静脉溶栓治疗中急性缺血性卒中TOAST分型特征及预后分析
吴晓强 俞晓翔 谈正叶 金玉华 王琰萍


[摘要] 目的 分析静脉溶栓治疗中急性缺血性卒中TOAST分型特征及其预后。 方法 收集2019年1月至2020年3月我院卒中单元急性缺血性卒中静脉溶栓病例资料,利用NIHSS评分、改良Rankin量表评分(mRS)等量表评估方法,回顾性分析不同TOAST分型溶栓时神经功能缺损、溶栓后出血及病情反复等特征,探讨影响急性缺血性卒中3个月内预后因素。 结果 入组118例患者,不同TOAST亚型间溶栓前、后NIHSS评分比较,差异均有统计学意义(H=12.060,P<0.05;H=11.500,P<0.05);72 h内各亚型溶栓后出血比较,差异有统计学意义(χ2=8.813,P<0.05);各亚型24 h内病情反复比较,差异有统计学意义(χ2=8.123,P<0.05);静脉溶栓3个月后评估,9个因素纳入模型,采用二元Logistic回归分析结果显示,年龄、性别及糖尿病病史不影响3个月内的预后。 结论 急性缺血性卒中静脉溶栓患者TOAST分型的各亚型在溶栓后出血和病情反复上存在差异;多种因素是急性缺血性卒中静脉溶栓3个月内预后的危险因素。
[关键词] 急性脑血管病;静脉溶栓;TOAST分型;预后
[中图分类号] R743.3 [文献标识码] A [文章编号] 1673-9701(2021)34-0004-04
[Abstract] Objective To analyze the TOAST typing features of intravenous thrombolytic therapy on acute ischemic stroke (AIS) and its prognosis. Methods The data of intravenous thrombolysis cases of AIS in stroke unit of our hospital from January 2019 to March 2020 were collected, and the NIHSS score and modified Rankin scale score(mRS) were used to retrospectively analyze the features of nerve function defect, hemorrhage after thrombolysis and relapsed illness during thrombolysis in different TOAST typing, and the factors impacting the prognosis of AIS within 3 months were investigated. Results The NIHSS scores of 118 patients before and after thrombolysis among different TOAST subtypes were statistically significant(H=12.060, P<0.05; H=11.500,P<0.05); There was statistically significant difference in hemorrhage among different subtypes within 72 hours (χ2=8.813,P<0.05). There was significant difference between the subtypes within 24 hours (χ2=8.123,P<0.05). Nine factors were included and evaluated in the model after 3 months of intravenous thrombolysis,and binary logistic regression analysis showed in the result that age,gender and diabetes history did not impact the prognosis within 3 months. Conclusion There are differences in hemorrhage and relapse after thrombolysis among different subtypes of TOAST typing in patients with AIS undergoing intravenous thrombolysis. Many factors are risk factors for prognosis of AIS after intravenous thrombolysis within 3 months.
[Key words] Acute cerebrovascular disease; Intravenous thrombolysis; TOAST typing; Prognosis
随着人口老年化日趋严重,急性缺血性卒中(Acute ischemic stroke,AIS)危害着人类健康。静脉溶栓仍是目前临床一线治疗方法,超早期应用组织型纤溶酶原激活物(Recombinant tissue plasminogen activator,rt-PA)静脉溶栓治疗是有效药物治疗手段之一[1],然而,脑梗死病因的多元化影响脑梗死预后及溶栓效价仍无一致性结论。已有研究显示,大动脉粥样硬化型及心源性脑栓塞型病死率高[2]。本研究回顾性分析我院卒中中心溶栓病例,旨在探讨临床评估短期内卒中患者预后,提供指导临床实践经验,更好地開展溶栓治疗,现报道如下。
1 资料与方法
1.1 一般资料
选取我院卒中中心2019年1月至2020年3月溶栓治疗的急性缺血性卒中患者共146例,排除尿激酶溶栓、血管内治疗、死亡21例,失访7例,入组118例。入院时采集患者的性别、年龄、体重、既往史(高血压病、糖尿病、吸烟史及饮酒史等)。急性脑缺血性卒中诊断均为入院后≤24 h头颅CT或MRI确诊,符合2018年中国急性缺血性脑卒中诊治指南,TOAST亚型是公认的急性缺血性卒中病因学分类标准[3],将急性脑梗死分为大动脉粥样硬化性卒中(Large artery atherosclerotic,LAA)、心源性脑栓死(Cardiogenic embolism,CE)、腔隙性卒中或小动脉闭塞性卒中(Small artery occlusion,SAO)、因其他罕见的原因导致的缺血性卒中(Stroke of other determined etiologies,SOE)、不明原因的缺血性卒中(Stroke of under demonstrated etiology,SUE)。上述病例均通过MRI、颈部血管及心脏超声、MRA或CTA、血液检测等检查,由2名主治及以上医师讨论后明确诊断。
1.2 方法
溶栓流程获医院医学伦理委员会批准,患者或近亲属签署知情同意书,采用注射用阿替普酶(商品名:爱通立,国药准字JS20160047)静脉溶栓,按照0.9 mg/kg,最大量不超过90 mg,先1 min内静脉注射10%总量,剩余加入生理盐水100 mL微泵注射,60 min结束,溶栓后24 h后予以抗血小板聚集、调脂稳定斑块、神经保护、改善循环等治疗。溶栓前后、出院前予NIHSS评分量表评分(The national institutes of health stroke scale,NIHSS);溶栓前后、出院前及3个月后予改良Rankin评分量表(Modified rankin scale,mRS)评分。神经功能缺损程度:NIHSS评分≤6分为轻度,7分≤NIHSS<15分为中度,NIHSS≥15分为重度。预后良好:mRS≤2分,预后不良mRS>2分。评分者经专业培训且具有主治医师资历。溶栓后出血标准:包括梗死病灶内和病灶外,溶栓治疗后72 h内或临床症状恶化时立即行头颅CT检查,根据有无症状可分为症状性和非症状性。症状性颅内出血常用的评价标准为美国国立卫生院卒中研究(National Institute of Neurological Disease and Stroke,NINDS)标准:溶栓后头颅影像学复查提示出血,且伴有神经症状及体征加重;0~24 h内神经缺损症状溶栓好转后病情反复:根据欧洲急性卒中协助研究(European Cooperative Acute Stroke Study,ECASS),NIHSS评分较溶栓后基线水平增加4分及以上。
1.3 统计学方法
采用SPSS 22.0统计学软件进行数据处理,对样本进行正态检验,同时检测方差齐性检验。无序分类变量用构成比表示,采用χ2检验;有序分类变量采用秩和检验;对可能影响预后的因素采用二元Logistic回归分析。P<0.05为差异有统计学意义。
2 结果
2.1 不同TOAST分型神经功能缺损程度溶栓前、后比较
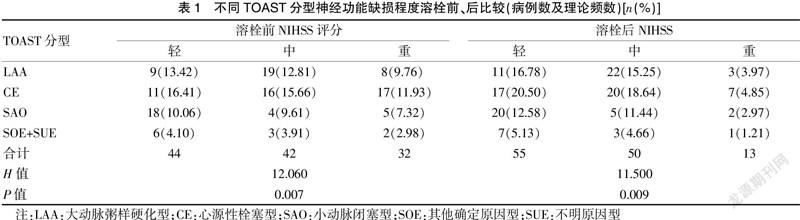
溶栓前LAA、CE、SAO及SOE+SUE四组间NIHSS分值比较,差异有统计学意义(H=12.060,P<0.05),LAA和CE神经功能缺损为重,SAO和SOE+SUE相对较轻;溶栓后四组之间比较,差异有统计学意义(H=11.500,P<0.05)。见表1。
2.2 不同TOAST分型在溶栓72 h内出血转化
LAA、CE、SAO及SOE+SUE四组间在0~72 h内出血转化的比较,差异有统计学意义(χ2=8.813,P<0.05)。见表2。
2.3 24 h内不同TOAST分型溶栓病情再反复的比较
LAA、CE、SAO及SOE+SUE四组间病情反复比较,差异有统计学意义(χ2=8.123,P<0.05)。见表3。
2.4 预后评估
纳入可能影响不同TOAST分型脑梗溶栓9个因素,预后评估为二元因变量(预后良好:mRS≤2分,预后不良:mRS>2分),故采用二元Logistic回归分析,为了减少类别间比较误差,TOAST分型按无序多分类变量处理结果显示,年龄、性别及糖尿病病史不影响3个月内的预后。见表4。
3 讨论
AIS超早期静脉rt-PA溶栓治疗疗效已达成了共识[4],但不同TOAST分型患者溶栓后的临床结局却差异很大[5]。Dong等[6]在一组AIS患者rt-PA溶栓的治疗研究中发现,所有卒中亚型中基线NIHSS评分与良好的预后相关。本研究回顾性分析我院卒中中心不同TOAST分型患者rt-PA溶栓前的NIHSS评分,溶栓前LAA和CE的NIHSS评分较SAO及SOE+SUE高,溶栓前、后CE患者神经功能缺损程度严重,可见不同TOAST分型溶栓前、后NIHSS评分及即刻效果可能与病变性质和血栓性质有关,从不同TOAST病因分析出发,SAO主要由穿支动脉的玻璃样变和纤维素样坏死所致,病灶小、分散且不规律,神经功能缺损程度轻[7],临床实践可见部分SAO患者无意中被发现,CE多见于心源性栓子脱落急性闭塞动脉,代偿难以建立,神经功能缺损严重,且静脉溶栓效果不佳[8],而LAA累及大血管,斑块纤维帽破坏,一段时间内发生一定血流动力学改变,易出现进展性卒中或远端栓塞,24 h内溶栓后病情反复。
rt-PA静脉溶栓中经常会关注溶栓后出血包括症状性和非症状性,以及病程演变进展问题。有研究表明,阿替普酶溶栓后出血主要与阿替普酶相关的凝血功能障碍、再灌注损伤和血脑屏障破坏等相互作用有关[9-11]。本研究结果显示,CE患者72 h内溶栓后出血率明显较其他型高,与相关研究[12]一致,但与NINDS试验并不完全一致[13],回顾样本中CE几乎均合并房颤病史,研究已证实心房颤动病史是阿替普酶静脉溶栓后发生出血性转化的独立影响因素[14-15],房颤产生的血栓脱落快速栓塞血管,造成急性缺血缺氧,血脑屏障破环严重,加之rt-PA溶解血栓,血管再通后再灌注损伤。AIS早期症状波动或进展是长期预后的预测因素,20%~40%的AIS患者在急性期内发生症状波动,60%症状加重者不能恢复到发病前基线状态[16],与狭窄动脉或微栓子、缺少侧支循环、低灌注等有关[17-18]。由表3可知,LAA患者较其他组易发生病情反复,不同TOAST分型患者在溶栓前神经缺损程度、溶栓后出血及病情反復等病程特点存在差异。
除溶栓时间窗外,与AIS预后相关的因素还很多,如血压、年龄、体重、性别、溶栓前神经缺损程度、溶栓前的影像学改变等,各研究有不同的结论[14]。本研究仅调查了3个月内AIS预后,以预后良好(mRS≤2分)和预后不良(mRS>2分)的对立性因变量建立二元Logistic回归模型,纳入年龄、性别、高血压病病史、糖尿病病史、饮酒史、吸烟史、溶栓后出血转化、病情反复等为模型自变量,TOAST分型按无序多分类变量处理,结果显示年龄和性别对3个月的预后无明显影响,这可能与入组患者偏老年化有关。有趣的是,影响不同TOAST分型的卒中预后,未发现糖尿病病史影响AIS溶栓后3个月内预后,可能原因在于与积极医疗干预和严格血糖管理有关;糖尿病是全身代谢紊乱的慢性疾病,或仅影响卒中再发,近期严格控制血糖水平,会减少卒中再发风险。有研究发现,有糖尿病史AIS患者接受静脉溶栓治疗后,与没有这些病史的患者相比,具有相似的临床结局,且其出血风险未增加[19]。亦有研究提示糖尿病史与溶栓后不良结局无关,且与未溶栓患者相比,具有糖尿病史的卒中患者仍能从溶栓治疗中获益[20],故对该类患者仍应积极溶栓治疗,使患者的临床获益最大化。
[参考文献]
[1] Rabinstein AA. Treatment of acute ischemic stroke[J]. Continuum(Minneap Minn),2017,23(1,Cerebrovascular Disease):62-81.
[2] Liu CH,Lin JR,Liou CW,et al. Causes of death in different subtypes of ischemic and hemorrhagic stroke[J]. Angiology,2018,69(7):582-590.
[3] Geisler T,Mengel A,Ziemann U,et al. Management of embolic stroke of undetermined source(ESUS)[J]. Drugs,2018,78(8):823-831.
[4] Akinseye OA,Shahreyar M,Heckle MR,et al. Simultaneous acute cardio-cerebral infarction:Is there a consensus for management?[J]. Ann Transl Med,2018,6(1):7.
[5] 張艳丽.不同TOAST亚型的青年脑梗死患者预后的差别及影响因素[J]. 中国实用神经疾病杂志,2016,19(16):20-22.
[6] Dong Y,Cao W,Cheng X,et al. Risk factors and stroke characteristic in patients with postoperative strokes[J]. J Stroke Cerebrovasc Dis,2017,26(7):1635-1640.
[7] Qiao Q,Hong Y,Zhao W,et al. Sex differences in outcomes and associated factors among stroke patients with small artery occlusion in China[J]. Biol Sex Differ,2018, 9(1):35.
[8] Capodanno D,Mehran R,Valgimigli M,et al. Aspirin-free strategies in cardiovascular disease and cardioembolic stroke prevention[J]. Nat Rev Cardiol,2018,15(8):480-496.
[9] Yaghi S,Willey JZ,Cucchiara B,et al. Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke:A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association[J]. Stroke,2017, 48(12):e343-e361.
[10] Li Y,Zhong W,Jiang Z,et al. New progress in the approaches for blood-brain barrier protection in acute ischemic stroke[J]. Brain Res Bull,2019,144:46-57.
[11] Zhong C,Yang J,Xu T,et al. Serum matrix metalloproteinase-9 levels and prognosis of acute ischemic stroke[J]. Neurology,2017,89(8):805-812.
[12] Saposnik G, Strbian D. Enlightenment and challenges offered by DAWN trial(DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention with Trevo)[J]. Stroke,2018,49(2):498-500.
[13] Porter RJ,Kupferberg HJ. The anticonvulsant screening program of the National Institute of Neurological Disorders and Stroke,NIH:History and Contributions to Clinical Care in the Twentieth Century and Beyond[J]. Neurochem Res,2017,42(7):1889-1893.
[14] Mehrpour M,Afrakhte M,Shojaei SF,et al. Factors predicting the outcome of intravenous thrombolysis in stroke patients before rt-PA administration[J]. Caspian J Intern Med,2019,10(4):424-430.
[15] Vaclavik D,Vilionskis A,Jatuzis D,et al. Clinical outcome of cardioembolic stroke treated by intravenous thrombolysis[J]. Acta Neurol Scand,2018,137(3):347-355.
[16] Geng HH,Wang Q,Li B,et al. Early neurological deterioration during the acute phase as a predictor of long-term outcome after first-ever ischemic stroke[J]. Medicine (Baltimore),2017,96(51):e9068.
[17] Chen Z,Li W,Sun W,et al. Correlation study between small vessel disease and early neurological deterioration in patients with mild/moderate acute ischemic stroke[J]. Int J Neurosci,2017,127(7):579-585.
[18] Shi Z,Zheng WC,Fu XL,et al. Hypercoagulation on thromboelastography predicts early neurological deterioration in patients with acute ischemic stroke[J]. Cerebrovasc Dis,2018,46(3-4):125-131.
[19] Gadalean F,Simu M,Parv F,et al. The impact of acute kidney injury on in-hospital mortality in acute ischemic stroke patients undergoing intravenous thrombolysis[J]. PLoS One,2017,12(10):e0185 589.
[20] Tsivgoulis G,Katsanos AH,Mavridis D,et al. Association of baseline hyperglycemia with outcomes of patients with and without diabetes with acute ischemic stroke treated with intravenous thrombolysis:A propensity score-matched analysis from the SITS-ISTR registry[J]. Diabetes,2019, 68(9):1861-1869.
(收稿日期:2020-12-19)

