Optical and visual quality comparison of implantable collamer lens and femtosecond laser assisted laser in situ keratomileusis for high myopia correction
Zheng Jiang, Hua Wang, Dong-Qiang Luo, Jiao Chen
1Medical College, Hunan Normal University, Changsha 410006, Hunan Province, China
2Center for Ophthalmic Optics, Hunan Provincial People’s Hospital; the First Affiliated Hospital of Hunan Normal University, Changsha 410005, Hunan Province, China
Abstract
● KEYWORDS: implantable collamer lens implantation;femtosecond laser assisted laser in situ keratomileusis;refractive stability; high myopia
INTRODUCTION
Myopia can be classified in two types: low to modest degrees of myopia (0 to -6.00 D) and high myopia(greater than -6.00 D). Currently, refractive surgery which correcting high myopia includes corneal refractive surgery represented by femtosecond laser assisted laserin situkeratomileusis (FS-LASIK) and intraocular refractive surgery represented by implantable collamer lens (ICL) implantation.FS-LASIK has high accuracy and patients can obtain good optical and visual quality after surgery[1]. However, FSLASIK, as a kind of corneal refractive surgery, has a high risk of postoperative keratectasia, so it is theoretically not suitable for people with high myopia or thin cornea[2]. ICL implantation can correct a large-scale of refractive errors, and it does not ablate the cornea, which can make up for the drawbacks of corneal refractive surgery[3-7]. Although the current performance of ICL implantation in terms of the high myopia correction are encouraging, the long-term efficacy and safety of this kind of surgery still need to be further observed and evaluated due to the short time of clinical application of this technique and the limited number of cases. This study used the Optical Quality Analysis System (OQAS) to compare clinical outcomes of ICL implantation and FS-LASIK for high myopia correction.We analysed the OQAS parameters to explore the potential influence factors which may have impact on the effect of high myopia correction, to detect which procedure have moreadvantages in high myopia correction. This allows to show how the different surgical procedures effect the high myopia correction,which can further optimize the operation result, and improve the patient’s postoperative visual quality and satisfaction.

Table 1 Preoperative demographics of study subjects
SUBJECTS AND METHODS
Ethical ApprovalThe Ethical Committee Review Board of Hunan Provincial People’s Hospital approved this project.Provided with verbal and written explanations of the possible consequences of the research, all patients have signed written informed consent. During the whole study, we obeyed the tenets of the Declaration of Helsinki.
ParticipantsTwenty-eight refractive surgery candidates (48 eyes) with high myopia that underwent the vision ICL (STAAR Surgical Company, Monrovia, California, USA) implantation and thirty-two refractive surgery candidates (58 eyes) with high myopia that received FS-LASIK were subordinated to this prospective study. Treatments were performed between April 2018 and November 2018 at Center for Ophthalmic Optics,Hunan Provincial People’s Hospital (Changsha, China).Myopic power ranged between -6.00 and -12.00 D with astigmatism <0.50 D. The mean age was 27.31±5.50y (range:18 to 37y). Inclusion criteria for ICL implantation were: 1)the patients whose refractive stability over the past 24mo,spherical refraction increased by <0.5 D per year, and corrected distance visual acuity (CDVA) ≥0.5 (decimal); 2) those were not good candidate for FS-LASIK due to thin corneal thickness; 3) those who voluntarily choose ICL implantation,and can fully understand the surgical complications. Exclusion criteria for ICL implantation were: 1) anterior chamber depth of ≤2.8 mm; 2) endothelial cell density of ≤2000 cell/mm2;3) systemic diseases that could impact the wound-healing process. Inclusion criteria for FS-LASIK were: 1) contact lens wearers to stop wearing them 4wk prior to surgery; 2) the patients whose refractive stability over the past 24mo, spherical refraction increased by <0.5 D per year, and CDVA≥0.5; 3)normal corneal thickness (an estimated residual stromal bed thickness of more than 250 μm)[2]. Exclusion criteria for FSLASIK were: 1) residual corneal stroma thickness<280 μm;2) the keratoconus suspects. Statistical analysis showed no significant difference in age, gender, CDVA and spherical equivalent between the two groups preoperatively (P>0.05,Table 1).
MethodsBefore and after operation, we used the OQAS(Visiometrics, Terrassa, Spain) to acquire the optical quality parameters: the modulation transfer function (MTF) cutoff frequency, the strehl ratio (SR), the objective scatter index(OSI). With the help of the Fourier transform, the OQAS could calculate the image of a light source (780 nm laser diode)reflected on the retina, which is designed on the basis of the asymmetric pattern of the double-pass technique with different entrance and exit of pupil sizes. It is the only currently available instrument used for objective measurement of the effect of optimal aberrations and the loss of ocular transparency on the human eye. It provides optical quality parameters, such as MTF, SR and the OSI. Before the measurements, the room illumination was kept low (approximately 25 lx) and the pupil diameter was more than 4.0 mm in all eyes during testing. The manifest refractive error of the patients was corrected fully during these measurements, the spherical error (up to -8.00 D)as well as the cylindrical error (up to -0.50 D) was corrected automatically by the double-pass system, the residual spherical error (over -8.00 D) and the cylindrical error (over -0.50 D)were corrected using an external lens because the uncorrected refractive error affects the optical outcome of the system directly.
Several studies[8-9]have explained the parameters’ meaning.The MTF specifies how different spatial frequencies are handled by an optical system such as a human eye. It is used by ophthalmologists to describe how the light from the object or scene focused onto a retina in the optical transmission chain.The MTF cutoff frequency is the frequency at which the MTF arrives at a value of 0.01. The results are given in cycles per degree. It stands for the frequency up to which the eye can focus an object on the retina with a significant 1% contrast.The loss of high frequencies represents a loss of information regarding the details of an object, thus reducing the image quality and visual acuity. Theoretically, an MTF cutoff of 30 cycles per degree (cpd) usually is equal to 20/20 visual acuity[8].
The SR is often interpreted as the ratio of the peak aberrated image intensity from a point source compared to the maximum gainable intensity using a theoretical optical system limited only by diffraction over the system’s aperture. In optometry,it is the ratio between the aberrated eye and the theoretical aberration-free eye in the MTF profiles. The SR represents retinal imaging quality and has a value between 0 and 1,perfectly unaberrated optical system theoretically having an SR of 1[9].
The OSI is calculated as the ratio of the amount of light outside the double-pass retinal intensity point spread function(PSF) image in the peripheral zone with a ring set between 12 and 20min of arc to the central zone with a circle of a radius of 1min of arc of the retinal image. The OSI for normal eyes would approximately range 1, while values over 5 would indicate highly scattered systems.
Implantable Collamer Lens and Surgical ProcedureAll the ICL implantation procedures were carried out by the same experienced surgeon. On the day of surgery, the patients were given dilating agents. After topical anesthesia and injection of 1% sodium hyaluronate into the anterior chamberviaa puncture site at the 6 o’clock position of the cornea, ICL was inserted through a 2.8 mm limbal incision and carefully positioned in the posterior chamber using a manipulator.Then, balanced salt solution (BSS) was used to wash out the viscoelastic surgical agent. Antibiotics eye drops, artificial eye drops, non-steroidal anti-inflammatory eye drops, and steroidal eye drops were used postoperatively.
Femtosecond Laserin situKeratomileusis ProcedureAfter topical anesthesia with 0.5% proparacaine hydrochloride,a suction ring was used to fix the cornea and raising the intraocular pressure to around 65 mm Hg before creating a corneal flap which pedicle was placed on the top. Then a flap with a thickness of 100-120 μm, flap diameter of 8.2-8.5 μm was created using WaveLight FS200 femtosecond laser. After lifting the flap, The WaveLight Allegretto EX500 (Alcon,TX, USA) was used for stromal ablation for a 6.00-6.50 mm optical zone. During the ablation, an active eye tracker was used to assure accurate ablation on the center of the pupil.Then, the stroma was washed with BSS solution and the flap was carefully repositioned over the stroma. The postoperative treatment included antibiotics eye drops, artificial eye drops,non-steroidal anti-inflammatory eye drops, and steroidal eye drops.
Statistical AnalysisTwo-samplet-test was used to compare different surgical procedure data. Results was expressed as the mean±SD and the statistical significance was set atP<0.05.
RESULTS
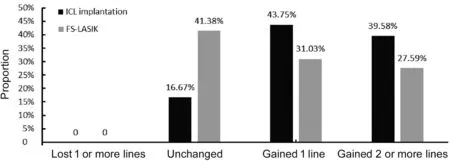
Figure 1 Comparison of 1-year changes in CDVA after ICL implantation and FS-LASIK for high myopia correction.

Figure 2 Comparison of 1-year proportions in UDVA after ICL implantation and FS-LASIK for high myopia correction.
Visual Acuity, Safety, and EfficacyOne-year changes in vision indices between the two groups are compared in Figures 1, 2, and Table 2. No statistically significant differences were observed in uncorrected distance visual acuity (UDVA) between ICL and FS-LASIK groups (allP>0.05) in postoperative 1wk and 1mo, but UDVA were better after ICL implantation than after FS-LASIK (allP<0.05)in postoperative 3, 6mo, and 1y. In postoperative 1wk, 1, 3,6mo, and 1y, the CDVA were better with the ICL group than the FS-LASIK group (allP<0.05). In postoperative 1y, the safety index in the ICL group and the FS-LASIK group were 1.33±0.27 and 1.17±0.24, respectively. There were no patients lost 1 or more lines of CDVA in both groups, but 21 eyes(43.75%) and 18 eyes (31.03%) gained 1 line of CDVA in the ICL group and the FS-LASIK group, respectively. Totally 19 eyes (39.58%) and 16 eyes (27.59%) gained 2 or more lines of CDVA, respectively. Totally 8 eyes (16.67%) and 24 eyes(41.38%) remained unchanged of CDVA, respectively. In postoperative 1y, the efficacy index in the ICL group and the FS-LASIK group were 1.28±0.22 and 1.13±0.26, respectively.Forty eyes (83.33%) and 45 eyes (77.59%) had a UDVA of 20/20 or better in the ICL group and the FS-LASIK group,respectively. Totally 25 eyes (52.08%) and 29 eyes (50.00%)had a UDVA of 24/20 or better, respectively.
Refractive OutcomesBased on the data presented in Figures 3,4, and Table 3, in the ICL group, no significant difference of spherical equivalent was found between postoperative time points (P>0.05), while in the FS-LASIK group, significant change of spherical equivalent was observed shift from hyperopia to myopia, it suggested that ICL implantation provides better refractive stability than FS-LASIK for the high myopia correction. The changes of spherical equivalent in the ICL group from 1wk to 1y postoperatively were -0.12±0.37 D,in the ICL group, spherical equivalent within ±0.50 D was achieved in 97.92% (47 eyes) of the eyes, within ±1.00 D was achieved in 100% (48 eyes) of the eyes, while the changes of spherical equivalent in the FS-LASIK group from 1wk to 1y postoperatively were -0.79±0.58 D, in the FS-LASIK group,spherical equivalent within ±0.50 D was achieved in 68.97%(40 eyes) of the eyes, within ±1.00 D was achieved in 98.28%(57 eyes) of the eyes, the changes of spherical equivalent were statistically different between the ICL group and the FSLASIK group (P<0.05).
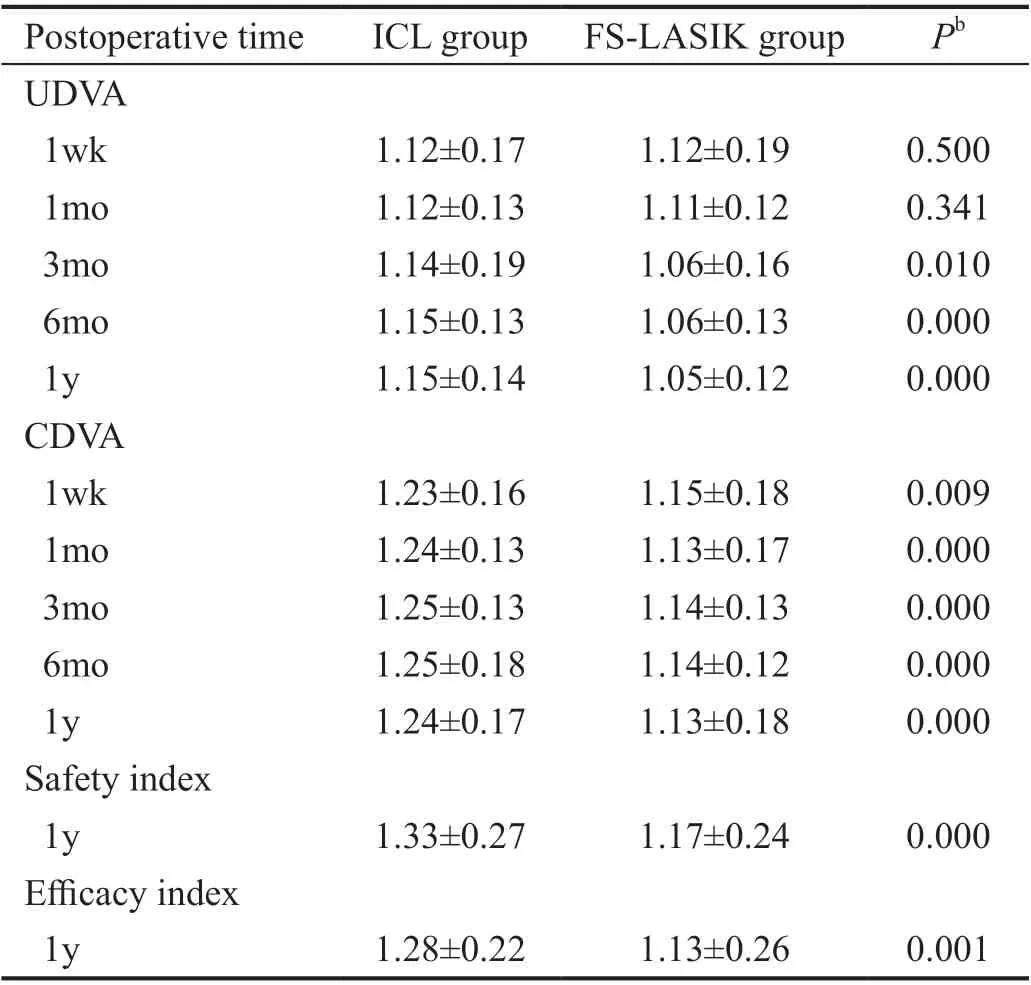
Table 2 Comparison of 1-year changes in vision after ICL implantation and FS-LASIK for the correction of high myopia
Objective Visual Quality ParametersOne-year changes in objective visual quality parameters in the two groups are compared in Figures 5, 6, 7, and Table 4. MTF cutoff frequency were higher with ICL implantation as compared to FS-LASIK (allP<0.05) in postoperative 1wk, 1, 3, 6mo,and 1y (Figure 5). With no statistically significant difference in SR between ICL implantation and FS-LASIK (P>0.05)in postoperative 1wk, but for postoperative 1wk, 1, 3, 6mo,and 1y, SR were higher with ICL implantation as compared to FS-LASIK (allP<0.05; Figure 6); OSI were higher with ICL implantation as compared to FS-LASIK (P<0.05) in postoperative 1wk, but OSI were lower with ICL implantation as compared to FS-LASIK (P<0.05) in postoperative 1mo, and with no statistically significant difference in OSI between ICL implantation and FS-LASIK (allP>0.05) in postoperative 3,6mo, and 1y (Figure 7).
DISCUSSION

Figure 3 Comparison of 1-year changes in refractive outcomes after ICL implantation and FS-LASIK for high myopia correction.

Figure 4 Comparison of 1-year proportions in refractive outcomes after ICL implantation and FS-LASIK for high myopia correction.
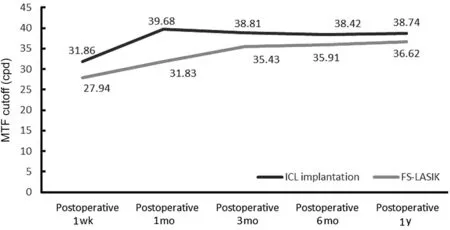
Figure 5 Comparison of 1-year changes in modulation transfer function cutoff after ICL implantation and FS-LASIK for high myopia correction.
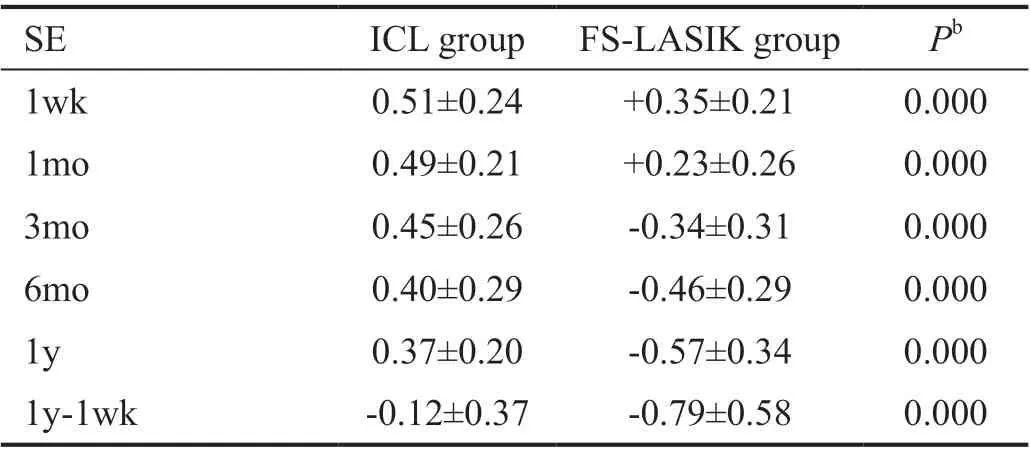
Table 3 Comparison of 1-year changes in refractive outcomes after ICL implantation and FS-LASIK for the correction of high myopia

Figure 6 Comparison of 1-year changes in strehl ratio after ICL implantation and FS-LASIK for high myopia correction.
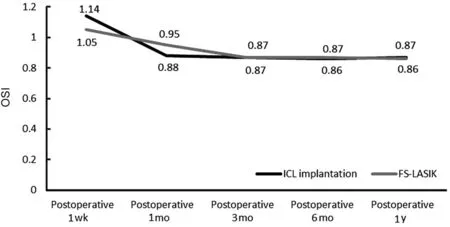
Figure 7 Comparison of 1-year changes in objective scatter index after ICL implantation and FS-LASIK for high myopia correction.

Table 4 Comparison of 1-year changes in objective visual quality parameters after ICL implantation and FS-LASIK for the correction of high myopia
High myopic errors can be corrected by different refractive surgeries such as ICL implantation and FS-LASIK. Basically,the FS-LASIK using a femtosecond laser to create a corneal flap, then utilizes an excimer laser to ablate stromal tissue after lifting the corneal flap to correct myopia. The whole ablation procedure is analogous to a lens fabrication in the corneal.FS-LASIK is effective in correcting low to moderate myopia,but the corneal nerve is damaged when the cornea is ablated,which increases the incidence of dry eyes after surgery[10].Other studies[11]reported that corneal refractive surgery have disadvantages in safety, efficacy and visual quality, and the risk of postoperative refractive regression and keratoconus also increases with the increase of the diopter. ICL is a reversible posterior chamber phakic intraocular lens (IOL) fixed in the ciliary sulcus. Unlike FS-LASIK, ICL can be exchanged if unexpected refractive changes occur after surgery. Some studies[12-13]have demonstrated that ICL implantation has the potential to substitute current laser refractive surgeries due to the high optical and visual quality of the ICL implantation.If the cornea is thick enough, both ICL implantation and FSLASIK can safely and effectively correct high myopia no more than -12.00 D. Therefore, we used direct between-groups comparison in this research to compare the subjective and objective visual quality of both procedures for high myopia correction, to detect which procedure have more advantages in high myopia correction. This provides a reference for patients with high myopia to select the best surgical procedure.
Visual Acuity and Refractive OutcomesSeveral studies[14-16]compared the effects of LASIK with mechanical microkeratome and ICL implantation for myopia correction.The results in those studies suggest that ICL implantation provides better UDVA and CDVA outcomes than LASIK with mechanical microkeratome for the high myopia correction.Although we compared ICL implantation and FS-LASIK,our results were similar to those of the above studies: For postoperative 3mo, UDVA were better after ICL implantation than after FS-LASIK. CDVA were better with the ICL group than the FS-LASIK group at each postoperative follow-up stage. In postoperatively, the safety index in the ICL group and the FS-LASIK group were 1.33±0.27 and 1.17±0.24,respectively; the efficacy index in the ICL group and the FSLASIK group were 1.28±0.22 and 1.13±0.26, respectively.ICL implantation provided better safety index and efficacy index than FS-LASIK for high myopia correction. There were no patients losing 1 or more lines of CDVA in both groups.The proportion of preoperative visual acuity improvement and the proportion of 20/20 visual acuity were better with the ICL implantation than FS-LASIK. It suggests that both ICL implantation and FS-LASIK procedures provide good safety and predictability when the cornea is thick enough,but ICL implantation possesses better clinical outcomes than FS-LASIK for the high myopia correction. In the ICL group, no significant difference of spherical equivalent was observed between postoperative time points, while in the FSLASIK group, significant change of spherical equivalent was observed shift from hyperopia to myopia. It suggested that ICL implantation provides better refractive stability than FSLASIK.
The reason why both procedures have different clinical outcomes is FS-LASIK procedure ablates stromal tissue in the central corneal, which changes the aspheric shape of the cornea[17], and the corneal wound healing process also makes the surface of corneal flap and the stromal tissue not smooth,which cause an increase in higher-order aberrations (HOAs)after FS-LASIK, especially spherical aberration[18]. While ICL implantation was considered to induce fewer HOAs than FS-LASIK, and possesses better optical and visual quality than FS-LASIK, it does not ablate the cornea and leave the central corneal untouched during the whole procedure[19].ICL implantation provides better refractive stability than FSLASIK. The wound healing process of corneal flap and stromal tissue may contribute to corneal thickness increased after FSLASIK[9], which makes UDVA shift from hyperopia to myopia after FS-LASIK. While ICL implantation only makes a 3 mm limbal corneal incision, which is far from the central optical zone. So the wound healing process of the incision hardly affect the refractive stability after ICL implantation[20].
Objective Visual Quality ParametersIn our study, after postoperative 1mo, all the optical and visual quality indices showed better outcomes in ICL implantation than FS-LASIK,which proves excellent optical and visual quality after ICL implantation.
The main reason ICL implantation possesses better optical and visual quality than FS-LASIK is that FS-LASIK induces more high-order aberrations (HOAs) than ICL implantation[18]. The specific reasons are as follows: 1) The tear film is unstable:the corneal nerve is damaged during FS-LASIK process,which makes corneal sensation decreased[21]and tear film not equally distributed. Tear film stability damaged can lead to the HOAs of corneal anterior surface increased. 2) Corneal flap:the corneal flap will be exposed to the air during FS-LASIK process, which causing hypoxic edema of corneal epithelial cells and corneal transmittance decreased, thereby increasing HOAs[22]. 3) Laser ablation: stromal tissue ablation by excimer laser correct the lower-order aberrations (LOAs), but changes the aspheric shape (the cornea is steep in the center but flat in the peripheral) of the cornea and optical property at the same time, which induced certain HOAs inevitably, and the quantity of HOAs is positively correlated with the ablation depth[16]. 4)Inflammation stimulation: the presence of tissue debris under the flap, corneal lamina reaction, vacuum aspiration, and overwash under the flap can also lead to increased postoperative HOAs[23]. 5) “Edge” effect: the difference in light refraction ability between the center and the edge of the lens results in spherical aberration, which occurs due to the increased refraction of light rays when they irradiate a lens near its edge.In comparison with those that irradiate close to the center, in other words, light passes through the edge of the lens, which gives rise to spherical aberration. We speculate that FS-LASIK may induce more spherical aberration mainly because the additional lens is in the corneal (ahead of the pupil). When the light passes through the edge of the additional lens, pupil cannot block the light which may induce spherical aberration.While ICL is behind the pupil which can block most light from passing through the edge of the lens, ICL implantation should induce less spherical aberration than FS-LASIK, and thus create less intraocular scattering. This hypothesis can also explain why patients after FS-LASIK are more likely to have poor vision at night, glare, and other visual symptoms. This is because the pupil dilates at night, and light is more likely to pass through the edge of the lens, resulting in more spherical aberration and decreased visual quality. The hypothesis in the present study are supported by Mok and Lee[24]which revealed that higher order aberrations was reduced as optical zone diameter was increased. This is because of the larger optical zone, the easier it is for the pupil to cover the edge of the optical zone. Less light passes through the edge of the lens which induce less HOAs.
In summary, more HOAs introduced after FS-LASIK than after ICL implantation, as well as the corneal wound healing process after FS-LASIK, which led to ICL implantation possesses better clinical outcomes and refractive stability than FS-LASIK for the high myopia correction. In addition,large pupils tend to introduce more spherical aberration, so patients should be strictly selected before refractive surgery. It is suggested that patients with large pupil should choose ICL implantation, so as to avoid visual quality problems caused by FS-LASIK.
A limitation of the research is that aberrations are closely linked with patient age, tear film, and intraocular pressure. In the future, more research could be utilized to find out how the visual quality was impacted by the patient age, tear film, and intraocular pressure.
ACKNOWLEDGEMENTS
Foundation:Supported by the Research Grant of Hunan Provincial Health Commission Project (No.C2017037).
Conflicts of Interest:Jiang Z,None;Wang H,None;Luo DQ,None;Chen J,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
