic eyes of DME patients.Taking the above factors into consideration, we believe that in countries such as China and other developing countries where patients are unable to afford monthly regimens of anti‐VEGF,IVTA is still a good option.
The way this study enrolling samples was nonrandomized,retrospective, and open label, which is the main limitations,because it means we preclude any evaluation of the efficacy or safety of focal laser and anti‐VEGF when combined with IVTA. Bias of missing data would affect the results of the study. As a result, a longer follow‐up period and a larger sample size may be helpful to validate the results in this study.Despite these limitations, our findings in this study are still promising and suggest that further research may be needed.
In summary, this preliminary study indicated that IVTA as an adjunct to the combination of anti‐VEGF was effective in DME treatment, with similar clinical efficacy. The addition of IVTA reduces the financial cost. The IVTA combination is not inferior to the IVC combined with focal laser treatment and is more cost effective for the management of DME.
ACKNOWLEDGEMENTS
Conflicts of Interest:Yu YY,None;Cheng Y,None;Chang LB,None;Xia HK,None;Li XX,None.
 International Journal of Ophthalmology2021年6期
International Journal of Ophthalmology2021年6期
- International Journal of Ophthalmology的其它文章
- A decrease in macular microvascular perfusion after retinal detachment repair with silicone oil
- Surgical outcomes in acute dacryocystitis patients undergoing endonasal endoscopic dacryocystorhinostomy with or without silicone tube intubation
- Dr. Father Wacław Szuniewicz, a forgotten pioneer in refractive surgery and his work in China
- Deterioration of Avellino corneal dystrophy in a Chinese family after LASlK
- A mutated CRYGD associated with congenital coralliform cataracts in two Chinese pedigrees
- Autophagy dysregulation mediates the damage of high glucose to retinal pigment epithelium cells
