Transepithelial photorefractive keratectomy for myopia:effect of age and keratometric values
Amanda Nur Shinta Pertiwi, Indra Tri Mahayana, Agus Supartoto,2, Wasisdi Goenawan,2, Suhardjo,2
1Department of Ophthalmology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada-Sardjito Eye Center, Dr. Sardjito General Hospital, Yogyakarta 55284,Indonesia
2Dr. Yap Eye Hospital, Yogyakarta 55232, Indonesia
Abstract
● KEYWORDS: transepithelial photorefractive keratectomy;refractive surgery; emmetropization; overcorrection
INTRODUCTION
There has been an increasing trend of employing photorefractive keratectomy (PRK) in surface ablation refractive surgery these recent years. PRK has shorter learning curve, lower surgical cost and lower risk for corneal ectasia[1].Transepithelial PRK (transPRK) has been established as a technique of PRK practiced worldwide for a few decades. It was introduced in late 1990s by Alioet al[1]to reduce the risk of conventional PRK which employed mechanical debridement prior to laser ablation[2-3]. In transPRK, ablation of the corneal epithelium and stroma is performed using an excimer laser rather than mechanical or chemical debridement techniques.Hence, it prevents flap-related complication as in laser assistedin-situkeratomileusis (LASIK) or mechanical debridementrelated conditions such as stromal dehydration, uneven epithelial debridement resulting in rough stromal wound bed,Bowman’s layer defect, an irregular anterior stromal surface,and retained islands of residual epithelium[4-5].
There are two techniques of transPRK in terms of epithelial layer removal: 2-step (PTK/PRK) and single-step transPRK.The later of which the epithelial layer is ablated in one single session along with the stromal ablation. TransPRK has evolved through several techniques aimed to optimize the refractive outcome and minimize complications[4]. Previous studies has reported efficacy, predictability and safety of these two techniques in myopic, hyperopic and astigmatic corrections with various results[6-10]. In myopic and/or myopic astigmatism correction, transPRK shows good and comparable refractive outcome compared to conventional PRK even though overcorrection happened more often in transPRK[2].
In this modern PRK era, there is increase understanding regarding refractive surgery along with the expectations of the good refractive outcomes. Meanwhile, there has always been imperfections and unachieved refractive target after laser ablative surgeries such as reported by several previous studies[11-13]. Thus, it triggers clinicians and refractive surgeons to look more onto what factors might affect laser ablative surgical success[13]. Very limited studies reported some demographic and preoperative factors affecting retreatmet rate after LASIK and PRK[12-17]. Moreover, to the best of our knowledge, this is the first study reporting demographic and preoperative factors affecting the success of transPRK in Asian population.
SUBJECTS AND METHODS
Ethical ApprovalStudy protocol has been approved by Institutional Review Board of Gadjah Mada University Medical Faculty (Ethics Committee Aproval Code: C64059)and was conducted according to the tenets of Declaration of Helsinki 2008. Informed consent was waived due to the retrospective nature of the study.
This retrospective cohort study consecutively included 140 eyes of 87 patients with myopia and myopic astigmatism who underwent transPRK between June 2015 and May 2019 at Dr. Yap Eye Hospital Yogyakarta, Indonesia. The inclusion criteria were myopic and/or myopic astigmatism patients, age greater than 17y; a stable preoperative refraction for at least 12mo; emmetropic (logMAR 0) refractive outcome target;intraocular pressure (IOP) less than 21 mm Hg; Schirmer I result more than 10 mm in 5min; a period without wearing contact lenses (more than 2wk for rigid contact lenses and more than 4d for soft contact lenses); no abnormality in the retina; and no history of autoimmune disease, diabetes, or ocular surgery. Keratitis and haze which impair visual acuity were considered as the exclusion criteria. Eligible subjects were devided into emmetropia or ametropia group according to uncorrected distance visual acuities (UDVA) 3mo postoperative. Emmetropia was defined as UDVA of logMAR 0 or better anytime post-operatively and/or no residual refractive error.
Data CollectionThe medical records of all eligible patients were reviewed and the following demographic and preoperative information extracted: age, sex, date of surgery, central corneal thickness (CCT; Orbscan II, Bausch and Lomb, USA),preoperative subjective spherical error and astigmatism,preoperative subjective spherical equivalent (SE), mean keratometric power in 5.00 mm of central cornea (mean K;Orbscan II, Bausch and Lomb), anterior maximum keratometry reading (Kmax), anterior minimum keratometry reading(Kmin), UDVA, corrected distance visual acuity (CDVA) and Schirmer I test results. The following intraoperative information was also extracted: transPRK technique (2-step transPRK or single-step transPRK), ablation depth, residual stromal bed(RSB), treatment plan (Planoscan or Tissue Saving), laser pulse, treatment time and the surgeon’s name.
Surgical TechniquePatients were given 5 mg of oral clobazam and 50 mg of oral diclofenac potassium. One drop of tetracaine 2% and 1 drop of chloramphenicol 0.25% were instilled in in the conjunctival fornix of the to be treated 3 times 5min apart prior to surgery. The eyes were then scrubbed and draped, and a Lieberman eyelid speculum was placed between the lids of the eye to be treated. The other eye was occluded. The ablations were performed by Technolaz 217z100 excimer laser (Bausch & Lomb, Rochester, New York) using the phototherapeutic-mode of the excimer laser(2-step transPRK) or using a single continuous laser shooting session to ablate both the epithelium and stroma in a single step (single-step transPRK). After excimer ablation, a sponge soaked with mytomycin-C (MMC) 0.02% was placed on the stroma for 60s. The MMC was rinsed from the ocular surface and a contact lens placed on the cornea. Postoperatively,patients received gatifloxacin eyedrop, fluorometholone 0.1%eyedrop, artificial tears, oral levofloxacin, oral diclofenac potassium, oral diazepam and oral vitamin C. They were examined at 1d, 1wk, 1, 2, and 3mo, and as necessary.Patients were encouraged to return for examination if vision deteriorated at any time after surgery.
Statistical AnalysisData were analyzed using SPSS software(version 22.0). Normality test was performed to all variables using Kolmogorov Smirnov test. Numerical data were tested using independentt-test if data were normally and using Mann-Whitney test if data were not normally distributed.Nominal data were tested using Chi-square/Fisher exact test.Bivariate analysis using Logistic regression was performed to independent variables to see their relationship with dependent variables and to calculate the odds ratio (OR). Multivariate analysis using Logistic regression (model 1) was performed to independent variables withP<0.25 on bivariate analysis.Adjusted multivariate analysis (model 2) was also performed to obtain which independent variable was the strongest predictor for ametropia following transPRK. Null hypothesis was rejected ifP<0.05 (95%CI) on bivariate Logistic regression and alternative hypothesis was accepted.
RESULTS
Primary OutcomesSubjects (140 eyes treated by transPRK)were devided into 2 groups based on UDVA measured 3mo post operatively: 120 (85.71%) eyes in emmetropia group and 20 (14.29%) eyes in ametropia group. There was a male preponderance with 79.29% eyes. Table 1 shows the demographic characteristics of the subjects in each group.There was a statistically significant difference of age between the two groups (P<0.001). The mean age of the subjects was 20.73±7.29y (range 17 to 55y; median 18.0y). The mean preoperative subjective spherical error and astigmatism were-2.49±1.60 D (range -0.5 to -8.75 D; median -2.25 D) and 0.68±0.59 D (range 0 to 3.50 D; median 0.5 D), respectively.The mean preoperative SE was -2.83±1.73 D (range -0.75 to-9.0 D; median -2.50 D). The mean preoperative visual acuity(logMAR) was 0.86±0.35 (range 0.1 to 1.80; median 1.0).Table 1 also shows preoperative subject characteristics of which there was no statistically significant difference between the two groups.
Table 2 shows that treatment time, ablation depth and laser pulse were higher in ametropia group and statistically significant.The mean treatment time in ametropia and emmetropia group were 47.55±12.18s and 41.33±13.43s, respectively (P=0.025).The mean ablation depth in ametropia and emmetropia group were 119.70±26.72 µm and 103.33±28.26 µm, respectively (P=0.017).The mean laser pulse in ametropia and emmetropia group were 3634.10±1181.81 and 2963.01±875.92, respectively(P=0.003).
Figure 1A shows higher preoperative refractive error was associated with significantly higher risk of ametropia. There was an increasing OR as the degree of preoperative refractive error increased. OR in SE higher than -6.0 D was 5.29(P=0.010). Figure 1B shows that higher preoperative Kmax was associated with significantly higher risk of ametropia.There was an increasing OR as the degree of preoperative Kmax increased. OR in Kmax higher than 45 D was 4.28 (P=0.013).Kmax higher than 46 D was associated with 21 times more risk of ametropia after transPRK (P=0.010). Figure 1C shows that higher preoperative mean K was associated with significantly higher risk of ametropia. There was an increasing OR as the degree of preoperative mean K increased. OR in mean K higher than 44 D was 4.35 (P=0.008). Mean K higher than 45 D was associated with 5 times more risk of ametropia after transPRK (P=0.045). Figure 1D shows that older age was associated with significantly higher risk of ametropia. There was an increasing OR with increasing age. OR in age >30y was 58 (P=0.000). Subjects in ametropia group was older than those in emmetropia group (P<0.001).
Table 3 shows the effect of preoperative and intraoperative factors on the risk of ametropia, based on bivariate and multivariate Logistic regression analysis. The following parameter significantly influenced the risk of ametropia in bivariate analysis: higher preoperative Kmax, higher mean K,higher preoperative subjective myopia, higher preoperative SE and older age, increased the risk of ametropia. In multivariate analysis model 1, age appeared to be the strongest factoraffecting the risk of ametropia. There were statistically significant differences between ametropia and emmetropia groups in treatment time, ablation depth and laser pulse. Thus we performed an adjusted multivariate Logistic regression analysis (model 2) to see which factor was the strongest predictor for the risk of ametropia. Model 2 resulted in age as the strongest factor for the risk of ametropia following transPRK (P=0.009).
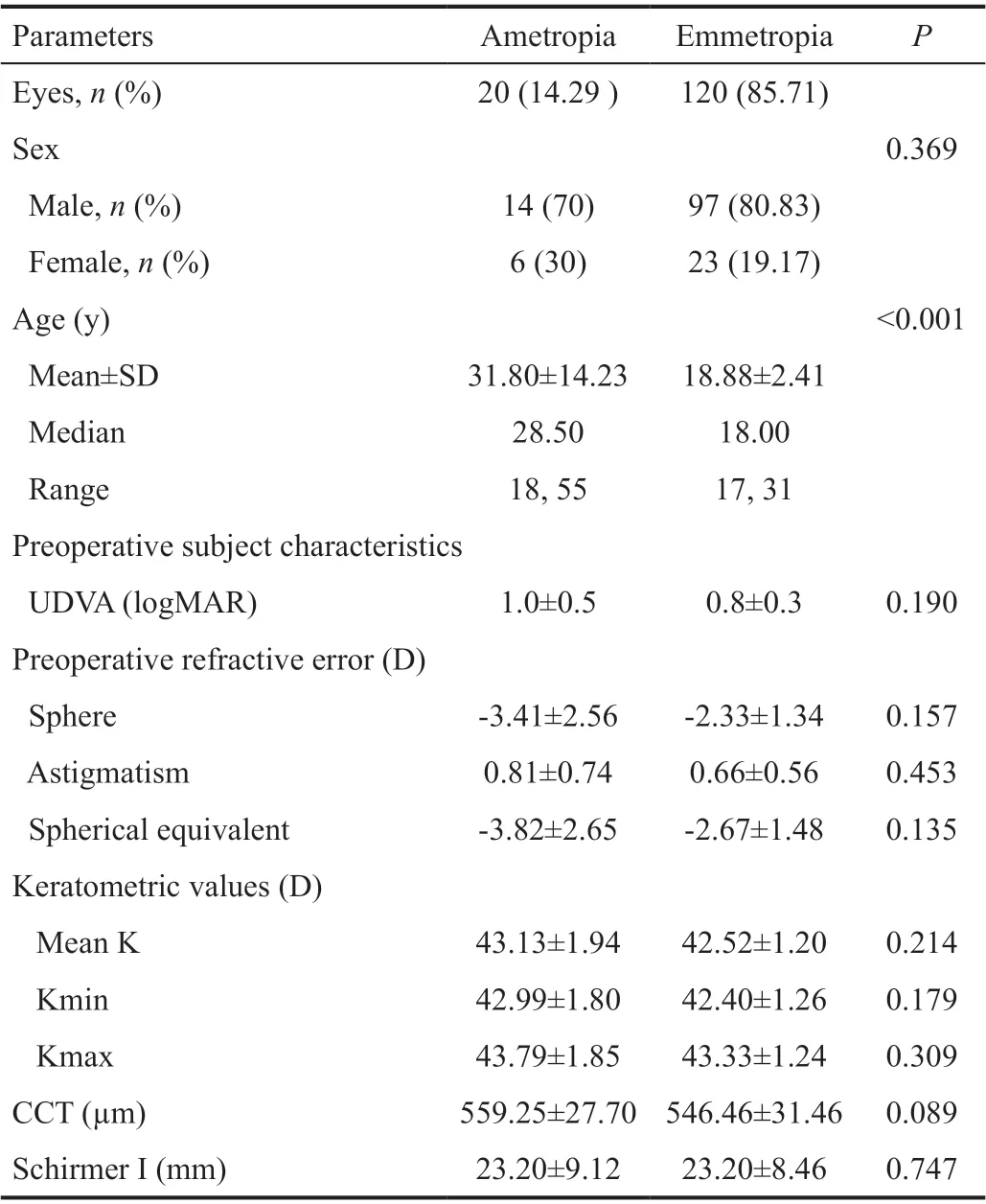
Table 1 Demographic and preoperative subject characteristics means±SD
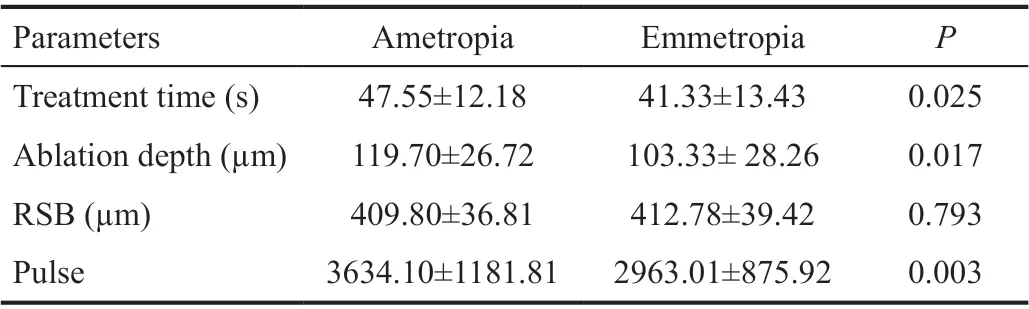
Table 2 Intraoperative parameter means±SD
Overcorrection was found in 10 eyes of 5 subjects. The mean preoperative spherical error and astigmatism were -4.33±2.46 D(range -2.00 to -8.75 D; median -3.38 D) and 0.69±0.27 D(range 0.50 to 1.25 D; median 0.5 D), respectively. The mean of CDVA postoperative was 2.93±1.46 (range +0.0 to +4.00;median +3.63). One eye could reach emmetropia after 116d postoperative and the fellow eye reached CDVA of +0.5 D.Orbscan II of 4 eyes showed irregularity of the 3 and 5 mm optical zone which passed 1.5 and 2.0 respectively.
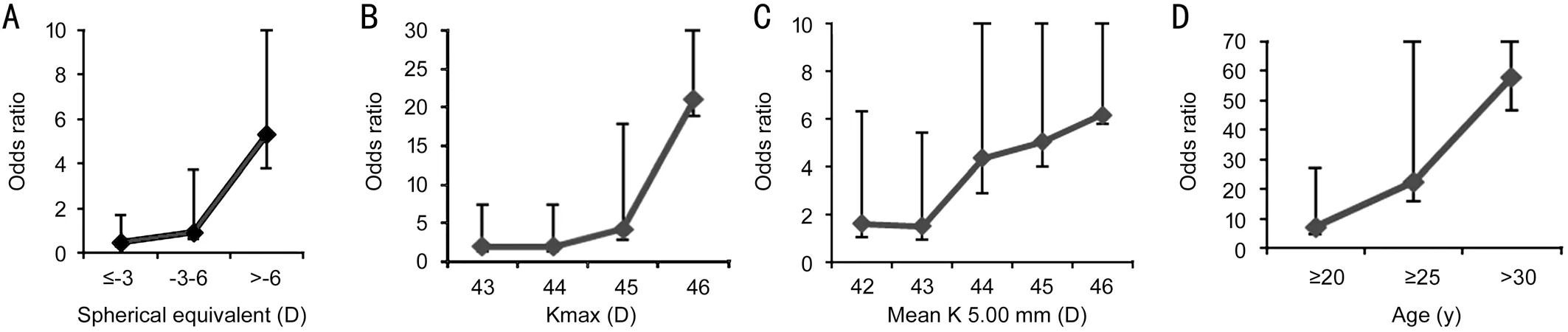
Figure 1 OR of ametropia based on degree of preoperative refractive error in SE (A); OR of ametropia based on anterior maximum keratometry reading (Kmax; B); OR of ametropia based on mean keratometric power in 5.00 mm of central cornea (mean K; C); OR of ametropia based on age (D).

Table 3 Bivariate and multivariate Logistic regression analysis of preoperative and intraoperative factors predicting ametropia
One subject (2 eyes) aged 19y, experienced delayed near visual recovery after transPRK with near addition of +1.0 D. The preoperative SE was -1.25 and -1.63 D for the right and left eyes respectively.
DISCUSSION
This was a retrospective cohort study investigating the preoperative and intraoperative parameters associated with ametropia after myopic transPRK. It showed that high preoperative subjective refractive error, high Kmax, high mean K of the 5 mm central cornea and older age significantly increased the risk of ametropia. These parameters were significant on bivariate analysis. Multivariate analysis resulted in age as the strongest factor increasing the risk of ametropia. Several cut-off points were found which could be useful for predicting patients’ refractive outcome following transPRK for myopia and myopic astigmatism and for further research purpose. There were also 10 cases of overcorrection with 4 cases of suspected early posterior corneal ectasia needing further examinations and 1 case of accommodation insufficiency as the noteworthy complication of transPRK.
Subjects in ametropia group were older than those in emmetropia group (P<0.001). Older age was found to significantly increase the risk of ametropia both in univariate and multivariate analysis. This finding corroborates several previous studies which supports older age as a factor increasing retreatment rate or ametropia following LASIK and PRK[13-16,18], although some studies found no correlation between increasing age and retreatment rate[12,17]. Age more than 40y has been known to be age at risk for corneal refractive surgery procedures[13].In LASIK and PRK, increasing age is associated with overcorrection. Whereas in small incision lenticule ertraction(SMILE), it is associated with undercorrection[19]. Aging cornea experience some changes on its structures which may cause a natural glication-mediated cross-linking[20].Previous study also found increasing corneal hysteresis and decreasing corneal resistance factor in aging corneas[21]. These ultrastructure changes as an aging process may play some roles in the unpredictable refractive outcome following corneal laser ablative surgeries. These facts warrant further research on the interplay between the ultrastructure changes of aging cornea,wound healing process, corneal biomechanics and refractive surgery outcomes.
There was an increasing OR as the degree of preoperative refractive error increased (Figure 1A). Subjects with preoperative subjective refractive error of more than SE -6.0 D had 5.29 times more risk of ametropia following transPRK (P=0.010).This finding was in line with some previous studies agreeing that retreatment rate or ametropia after LASIK and PRK was associated with higher degree of initial correction[11,14-15,17,22-23].This might happen due to the less predictability of nomogram in higher correction[15]. The higher the initial correction, the more is ablated corneal tissue. Ablation depth is associated with wound edge and surface regularity, RSB biomechanics and stromal regeneration. The more the ablated corneal stroma,the more irregular and steeper the surface and wound edge is resulted. This may increase the probability of epithelial hyperplasia, collagen and extracellular matrix deposition[24-25].Those factors may be the cause of the less predictable refractive outcome in higher spherical error correction in transPRK as well.
Another primary outcome in this study was cut-off points from keratometric value as predictors for ametropia following transPRK. Subjects with Kmax higher than 45 D had 4.28 more risk of ametropia (P=0.013). Increasing the cut-off point into 46 D of Kmax rose the odds of getting ametropia into 21 times more risk (P=0.010). Mean K of the central 5 mm cornea higher than 44 D was associated with 4.35 more risk of ametropia (P=0.008). Increasing the cut-off point into 45 D of mean K rose the odds of getting ametropia into 5 times more risk (P=0.045). A research done by Ambrósioet al[26]for color scaling software in Pentacam (Ambrosio 2) proposed mean of keratometric values in normal population of 43.1±1.43 D and 44.6±3.4 D for mean K and Kmax respectively. The keratometric values found to increase the risk of ametropia following transPRK here are all above the numbers proposed by Ambrósioet al[26]in his population study. Retreatment rate was significantly found to be higher in subjects with keratometric value >46 D[14]. Steeper corneal curvature triggers more intense remodeling process thus lowering the predictability of PRK refractive outcome[27]. In this study, there were proposed cut-off points of 45 D for Kmax and 44 D for mean K in 5 mm optical zone as the predictors for ametropia following transPRK. These cut-off points may be useful for further research purpose and also important for patient education regarding the success of refractive surgery outcome.In this present study, we found some complications following single-step transPRK as our secondary outcomes. There were 10 cases of overcorrection with 4 cases of suspected early posterior corneal ectasia. Another case is a 19 years old male with blurry vision on near-work corrected with addition lens of S+1.0 D. Subjects with overcorrection were all above 30 years old. As shown in Figure 1D that age >30 years old increase the risk of ametropia following transPRK by 58 times (P=0.000).Preoperative spherical error and astigmatism showed a vast range of refractive error. The mean Kmax and mean K also showed a broad range of values. There were 4 eyes with preoperative Schirmer I test of ≤10 mm (range 2-30 mm). Thus,it was suspected that low Schirmer I test value as one factor contributing to this overcorrection. Three subjects (6 eyes)refused to visit for Orbscan II examination, hence we only have 4 Orbscan II data from 4 eyes of 2 subjects. Orbscan II data showed irregularity of the 3 and 5 mm optical zone which passed 1.5 and 2.0 respectively. These finding could indicate an early keratoectasia which warrant further serial examinations to establish this diagnosis. Keratoectasia patients tend to be younger, more myopic, have thinner corneas preoperatively,lower postoperative RSB thickness, and more frequently have abnormal preoperative topographies as compared to patients who do not develop ectasia. According to Ectasia Risk Score System (ERSS) developed by Randleman[28], these 4 eyes scored low risk for keratoectasia. However, there is no single parameter that could predicts the development of keratoectasia.Keratoctasia may also occur in an otherwise healthy cornea if there is significant weakening caused by the surgery[27].
One subject (2 eyes) with near addition of +1.0 D 2mo postoperative was suspected to have accommodation insufficiency.This is probably due to accommodative amplitude change from myopia to emmetropia following transPRK which requires another extra +1 D of accommodation to do near-work activities at 30 cm range. A study showed transient near-vision problems in younger myopes in early postoperative days after PRK might be due to decrease in amplitude of accommodation and facility of accommodation, which will eventually increase overtime[29].
The mechanism underlying the overcorrection and the accommodation insufficiency occurred following single-step transPRK has not yet been explained due to the nature of its retrospective design. Further prospective research is needed to study the interaction between single-step ablation profile,degree of preoperative myopia, steepness of anterior and posterior corneal curvature, corneal biomechanics changes following transPRK and the refractive outcome. Incorporation of anterior segment-OCT (AS-OCT) and ocular response analyzer (ORA) might be useful for further study.
In conclusion, older age was found strongly associated with the increasing risk of ametropia following transPRK. Cut-offpoints of Kmax and mean K 5 mm for ametropia risk at 45 and 44 D were proposed. Further prospective study is needed to elucidate precisely on what aging process and steep cornea might do to wound healing and corneal remodeling following transPRK.
ACKNOWLEDGEMENTS
We would like express our best gratitude and appreciation to the enthusiastic cooperation and warm welcome of Dr. Yap Eye Hospital, Yogyakarta, for being the host of the present study.
Conflicts of Interest: Pertiwi ANS,None;Mahayana IT,None;Supartoto A,None;Goenawan W,None;Suhardjo,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
