Addressing the MSlCS learning curve: identification of instrument-holding techniques used by experienced surgeons
Alexandra J. Berges, Zervin R. Baam, Angela Zhu, Shameema Sikder,, Samuel Yiu,,4,Ravilla D. Ravindran, Kunal S. Parikh,,4,5,6
1Johns Hopkins University School of Medicine, Baltimore,MD 21287, USA
2Aravind Eye Hospital, Madurai, Tamil Nadu 625001, India
3Wilmer Eye Institute, Baltimore, MD 21287, USA
4Center for Nanomedicine, Baltimore, MD 21231, USA
5Department of Biomedical Engineering, Baltimore, MD 21218, USA
6Center for Bioengineering Innovation & Design, Baltimore,MD 21218, USA
Abstract
● KEYWORDS: cataract; manual small incision cataract surgery; instrument holding; training; learning curve
INTRODUCTION
Untreated cataract is the primary cause of preventable blindness, leading to visual impairment in 35.1 million individuals, and contributing to 33.4% of blindness worldwide[1]. There are an estimated 20 million people with preventable blindness due to cataract, heavily skewed towards low- and middle-income countries (LMICs) due to lack of access to surgical treatment[2]. The use of manual small incision cataract surgery (MSICS) has grown in popularity in comparison to phacoemulsification in LMICs because it is more time- and cost-efficient, requiring less time, capital equipment investment, and maintenance costs, while achieving excellent visual outcomes and low complication rates[3]. A study on the outcome of 593 cataract surgeries performed at the Aravind Eye Hospital utilizing MSICS reported an average time of 3.75min, with a best corrected visual acuity of greater than or equal to 6/18 achieved in 94% of patients[3].High volume eye care systems in LMICs have leveraged this efficient, high quality, low cost approach to cataract surgery in order to increase cataract surgical volume and enable increased access to patients. Moreover, MSICS has advantages over phacoemulsification in the surgical management of mature cataracts, which are more prevalent in LMICs. In particular, MSICS allows surgeons to avoid the amount of phacoemulsification energy required to fragment dense cataracts, which can damage to the corneal endothelium and zonular fibers, and lead to further complications[4].
Despite the surgical benefits of MSICS and training programs which include lectures, surgical observation, and handson wet lab training, the steep MSICS learning curve has led to reports of suboptimal trainee cataract surgery outcomes across LMICs[5]. Complication rates amongst trainees at various institutions range from 2.6%-30.9% with common complications including posterior capsular rent and zonular dialysis[5-8]. One retrospective study at Sankara Eye Hospital in Chennai, India found that overall complication rates were most prevalent in the first month of training (44.4%) and declined to 21.9% after three months of training[8]. At the Aravind Eye Hospital, specifically, residents performing their first 100 MSICS procedures were more than three times more likely to encounter an intraoperative complication than residents who had performed at least 600 procedures[6]. Finding ways to improve MSICS training provides a high leverage opportunity to both increase cataract surgical rates and improve patient outcomes.
Cataract surgery is performed under a microscope and requires small instruments and precise movements, providing a low margin of error during manipulation of fragile ocular tissue in a confined area. Compared to the extracapsular cataract extraction procedure, MSICS involves more maneuvers in the anterior chamber, specifically during capsulotomy, while dislodging the nucleus from the posterior to anterior chamber,and extracting the nucleus through the scleral tunnel[9-10]. The importance of proper hand positioning is recognized by most experienced surgeons, as mastering instrument handling is critical for stable and precise manipulation of ocular tissue through microincisions during surgery[10]. However, existing MSICS training programs and methods are limited in their capacity to instruct and help trainees gain confidence with optimal hand positioning. Most training programs instruct trainees to use the “most comfortable position” or a “pencil grip”, but do not offer specific, validated hand position options for new surgeons. Moreover, didactic surgical videos do not capture proper hand positioning exhibited by the surgeons,as their hands are outside of the field of view of the operating microscope. Trainees often utilize wet labs to acquire dexterity with technical hand positioning skills, including simulators andex vivomodels. Wet-laboratory training has been proven as an effective method of reducing occurrence of posterior capsule rupture and vitreous loss, but not tunnel or iris complications[11], possibly because existing training tools are not able to fully replicate true surgical conditions and constraints[12]. Just as incoming trainees benefit from access to robust, tested, and standardized surgical protocol and instruments, we hypothesize that trainees will benefit from access to a set of validated hand positions that can inform their own techniques. To date and to our knowledge, there has not yet been a study focused on identifying optimal hand position techniques utilized by experienced MSICS surgeons. Thus, theobjective of this manuscript is to provide insights into clinical best practices and to identify instrument holding archetypes used by experienced surgeons at the Aravind Eye Hospital in order to develop a universal language and set of validated techniques that can be utilized in MSICS curricula.
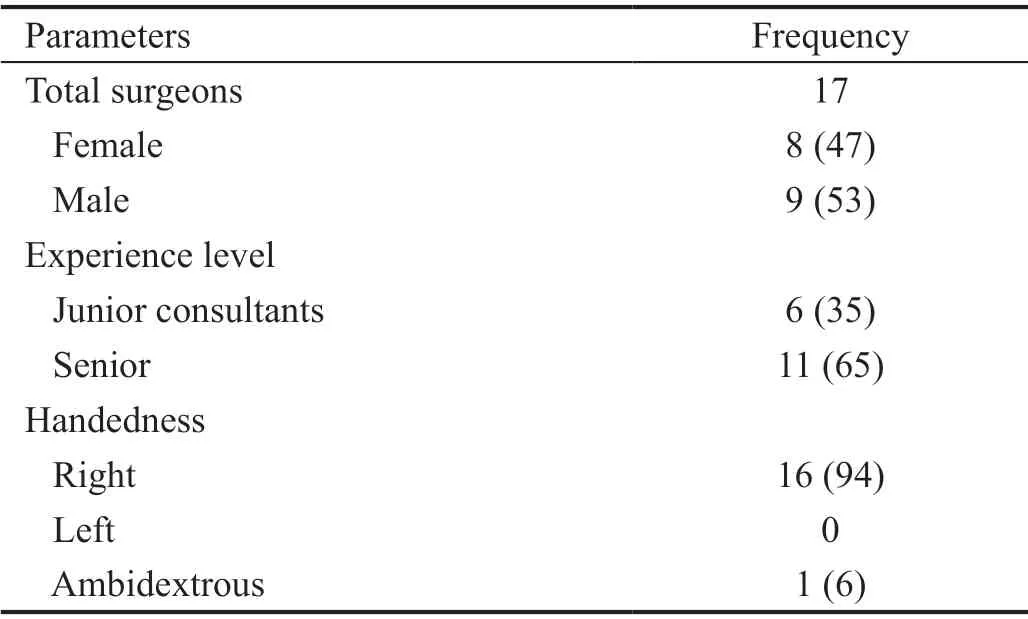
Table 1 Surgeon characteristics n (%)
MATERIALS AND METHODS
SurgeonsObservations took place in the wet lab at the Aravind Eye Hospital in Madurai, India, and were determined to be exempt by the Johns Hopkins Medicine Institutional Review Board. At Aravind, cataract surgeon experience level corresponds to the number of MSICS surgeries that a surgeon has performed to enable proficiency in various types of cataracts. An average junior consultant requires between 700 and 1000 MSICS surgeries to handle uncomplicated cataracts,and then another 1000 to 1200 surgeries to become better at handling mature cataracts. Senior surgeons have the experience and skill to perform most complex surgeries, including traumatic cataracts, cataracts with gross phacodonesis, and secondary IOL procedures. We observed the hand positions of junior consultants and senior surgeons (n=17) in the Cataract and Cornea Departments at Aravind. Sixteen surgeons were right handed and one was ambidextrous. Surgeon information is listed in Table 1.
Data CollectionThe experimental set up in the Aravind Eye Hospital Simulation Center was designed to approximate an operating theater. Each surgeon performed five MSICS steps(scleral incision, scleral tunnel, side port, corneal tunnel, and capsulorhexis) utilizing a crescent blade, keratome blade,side port blade, forceps, and cystitome (Aurolab, Madurai,India) onex vivogoat eyes under a dissecting microscope.Images and videos were taken during each step to record surgeon finger and hand positions. Surgeons were also asked to describe their pencil holding technique, classified within the framework of four grasp patterns that have been recognized as appropriate for mature writing: Dynamic Quadripod, Dynamic Tripod, Linear Quadripod, and Linear Tripod[13]. Information was collected about each surgeon’s experience level, glove size, and handedness. Summary statistics showing the numberof surgeons using each described hand position technique were calculated.

Table 2 Summary of commonly used archetypes and modifying factors for five MSICS steps
Statistical AnalysisFollowing data collection, surgeons’ hand position patterns were assessed, noting common features such as number of fingers placed on the instrument, degree of finger flexion, and finger contact on the instrument. Techniques were classified based on major archetypes, representing fundamental differences in instrument handling technique. Modifying factors were also identified, representing the amount of flexion in the index finger used to maneuver the surgical tool.Index finger “flexion” was considered in cases of proximal interphalangeal (PIP) joint flexion towards the palm of the hand greater than 30 degrees and distal interphalangeal (DIP)joint extension. Index finger was considered “straight” in cases of simultaneous PIP and DIP joint extension. Finally, index finger was considered “bent” in cases of simultaneous PIP and DIP joint flexion towards the palm less than 30 degrees.This nomenclature was verified with ophthalmologists at the Wilmer Eye Institute at Johns Hopkins University and at Aravind, through a review of the de-identified photos and videos. Illustrations of primary instrument handling archetypes were developed using Adobe Illustrator CC 2019 (version 23.0.1, Ventura, CA, USA) using photos taken of a surgeon’s hand, and traced within the graphic-driven software.
RESULTS
Common Archetypes and Modifying FactorsFor each MSICS step, common archetypes and key modifying variables utilized by experienced surgeons were identified, as shown in Table 2. Factors considered in describing hand positions included number of fingers used to support the instrument,distance between fingers along surgical instrument shaft, the degree of finger flexion, and utilization of the non-dominant hand. Key differences included thumb placement and number of fingers supporting the instrument (quadripodvstripod).Modifying variables included index finger curvature and amount of flexion.
Scleral IncisionThe scleral incision step is performed with a crescent blade angled downward at one-third to one-half scleral depth, in a frown-shape.The frown shape is difficult to make for a beginner compared to a straight incision,because the groove must be made with one smooth hand movement. However, it ensures minimal astigmatism and is the preferred incision type for most cataract surgeons[14].In an analysis of resident-performed MSICS, the most commonly noted complication (33%), was intraoperative wound leak,emphasizing the necessity of meticulous wound construction in MSICS[15]. The primary archetypes included quadripod and tripod, in which four fingers (thumb, index, middle, ring) and 3 fingers (thumb, index, and middle) are used respectively(Figure 1). The identified modifying factors describe the degree of flexion of the dominant index finger. In ‘flexed index’, the index finger is flexed with most pressure on the middle of the fingertip. In ‘straight index’ the index finger is straight with the entire fingertip contacting the crescent blade. In ‘curved index’the index finger is slightly curved with most pressure exerted on the distal fingertip.

Figure 1 Hand position archetypes and modifying factors for scleral incision step.
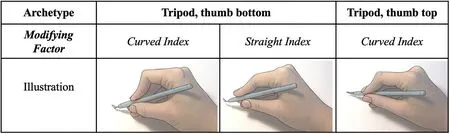
Figure 2 Hand position archetypes and modifying factors for scleral tunnel step.
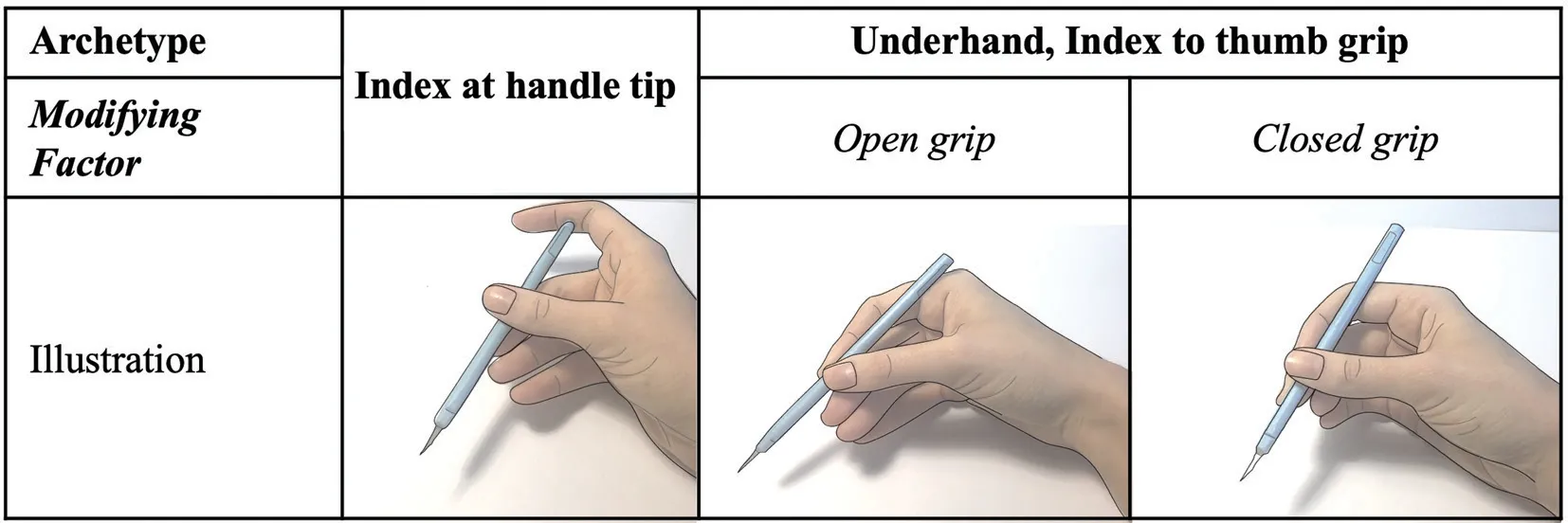
Figure 3 Hand position archetypes and modifying factors for side port incision step.
Scleral TunnelA scleral tunnel is subsequently constructed using an angled crescent blade point upwards, with the incision extending approximately 2-2.5 mm into the cornea. In a selfreported assessment of MSICS difficulty, tunnel construction was rated as the second most difficult step, which may be due to the coordinated “wriggling motion” necessary to create a funnel-shaped pocket[16]. The wriggling movements could be achieved by 1) using the thumb and index finger at the same instrument level while using the third finger for support; 2)moving the hand back from the crescent tip; or 3) keeping the instrument tip perpendicular to the orbit upon entry. The primary archetypes consisted of a tripod position with thumb placed either on the top or the bottom of the crescent blade shaft (Figure 2). In both positions, the thumb, index, and middle finger are used to support the crescent blade, however in the top position the thumb is placed 90° from the index finger on the side of the instrument. In the bottom position,the thumb is placed 180° from the index finger on the bottom of the instrument. The observed modifying factors describe the degree of flexion of the index finger. In ‘straight index’ the index finger is straight with the entire fingertip contacting the crescent blade. In ‘curved index’ the index finger is slightly curved with most pressure exerted on the distal fingertip.
Side PortPerforming a side port involves creating a paracentesis temporally with a myringotomy or similar blade in the peripheral cornea. The primary archetypes included holding the index finger at the handle tip, with the index finger placed at the end of the instrument, and index to thumb grip, with the index finger opposing the thumb to support and stabilize the instrument (Figure 3). Modifying factors included‘open grip’ and ‘closed grip.’ In the open grip, the instrument is gripped between thumb and index fingertips with the thumb curved to apply pressure with distal thumb fingertip. In the closed grip, the index is gripped between the thumb, index, and middle fingers, with the thumb flexed to apply pressure using the entire fingertip. In order to pass the cannula straight into the same wound previously created, some surgeons suggested estimating the optimal plane of entry prior to angling the instrument towards the orbit.
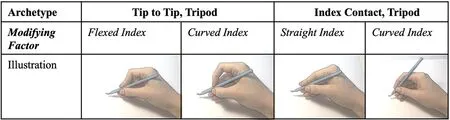
Figure 4 Hand position archetypes and modifying factors for corneal entry step.
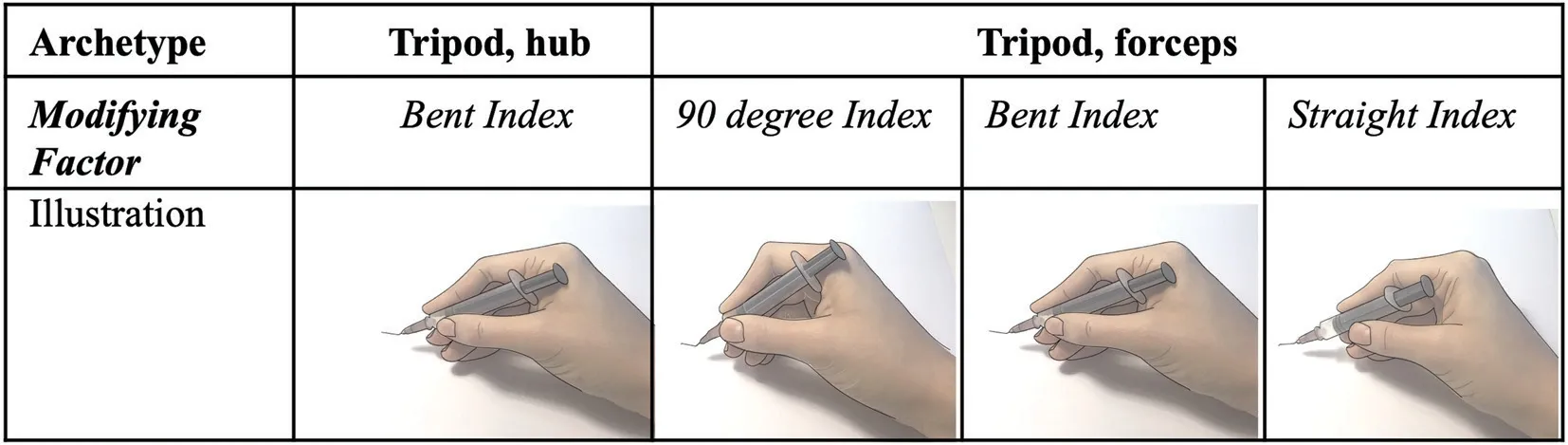
Figure 5 Hand position archetypes and modifying factors for the capsulorhexis step.
Corneal EntryThe corneal entry step involves using a keratome to enter the anterior chamber, directed to include the dissected area from the scleral tunnel. There is difficultly associated with holding the keratome so that corneal entry is not ragged. The major archetypes included tripod ‘tip to tip’and ‘index contact’ (Figure 4). ‘Tip to tip’ involved use of the thumb, index, and middle finger to support the keratome primarily with the index and thumb fingertips in opposition.‘Index contact’ involved use of the thumb, index and middle finger, with the length of the index finger to support the instrument, along with the thumb fingertip. The observed modifying factors involved flexion of the index finger,including flexed, curved, and straight variants.
CapsulorhexisThe continuous curvilinear capsulotomy(CCC) is performed either through the paracentesis to reduce viscoelastic leakage or the scleral incision to allow for more maneuverability. Once an initial flap has been lifted, this is extended in a continuous manner until the entire capsulorhexis is completed, ideally 6-8 mm in diameter. The step is performed using a capsulotomy needle. In a study of resident perceived difficulties in cataract surgery cases, performing a capsulorhexis was identified as a challenging step, particularly in MSICS because the rhexis must be larger compared to phacoemulsification[17]. To address this, surgical capsulorhexis simulation involving instrument handling with extensive anti-tremor training, bimanual navigation and capsulorhexis technique has been shown to improve complication rates among resident cataract surgeons[18]. The major archetypes(Figure 5) describe the use of the non-dominant hand to either support the keratome or stabilize the incision site. Each position uses the thumb, index, and middle finger to support the keratome. In one variation, the non-dominant hand index finger is placed on the hub for support. Alternatively, the nondominant hand uses forceps to hold the orbit in place. The observed modifying factors involved flexion of the index finger, including 90°, where most pressure is applied on the fingertip, slightly flexed, and straight, where the entire index finger length contacts the instrument for support.
DISCUSSION
The current method of teaching new surgeons how to hold instruments for ophthalmic surgery involves instructing trainees to pick the most comfortable position. Selecting an instrument holding technique is quite variable and individualized. Most surgeons use their pencil grip position,while others learn the specific technique used by their trainer and modify for their own comfort. Some find it more difficult to identify a suitable position and observe many experienced surgeons until identifying an instrument holding technique that causes the least fatigue and best surgical outcomes.
This work aimed to describe a set of validated hand positions for MSICS that could allow trainees to practice instrument holding techniques in an informed manner in a simulation setting. In the present study, cataract surgeons from Aravind Eye Hospital of varying experience levels exhibited their instrument holding techniques across five MSICS steps using animal eyes to mimic human tissue properties. Hand positions were described using major archetypes, which remained consistent within each subset of surgeons, and minor modifying factors which displayed more variability.
As all observations were conducted at a single site, additional validated archetypes likely exist at different institutions. We focused on particular MSICS steps involved in wound creation and capsulorhexis, components of the surgery that are practiced in simulation and have been shown to contribute significantly to the resident learning curve and complications[14-20].
For scleral incision, quadripod technique may be appropriate for surgeons utilizing four fingers in their typical pencil grasp.The additional fourth finger placed on the instrument allows for increased stability, but decreased ease of movement inside the eye. The use of the 4thfinger on the instrument shaft also decreases its utility in stabilizing the movement on the table.The tripod technique may be appropriate for a surgeon using a‘tripod’ pencil grasp. As compared to quadripod grip, the tripod grip allows for increased ease of movement inside the eye.Additionally, during scleral incision, while senior surgeons used flexed, curved and straight index fingers 45%, 36%, and 18% respectively, 100% of the junior surgeons used a flexed index finger, demonstrating a possible marker for expertise.
For scleral tunnel, the thumb bottom approach was most commonly used, which features an open web space technique.This allows the surgeon to use all intrinsic muscles of the hand,thus enabling control and precision during surgery. In contrast,for the side port step, the index to thumb grip was the most common archetype, likely due to the increased stability and control while creating the paracentesis using this oppositional grip. In contrast, the index at handle tip method may lead to aberrant movements and is more dependent on hand size and finger flexibility.
Overall, modifying factors for scleral incision, scleral tunnel,corneal entry, and capsulorhexis described the flexion of the index finger on the instrument, leading to differences in the magnitude and location of pressure applied to the tool shaft.Increased flexion may limit mobility and increase fatigue after many hours of surgery, however this modification may also help to increase stability for a surgeon with smaller hands or struggling with tremor during a particular step. A curved index finger involves most pressure placed on distal fingertip,which may limit stability and smoothness of movement,however decreased flexion leads to increased ease of mobility.In contrast, straight index finger involving pressure applied in the central fingertip facilitates controlled movements inside the eye and the lack of prolonged flexion during surgeries may lead to decreased fatigue over time.
Particularly for the capsulorhexis step, keeping the index finger bent may prevent unnecessary movements while also not placing too much strain on the joint. For this step, 45%and 18% of senior surgeons held their index straight and bent,respectively, compared to 17% and 50% of junior surgeons.Many surgeons fixed the index finger at a right angle, which may lead to fatigue if sustained for a long time. However,for a surgeon struggling with aberrant movements during the capsulorhexis step, it may be helpful to fix this joint to prevent extra motions. Finally, use of the non-dominant hand during the capsulorhexis step to provide hub support may be advantageous for inexperienced surgeons who have difficulty with tremor or aberrant movements during capsulorhexis.
For corneal entry, major archetypes differed in the grip type,either utilizing a tip to tip method of the opposing index finger and thumb, or utilizing index contact with the instrument. The increased index contact may increase mobility, which would be advantageous for surgeons struggling to enter the anterior chamber without tremor. During the corneal entry step, 55% of senior surgeons held their index finger in the straight position,compared to 17% of junior surgeons, who most commonly performed the step with a curved index finger (67%).
Notably, we observed that trainees often overcome specific challenges of MSICS through various modifications to hand position. For example, one challenge for trainees is maintaining anterior chamber depth because the incision size is large compared to a phacoemulsification procedure.Thus, many surgeons associate optimal hand positions with decreased pressure applied to the posterior lip, which leads to minimized anterior chamber collapse. To make small movements, surgeons may move fingers proximally on the instrument to avoid impediment of the visual field. To enable free movement inside the anterior chamber, experienced surgeons often hold the instrument lightly, with only the first three fingers. Furthermore, some only use the third finger on the instrument for support alone, rather than to facilitate movement of the tip. During training, tremor can be limited by means of stabilization using the 4thand 5thfinger on the patient’s head. These described findings and nomenclature will provide structured terminology to enable trainers to discuss technical aspects of instrument holding technique during didactics and intraoperative instruction.
Future directions include the potential to utilize information about validated hand positions to improve training and MSICS outcomes among trainees. This work could be used to develop training materials to allow trainees to intentionally select and test different hand positions in an informed manner. Additionally, intraoperative video camera recording would allow for assessment of instrument holding technique in a surgical setting to guide future training. Further characterization of variations in hand position could influence ophthalmic surgical instrument design individualized to surgeon factors. Finally, future studies comparing the clinical outcomes and complications associated with different MSICS instrument holding techniques could improve training and inform best practices in the field.
ACKNOWLEDGEMENTS
The authors acknowledge Dr. Aswin P. R. for coordination at the Aravind Eye Hospital, Dr. Sam Reiter and Dr. Grayson Armstrong for clinical insights into the difficulties experienced by MSICS trainees, Ms. Jemima David for use of the wet lab simulation center at Aravind Eye Hospital, and Johns Hopkins School of Medicine Dean’s Summer Research Program for financial support for the research.
Foundations:Supported by Dana Center for Preventative Ophthalmology, Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore, Maryland 21287;Johns Hopkins School of Medicine Dean’s Summer Research Funding, Johns Hopkins University School of Medicine,Baltimore, Maryland 21205-2196.
Conflicts of Interest:Berges AJ,None;Baam ZR,None;Zhu A,None;Sikder S,None;Yiu S,None;Ravindran RD,None;Parikh KS,None.
 International Journal of Ophthalmology2021年5期
International Journal of Ophthalmology2021年5期
- International Journal of Ophthalmology的其它文章
- Comprehensive evaluation of intravitreal conbercept versus half-dose photodynamic therapy for chronic central serous chorioretinopathy
- Lipid accumulation and protein modifications of Bruch’s membrane in age-related macular degeneration
- Via pars plana anterior iris enclavation lOL fixation
- Role of microRNA-25 in high glucose cultured Müller glia
- Protective effects of piperine on the retina of mice with streptozotocin-induced diabetes by suppressing HlF-1/VEGFA pathway and promoting PEDF expression
- Expression levels of pro-inflammatory interleukin-8 and certain antimicrobial peptides in concurrent with bacterial conjunctivitis
