Does shifting to professional emergency department staffing affect the decision for chest radiography?
Marin Pavlov, Lucija Klobučar, Iva Klobučar, Kristina Žgela, Vesna Degoricija,4
1 Department of Cardiology, Sestre Milosrdnice University Hospital Centre, Zagreb 10000, Croatia
2 Institute of Emergency Medicine, Osijek-Baranja County, Osijek 31000, Croatia
3 University of Zagreb School of Medicine, Zagreb 10000, Croatia
4 Department of Medicine, Sestre milosrdnice University Hospital Centre, Zagreb 10000, Croatia
KEYWORDS: Chest radiography; Emergency department; Emergency physicians; Healthcare organization
INTRODUCTION
Until late 2010, emergency departments (EDs) in Croatia providing care to internal medicine (non-surgical)patients were run by internal medicine specialists (IMSs),often by physicians with non-emergency subspecialties.In general, EDs were subdivided into particular specialty services, and served as “acute clinics” with on-duty physicians rotated in and out.[1]Since joining the European Union in 2013, legislation and practice in Croatia have changed. In April 2009, the European curriculum on emergency medicine, requiring a minimum training period of f ive years, was approved by Directive 2005/36/EC of the European Parliament.[2]Subsequently, a new specialization for emergency physician specialists (EPSs) was established,including trauma, neurology, pediatrics, and ultrasound training. Numerous EDs around the country shifted from specialty outpatient clinics to general EDs operated by EPSs. Compared with previous non-professional teams(who were not dedicated solely to ED work due to their numerous duties within their subspecialties, particularly in tertiary centers), EPSs tend to be more involved in structural improvements, inclined to the standardization of workup and treatment, and enthusiastic in accomplishing new ED-related skills (especially the use of ultrasound). However, a concern emerged about whether the shift to EDs run completely by EPSs would lead to unnecessary investigations due to a lack of experience. This was expected to become most obvious in radiologic examinations, which were abundant.[3,4]We hypothesized that shifting to professional ED teams would initially lead to higher rates of radiologic workup during ED visits.
METHODS
The study was conducted in the ED of a tertiary teaching University Hospital Center (UHC). The UHC is situated in a one-million-inhabitant capital, and provides emergency medical services for an urban population of approximately 350,000. There is a “no refusal” strategy for citizens outside the referral area, as well as for patients with no insurance policy. The daily turnover within the ED is approximately 300 visits in total, and 80 of them are in the internal medicine ED. The service is organized in a 24-hour shift with one physician being in charge and two additional physicians(internal medicine or subspecialty residents) helping out with examinations. A consulting cardiologist, gastroenterologist,nephrologist, and intensivist are available 24 hours every day. All workup, treatment, and admittance decisions are made by the physician in charge.
There were two enrollment periods for our study. From December 21, 2012 to January 5, 2013, 1,000 consecutive patients (“all-comers”) examined within the internal medicine ED were enrolled as group 1 (G1). During this enrollment period, all patients were examined by an IMS with at least f ive years of work experience. These physicians were subspecialists in different fields of internal medicine.However, they all lacked structured education in the field of emergency medicine. The second enrollment period was from December 21, 2018 to January 3, 2019, in which additional 1,000 consecutive patients were enrolled as group 2 (G2). These patients were examined by an EPS with average two years of work experience, and five-year structured training in all fields of emergency medicine including trauma, emergency anesthesia, and resuscitation.A total of 51 G1 and 41 G2 patients were excluded from the study for various reasons. A propensity score matching was performed on the remaining 1,908 patients with the following matching variables: age, sex, dyspnea, cough,fever, and chest pain as leading symptoms (matching without replacement, match tolerance: 0.005). A total of 1,816 patients (908 in each group) entered the f inal analysis.
All the relevant demographic data, presenting signs and symptoms, as well as the workup and outcome details, were collected from digital medical archives. During workup,chest X-rays (CXRs) were performed upon indication of the specialist in charge. There were no written protocols on CXR indications. All CXRs were re-examined by an experienced intensivist who was blinded for the findings and patient details. If an original finding did not match the re-examination finding, the CXR was assessed by an experienced radiologist, and a consensus was sought. If no consensus was reached, the experienced radiologist’s f inding was used as def inite.
Statistical analysis
Descriptive data were presented as mean±standard deviation (SD) or medians and interquartile range (IQR).Categorical variables were presented as counts and frequencies. Categorical variables were analyzed by Chisquare or Fisher exact test and continuous variables by Mann-WhitneyU-test. Binary logistic regression was used to evaluate the relation of continuous variables and the tendency to perform CXR. The method was also used to create models to determine the independent contribution of different variables on the tendency to perform CXR, and for the CXR f inding to be pathological. The conditional forward stepwise approach was used. The regression results were used to generate receiver operating characteristic (ROC)curves to predict pathological findings. The optimal cutoff points were determined by using Youden’s index. Twotailed signif icance tests were performed, and aP-value <0.05 was considered significant. The statistical analyses were performed using SPSS for Windows, version 25 (IBM SPSS,Armonk, USA).
RESULTS
Slightly over half of the population was female (52.4%),with a mean age of 63 (45-76) years. After propensity score matching, there were no significant differences between the two groups regarding age, sex, and admittance rate,frequency of chest pain, fever, dyspnea, or cough as leading symptoms. CXR was performed in 40.6% of all patients.There was no difference in the frequency of CXR (38.9% in G1 vs. 42.3% in G2,P=0.152) or abdominal X-ray (14.4%vs. 14.8%,P=0.894), while comprehensive abdominal ultrasound (6.7% vs. 3.6%,P=0.004) and computed tomography (3.9% vs. 2.0%,P=0.025) were more often performed in G1. In brief, significantly more CXRs were performed in G2 in patients older than 65 years (Figure 1A),in female patients older than 65 years, in patients presenting during the evening and night shifts (between 4 p.m. and 8 a.m.) as well as during off-hours, in patients with a history of malignancy, in patients presenting with gastrointestinal(GI) bleeding, and in patients with bradycardia, but less in patients presenting with arrhythmia.
Overall, time spent in the ED was similar in the two groups (240 [161-371] minutes vs. 261 [154-413] minutes,P=0.198). Time spent in the ED was related to the frequency of CXR with logistic regression (odds ratio [OR]=1.115,95% conf idence interval [CI]1.087-1.144),P<0.001, Figure 1B). In the group of patients with CXR performed, time spent in the ED was longer for G2 patients (281 [185-424]minutes vs. 322 [197-496] minutes,P=0.011).
No difference in the rates of pathological CXR was found between the groups (47.3% in G1 vs. 52.2% in G2,P=0.186). The most common pathologies observed on CXR are shown in Figure 1C. The CXR finding was more often mentioned in the discharge letter in G1 (67.3% vs. 37.5%,P<0.001). This was true for both admitted (52.4% vs.2.3%,P<0.001) and discharged patients (68.7% vs. 55.1%,P<0.001). Lung rales and wheezing were more frequently reported in the clinical status in G1, and peripheral edema in G2 patients (Figure 1D). However, when only patients with CXR signs of congestion were analyzed, no difference was found (81.5% vs. 69.1% for rales,P=0.136; 7.7% vs. 7.3%for wheezing,P=1.000). In patients with cardiomegaly,rales were more often reported in G1 (64.4% vs. 47.5%,P=0.025), while the difference in reported rates of wheezing was not signif icant (10.9% vs. 5.0%,P=0.183).
Admittance rates were similar (23.8% vs. 22.4%,P=0.504). No difference in admittance to intensive and post-intensive care wards was detected (37.4% vs. 42.6%,P=0.317). The frequency of CXR in the two groups did not differ when the patients were stratif ied according to the type of ward (regular ward 61.2% vs. 67.2%,P=0.356; intensive and post-intensive care ward 50.0% vs. 57.0%,P=0.437).Among discharged patients, there were 78 repeated visits within 14 days (4.6% vs. 3.8%,P=0.355).
Antibiotics were more often prescribed in G1 (12.1%vs. 7.7%,P=0.003), and the difference persisted regardless of CXR (no CXR 8.0% vs. 4.8%,P=0.046; CXR performed 20.4% vs. 11.7%,P=0.005). On the contrary, no difference was found in prescribing diuretics at discharge,neither between the two groups in total nor when stratif ied against CXR.
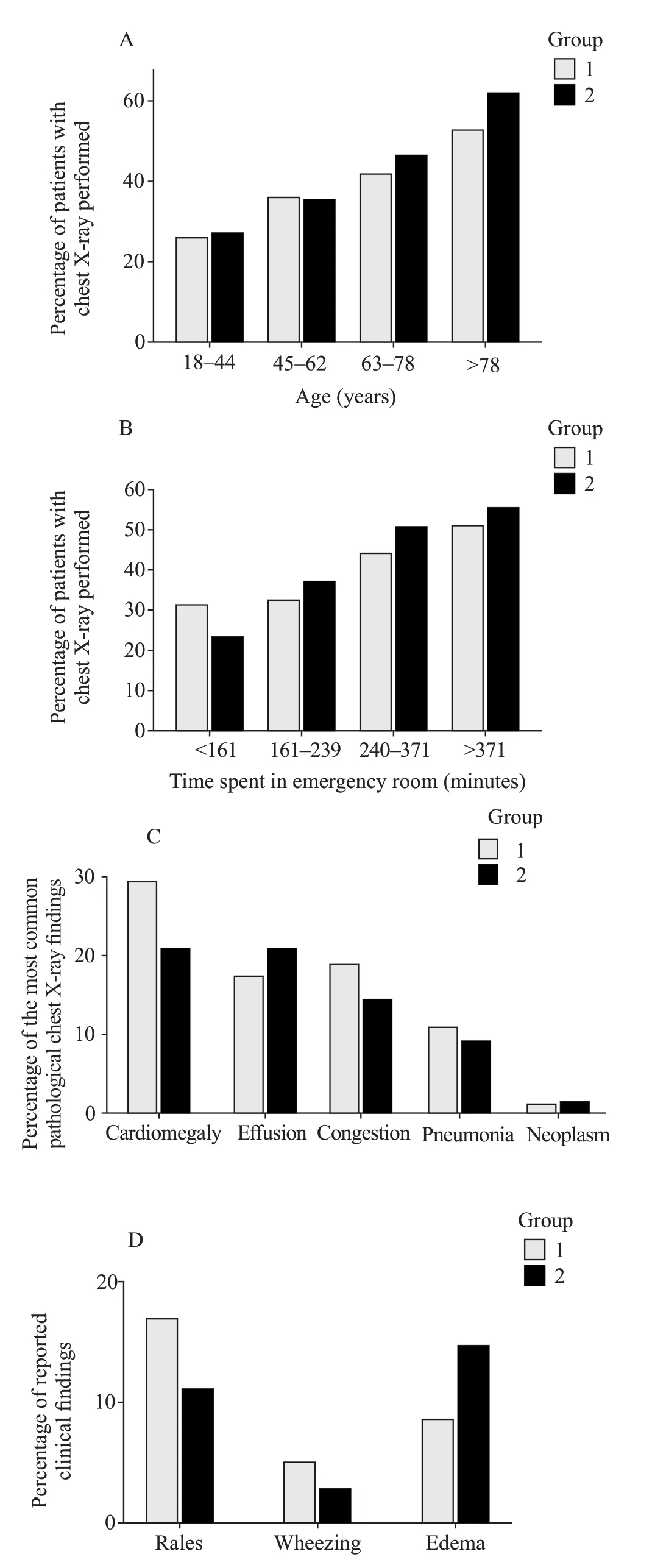
Figure 1. Comparisons between G1 and G2. Frequency of chest X-rays according to age (A) and time spent in the ED (B); G1 logistic regression: odds ratio (OR)=1.024, 95% confidence interval (CI)1.016-1.032; G2 logistic regression: OR=1.030, 95% CI 1.023-1.038;C: the most common pathological chest X-ray findings; D: rates of reported clinical f indings.
By using binary logistic regression with 22 variables included, two models to predict the tendency to perform CXR were created (Table 1). In addition, two models to predict pathological CXR findings are presented in Table 2. By using predicted probability for pathological CXR for each case, ROC curves were plotted (G1: area under the curve 0.877±0.018,P<0.001, 95%CI0.841-0.913,sensitivity 78.4%, specificity 82.2%; G2: area under the curve 0.785±0.023,P<0.001, 95%CI0.740-0.830,sensitivity 72.1%, specif icity 72.7%).
Similar number of patients died within ED during workup (0.9% vs. 1.4%,P=0.452). Among the discharged patients, five (0.2% vs. 0.3%,P=1.000) died within 30 days of ED discharge. Intra-hospital and 30-day mortality for admitted patients were comparable (9.8% vs. 11.8%,P=0.498; 10.2% vs. 12.3%,P=0.501). Rates of CXR examinations did not differ between the two groups when analyzed against outcome (survivors 38.6% vs. 42.0%,P=0.149; non-survivors 58.3% vs. 70.0%,P=0.675).
DISCUSSION
In this single-center retrospective observational study,shifting from IMSs to EPSs within the internal medicine ED section did not affect the CXR rate. This disputes our hypothesis, which was based on the acknowledged differences in the levels of experience and education between EPSs and IMSs in the field of internal medicine.No difference was observed in patients with common highrisk factors such as hypotension, dyspnea, chest pain, or lower Glasgow Coma Scale. The possible explanation for this uniformity of workup for severe patients is that the algorithms for such patients mastered during training are similar, and consequently the workup is comparable as well, despite the absence of written recommendations. On the other hand, patients in whom the clinical presentation may be obscured, such as older patients, especially older females (but not female patients in general), and patients with a history of malignancy, were more radiographed in G2. Moreover, more CXR examinations were performed in G2 during off-hours and night shifts compared with G1.This could be related to a lack of expertise and diagnostic uncertainty during the time when additional consultations are not easily available. Other studies reported similar reasons for inappropriate radiologic workup: medico-legal issues,[5]diagnostic uncertainty,[6]inadequate education and training,[7]requests from consulting subspecialty physicians, increased workloads within the ED,[8]and patient self-referral.[9]Contrary to our data, Gardiner and Zhai[10]reported just 0.8%of CXRs performed during off hours as inappropriate in a study from a teaching hospital in Australia.
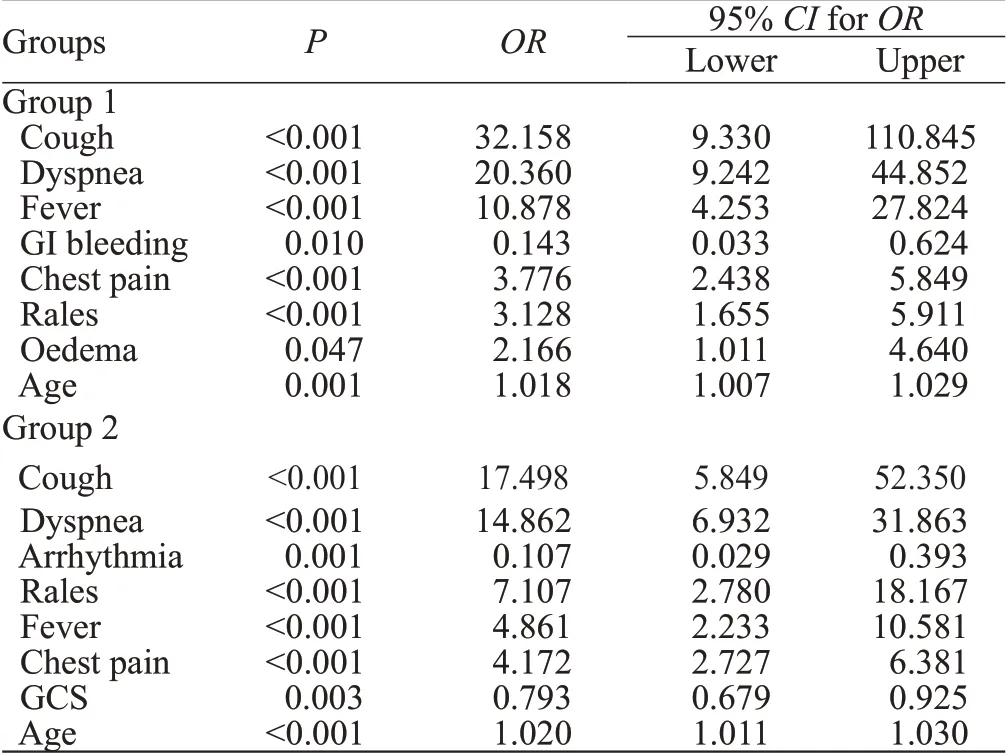
Table 1. Factors independently related to performing chest X-rays
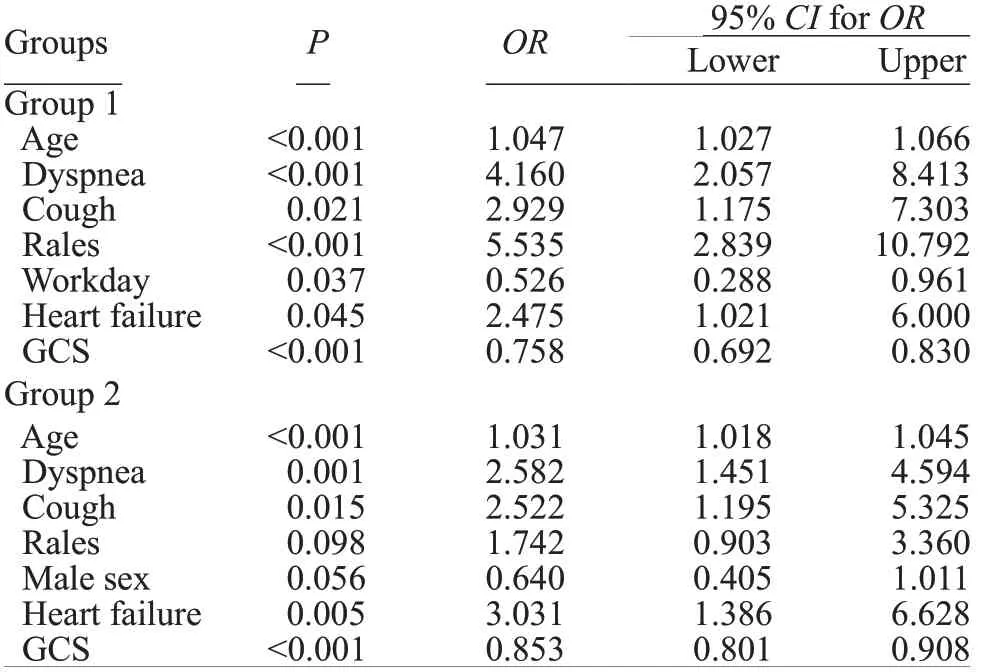
Table 2. Factors independently related to pathologic chest X-ray f indings
The sensitivity to routine CXR could explain the difference recorded for the patients presenting with GI bleeding. Occasionally, gastroenterologists performing urgent endoscopies insist on radiographic investigations,although there is no specific local protocol involving CXR. This may be a possible explanation of the higher CXR rates in patients presenting with GI bleeding.Contrary to IMSs, who have various obligations within their (sub)specialties, EPSs spend their working time exclusively within the ED. This provides them with the possibility to tailor strategies required for particular pathologies. Occasionally, this leads to a generalized approach and unnecessary workup, particularly in instances when the final treatment is performed by other specialists. The American Society for Gastrointestinal Endoscopy suggests that CXR should be considered only in patients with new respiratory signs or symptoms of decompensated heart failure, and routine chest radiography is not recommended before endoscopy.[11]In a meta-analysis of 14,390 preoperative CXRs, unexpected findings were observed in 1.3% of the cases, while only 0.1% of the findings affected the way the patient was treated.[12]Benacerraf et al[13]concluded that in patients under 40 years old with no symptoms CXR should be omitted. Such a guideline could reduce the number of CXRs in this population by 58%. In this study, 24.7% of patients under 40 years underwent CXR. Although the absolute and relative numbers of such patients were low,they could be reduced even further should written protocols be provided.
We observed a non-significant tendency to resolve arrhythmias more promptly in G2 (221 [180-485] minutes vs. 209 [142-372] minutes,P=0.159). This was possibly due to self-governing procedural sedation for electric cardioversion in G2 (acquired during EPS training), as opposed to sedation managed by anesthesiologists in G1.For the same reason (independent treatment, as opposed to examinations performed by other physicians), the workup was less generalized, leading to a higher number of patients in whom CXR could be omitted in G2. Although academic societies provide no clear guideline on CXR in patients presenting with arrhythmia, performing CXR on patients presenting with signs and symptoms of congestion is plausible. Stiell et al[14]presented data on 1,091 patients treated for atrial flutter of fibrillation within the EDs in six Canadian academic hospitals. CXR was performed on all patients. The authors found that radiographic findings of pulmonary congestion, detected in 2.2% of the patients,independently predicted the occurrence of adverse events within 30 days from enrollment.
The majority of EPSs utilize bedside ultrasound,including protocoled examinations such as focused assessment with sonography in trauma (FAST).[15]Such examinations were previously shown to reduce the number of other radiologic examinations, mainly computed tomography.[16]Although this issue was not directly assessed in our study, and the propensity score matching was composed to standardize the tendency to perform CXR, the G2 patients underwent significantly fewer comprehensive abdominal ultrasounds and computed tomographies. This could be appreciated as an advancement of professional ED staffing, and further disputes our hypothesis.
We found IMSs to be more detailed in reporting the radiologic findings in discharge letters. While the significance of this result is hard to assess (possibly being a mere difference in referral style), it is in accordance with the differences in training. While IMSs pay more attention to pathophysiological pathways and tend to explain the diagnostic and treatment decisions more thoroughly, EPSs employ a more “surgical” approach: focused, resolute, and characterized by concise reporting. The same can be stated for differences in the reporting of physical f indings. Although there was no objective way to rate the number of missed auscultation findings, the results suggest that some lung phenomena may have been missed, or at least underreported in G2. Moreover, in regression analysis, the auscultation f inding was the most independent predictor of pathological CXR in G1. Whether this has an impact on the quality of emergency care is not clear.
Similar variables were associated with obtaining CXR in logistic regression in both groups. Although there are no written recommendations, routine CXR for all patients is strongly discouraged. We were unable to find equivalent data regarding non-trauma ED visits for a prediction model comparison in the literature. The rate of CXRs performed in the ED is similar to the ones in other studies. In the National Hospital Ambulatory Medical Care Survey, X-ray imaging was performed in 33.7% out of 49,061 ED visits.[17]In patients assessed for acute cardiac ischemia, Katz et al[18]reported an 85.8% CXR referral rate for EPSs classified as the highest tertile of the malpractice fear score, compared with 73.5% in the lowest tertile. The corresponding percentage for chest pain patients in our study was 56.3%.
In the prediction models for pathological findings,f ive out of seven variables were identical, with the same order when ranked according to level of significance.All variables were easily obtainable by history taking and physical examination. By ROC curve analysis, a significantly better prediction of pathological findings was achieved for G1. A study reported similar rates of pathological f indings,[19]although there were series with considerably lower rates.[20]Al Zadjali et al[20]reported higher rates of normal f indings in young, non-dyspneic,and non-tachypneic patients, as well as in patients with no significant medical history. In patients presenting with chest pain, Hess et al[21]reported an absence of a history of congestive heart failure or smoking, and no abnormalities on lung auscultation as factors required to forgo CXR.
Whether the observed difference in antibiotic prescription rates was the result of a systematically different approach should be assessed in further studies. Huang et al[22]indicated that IMSs and EPSs employed a similar approach to patients with pneumonia. Conversely, Wigton et al[23]reported restrictive antibiotic prescription habits for urinary tract infection in EPSs compared with IMSs.
Study limitations
This was a retrospective observational study. Although a propensity score matching was performed, the results obtained from this study population cannot be unequivocally applied to the general population. The study was conducted during the winter period, possibly leading to a higher percentage of CXRs due to the seasonal peak in respiratory infections. The authors wanted to share their explanation of the significant differences obtained in the analysis,although the majority of them remained within the sphere of speculation.
CONCLUSIONS
To conclude, moving to EPS staffing in the ED does not lead to an increase in radiologic workup. By implementing deliberate usage of ultrasound, some self-governing procedures, case-oriented investigations, and center-specif ic recommendations, unnecessary radiologic workup can be avoided. Professional ED staffing could lead to a higher standard of emergency care.
Funding:This study did not receive any funding.
Ethical approval:Ethical approval for this study was obtained by the Sestre Milosrdnice University Hospital Center Ethics Committee (251-29-11-20-01-8).
Conflicts of interests:The authors declare that they have no competing interests.
Contributors:MP was involved in study concept and design,statistical analysis, drafting, and critical revision of the manuscript.LK conducted data acquisition, and provided statistical expertise and critical revision. IK was involved in study design, data acquisition,analysis and interpretation of the data, language editing, and critical revision. KŽ carried out data acquisition, language editing, and critical revision of the manuscript. VD was involved in study concept and design, study approval and collection of the data, critical analysis of statistical methods, and critical revision of the manuscript.
 World journal of emergency medicine2021年2期
World journal of emergency medicine2021年2期
- World journal of emergency medicine的其它文章
- Effectiveness of an educational program on improving healthcare providers’ knowledge of acute stroke: A randomized block design study
- Role of urine studies in asymptomatic febrile neutropenic patients presenting to the emergency department
- Violence toward emergency physicians: A prospectivedescriptive study
- Poor outcomes of delirium in the intensive care units are amplif ied by increasing age: A retrospective cohort study
- Efficacy and safety of corticosteroids in immunocompetent patients with septic shock
- Blood eosinophils and mortality in patients with acute respiratory distress syndrome: A propensity score matching analysis
