Histological observation in pachyvessels in a patient with choroidal melanoma
Satoru Kase, Kousuke Noda, Susumu Ishida
Department of Ophthalmology, Faculty of Medicine and Graduate School of Medicine, Hokkaido University, Sapporo 060-8638, Japan
Dear Editor,
I am Dr. Satoru Kase, from the Department of
Ophthalmology, Faculty of Medicine and Graduate School of Medicine, Hokkaido University. I write to present a case of choroidal melanoma arising from a thickened choroid.The “pachychoroid” has recently been proposed as an entity comprising an increase in the choroidal thickness and dilatation of large choroidal vessels (so-called pachyvessels)[1].The pachyvessels subsequently compress the choriocapillaris,thereby causing subsequent damage of retinal pigment epithelium (RPE). This entity commonly occurs in eyes with pachychoroid spectrum disorders[2]. In contrast, uncomplicated pachychoroid (UCP) is a new clinical entity, characterized by a thickened choroid containing pachyvessels without RPE disruption[3]. UCP also manifests milder choroidal vascular hyperpermeability (CVH) than common pachychoroid spectrum disorders. However, histopathology of the pachyvessels has yet to be reported.
Choroidal melanoma is a subsequent life-threatening intraocular tumor. Indocyanine green angiography (ICGA)is one of the useful imaging modalities to make a clinical diagnosis of the tumor, whilst little is known about ICGA findings in the background of melanoma. We report a patient with choroidal melanoma arising in UCP and describe the histopathology of pachyvessels in the enucleated eye.
Ethical ApprovalInstitutional review board in Hokkaido university waived application for clinical research of humans because this is a single case report. Written informed consent was obtained to report the clinicopathological data of this patient in the international journal. This study adhered to the tenets of Declaration of Helsinki.
A 51-year-old man suffered from blurred vision in his left eye. The fundus showed a brownish choroidal mass located on the superior side of the macula OS (Figure 1A), while the fundus was normal OD (Figure 1B). ICGA demonstrated hypofluorescence throughout the examination in the tumor and hyperfluorescence in the posterior pole around the tumor (Figure 1C: arrows). Swept-source optical coherence tomography (SS-OCT) showed serous retinal detachment in the macula OS, and a markedly thickened choroid with a subfoveal choroidal thickness measuring over 500 μm (Figure 1D: arrows). There were several dilated choroidal vessels(Figure 1D: asterisks) in the Haller layer OS, consistent with pachyvessels. The choroid was also thickened, measuring over 500 μm similar to OS, with a variety of pachyvessels in the fellow eye OD without RPE abnormalities (Figure 1E). ICGA revealed CVH in the posterior pole OD (Figure 1F). Although small choroidal melanoma was initially suspected OS, he did not desire radiotherapy nor enucleation. When the tumor size gradually increased one year later, SS-OCT did not clearly detect choroidal vessels in the Haller layer. Since the tumor further enlarged, and his visual acuity deteriorated to 0.08(Figure 1G), enucleation was conducted after informed consent was obtained. He is well without distant metastases three and a half years after the initial presentation.
Histopathological FindingsThe tumor was diagnosed as malignant melanoma. Histologically, tumor cells did not invade other surrounding tissues such as the ciliary body, sclera, or optic nerve. In addition, there was RPE damage at the top of the tumor. Protein-like materials markedly accumulated in the choroidal stroma (Figure 2A, asterisk) adjacent to the tumor,admixed with normal choroidal vessels. There were markedly dilated vessels containing protein-like materials in the lumen(Figure 2B) adjacent to the tumor. Further, large choroidal vessels were located in the Haller layer apart from the tumor(Figure 2C). Immunoreactivity for alpha-smooth muscle actin (αSMA) was exhibited by normal choroidal arteries(Figure 2D: arrow), whereas the expression was less marked in the pachyvessels (Figure 2D: asterisk) and choriocapillaris.Immunoreactivity for CD34, a vascular endothelial marker,was noted not only in the choriocapillaris and choroidal veins/arteries (Figure 2F: arrow) but also tumor vessels, as shown in a previous study[4]. However, CD34 immunoreactivity was not detected in dilated vessels located in the Haller layer (Figure 2E) or adjacent to the tumor (Figure 2F: asterisk). In contrast,D2-40, a lymphatic endothelial cell marker, was not expressed in any of the choroidal vessels (data not shown).
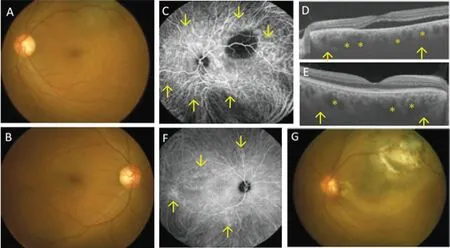
Figure 1 Funduscopic examination (A, B, G), indocyanine green angiography (ICGA; C, F), and swept-source optical coherence tomography (SS-OCT; D, E) of a choroidal melanoma patient Fundus examination reveals a round choroidal mass located on the superotemporal side of the posterior pole at the initial presentation (A) in the left eye. The fundus is normal in the right eye (B). ICGA reveals hypofluorescence in the tumor in the left eye (C), whereas there is hyperfluorescence in the posterior pole (C, F, arrows) in both eyes. Figures D and E are horizontal sections of the macula. SS-OCT imaging shows retinal detachment and a thickened choroid, measuring 518 μm in the subfoveal choroid (D, arrows) together with markedly dilated vessels (D, asterisks) in the left eye. SS-OCT also shows a thickened choroid (E,arrows) with dilated choroidal vessels (E, asterisks) in the right eye. The enlarged choroidal tumor involves the macula before enucleation (G).
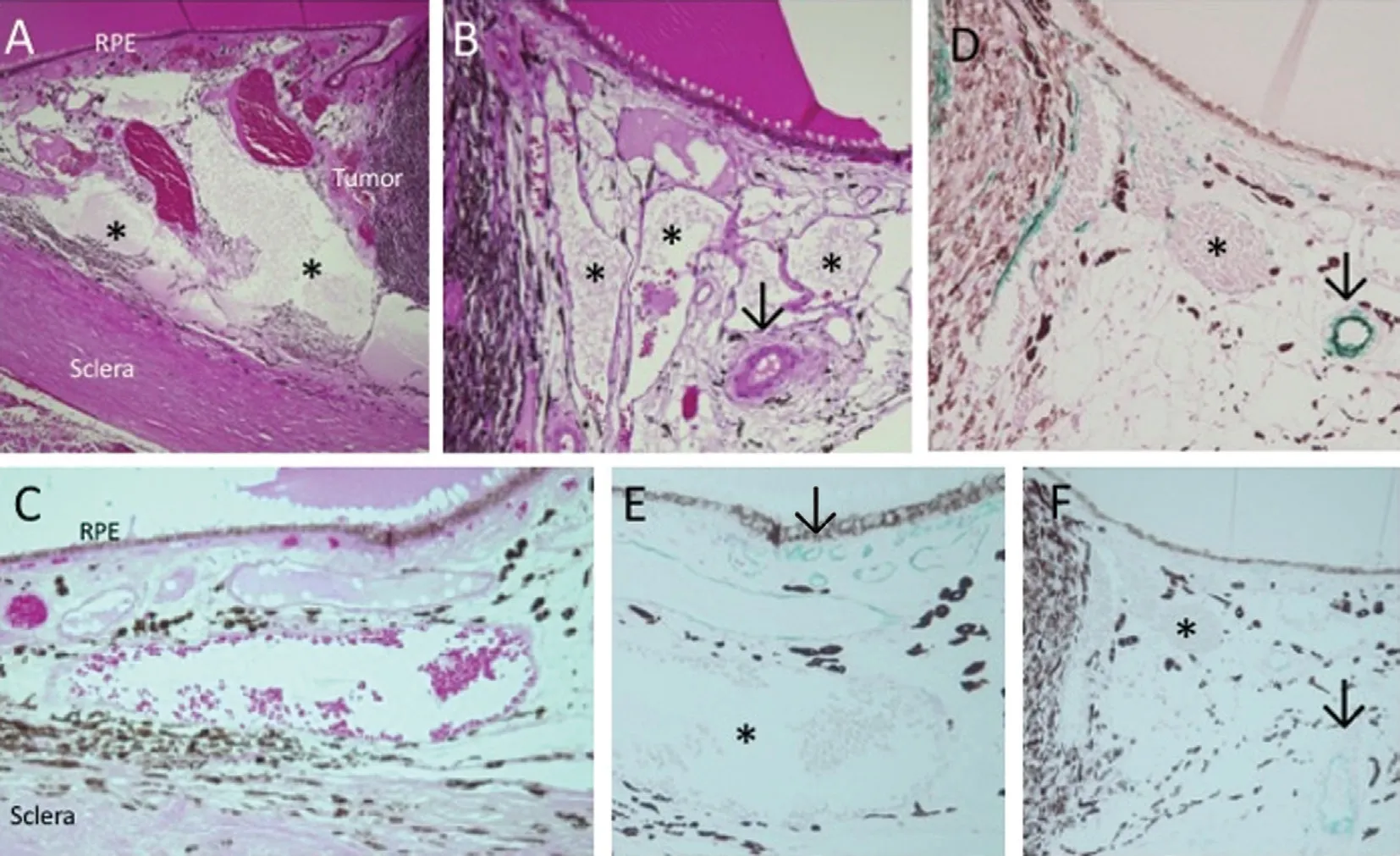
Figure 2 Histological findings (A-C) and immunoreactivity for alpha-smooth muscle actin (αSMA; D) and CD34 (E, F) in a choroidal melanoma patient Some protein-like materials markedly accumulate in the choroidal stroma (A, asterisks) adjacent to the choroidal melanoma(A, tumor) on the temporal side. There are highly dilated veins located in the Haller layer containing protein-like materials (B, asterisks) on the nasal side of the tumor, where a normal choroidal artery is observed (B, arrow). Further large choroidal vessels were located in the Haller layer apart from the tumor (C). Immunoreactivity for αSMA is less marked in the dilated vessels (D, asterisk) than in normal choroidal vessels (D,arrow: histogreen visualization). Immunoreactivity for CD34 is noted in the choriocapillaris and choroidal veins/arteries (E, F, arrow), but not in the dilated vessels located in the Haller layer apart from the tumor (E, asterisk) or adjacent to the tumor (F: asterisk).
DISCUSSION
This study is the first report of clinicopathological findings in pachyvessels in an enucleated eye with choroidal melanoma.SS-OCT detected the highly thickened choroid with pachyvessels in the Haller layer in both eyes. ICGA revealed CVH in the posterior pole, consistent with features of UCP.The pachyvessels located in the Haller layer histologically had thin vessel walls and contained protein materials in the lumen. This case further demonstrated marked accumulation of protein-like materials in the choroidal stroma adjacent to the tumor. Whether the material accumulation was dependent on/independent of choroidal melanoma remains unclear. One of the causes may be tumor enlargement, since the stromal area OS detected by SS-OCT increased as the tumor grew larger.These findings suggest that pachyvessels are leaky vessels, in which protein leakage may have been promoted from vessels in cases of vessel compression due to tumor enlargement.
These histological findings also indicate that the thickened choroid and CVH detected by clinical images are caused by stromal protein accumulation and pachyvessels. αSMA and CD34 immunoreactivities were less marked in pachyvessels,suggesting disruption of the actin filament configuration and endothelial cells or elongation of smooth muscle cells by the dilatation of the vessels. The immunohistochemical findings might be histological features of pachyvessels and associated with CVH and an increased choroidal thickness.
A limitation of this study is that there is a possibility of these two conditions co-occurring incidentally: UCP and choroidal melanoma. Pathological analyses of eyes with UCP without choroidal melanoma would overcome such a limitation.
ACKNOWLEDGEMENTS
Conflicts of Interest:Kase S,None;Noda K,None;Ishida S,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
