Clinical Effects of the Qi-acupuncture Therapy of TCM on Portal Hypertension
XU Yu-bo (许钰波), LIU Xiang (刘 湘)
1. Department of TCM Prevention and Healthcare, National Key Clinical Hepatology Hospital, Hebei Hepatopathy Hospital of TCM, Shijiazhuang 050800, China
2. The Outpatient Department of Hebei Hospital of TCM, Shijiazhuang 050000, China
ABSTRACT Objective:To explore the effective prevention and treatment of portal hypertension (PH).Methods : A total of 220 patients who came to our hospital from March 2015 to October 2018 were treated.They were randomly divided into the treatment group and the control group, each with 110 cases. Before treatment, there was no significant differences in age, sex, clinical symptoms, signs, laboratory tests and color Doppler ultrasound related examinations between the 2 groups (P>0.05). Among them, the treatment group on the basis of traditional Chinese and Western medicine treatment in our hospital, the Qi-acupuncture therapy of TCM was added. The extra meridian acupoints along with acupoints were selected. The control group received conventional treatment with traditional Chinese and Western medicine in our hospital. Results: There were significant differences in clinical symptoms, signs and chemistry between groups after treatment (P<0.01).There were significant differences in test, color ultrasound related examination and so on (P<0.01). Those in the treatment group was significantly better than the control group (P<0.01). Conclusion: On the basis of the Qi-acupuncture therapy of TCM, selecting extra meridian acupoint and acupoints can effectively treat PH.
KEYWORDS Portal hypertension; Cirrhosis; Qi-acupuncture therapy of TCM; Acupuncture
BACKGROUND
Portal hypertension is an important factor affecting the clinical prognosis of patients with liver cirrhosis. It is severity determines the occurrence and development of complications of cirrhosis,such as esophagogastric variceal bleeding,peritoneal effusion, hepatorenal syndrome, hepatic encephalopathy, hepatic myelopathy, etc.[1]. In 2015, hepatitis B resulted in 887 000 deaths,mostly from complications (including cirrhosis and hepatocellular carcinoma)[2]. Esophageal and gastric variceal bleeding is the most common complication of PH in cirrhosis, and the incidence is as high as 55.6%. The Department of Preventive and Health Care of TCM in our hospital randomly selected 220 patients on the basis of acupuncture treatment of hepatic PH, who were treated in groups. The curative effect was good. The report was as follows.
CLINICAL DATA
General Information
From March 2015 to October 2018, 220 patients with PH were hospitalized in our hospital. They were randomly divided into the treatment group and control group for clinical research. In the treatment group,110 cases were treated, including 66 males and 44 females, aged 20-70 years old, including 2 cases of pre-hepatic type, 103 cases of hepatic type and 5 cases of post-hepatic type, 96 cases of ascites, 14 cases of pleural effusion, 35 cases of edema of lower limbs, 20 cases of abdominal wall varices and 14 cases of varices of lower limbs. There were 110 cases in the control group, including 66 males and 44 females,aged 22-70 years old, including 2 cases of pre-hepatic type, 103 cases of hepatic type and 5 cases of posthepatic type, 96 cases of ascites, 14 cases of pleural effusion, 34 cases of edema of lower extremities, 20 cases of varicose veins of abdominal wall and 14 cases of varicose veins of lower extremities. There were no significant differences in age, sex, clinical symptoms,signs, laboratory tests and color Doppler ultrasound related examinations between the 2 groups (P>0.05).
Diagnostic Criteria
The diagnosis and treatment guide of cirrhosis[3],the diagnosis and treatment guide of liver fibrosis[4],the consensus of diagnosis and treatment of cirrhosis[5], China Experts' Consensus on the Clinical Application of the Gradient of Hepatic Venous Pressure (2018)[6], prevention and treatment of esophagogastric varices bleeding in cirrhotic PH[7]were applied. Hilscher moira-b, etc.[4]believed that the elastic imaging of the spleen is helpful to monitor the occurrence of PH before and after shunt operation.
Exclusion Criteria
Patients with primary liver cancer or acute esophageal and gastric variceal bleeding, except for patients younger than 14 years or older than 70 years.
Inclusion Criteria
Both the "diagnostic criteria" and the "exclusion criteria" were met.
Basic Information of the Drugs Used
Selection of acupuncture needles: Huatuo brand acupuncture needles, Production License No.:Jiangsu Food and Drug Medical Device Production License 20010020, Registration License No.: Jiangsu Medical Device Registration License 20162270970,Product Technical Requirements No.: Jiangsu Medical Device Registration License 20162270970.
Propranolol hydrochloride tablets, Jiangsu Yabang Epperson Pharmaceutical Co., Ltd,Approval No.: H32020133, executive standard:Chinese Pharmacopoeia 2010 Second Edition,Packaging: plastic bottles, 100 tablets per bottle.
Methods and Therapeutic Schedule
With inclusion criteria and exclusion criteria,220 hospitalized patients with PH were given our routine medicine treatment. Treatment of ideas for all patients were fasting spicy greasy food during compensatory period in order to protect the liver cells and improve liver function, along with prevention and treatment of complications. Chinese medicine for activating blood circulation and strengthening body immunity were used to promote the liver cell regeneration. For decompensated period, patients should take rest and control diet. Food rich in protein and vitamin and digestible is given with priority.When liver function is damaged significantly or have precursors of hepatic encephalopathy, intake of protein is restricted or prohibited. With low sodium salt or autumn stone diet, hard coarse food is avoided. Treatment of western medicine diuretics,amino acid supplement human blood albumin is supported. At the same time, combined with blood circulation by removing blood stasis, tonifying spleen and kidney Qi was applied. According to random number table, the patients were divided into the treatment group and control group. There was no significant difference before treatment (P>0.05).Among them, 110 patients in the treatment group received acupuncture at the external points with Qi-acupuncture therapy of TCM [Leitou (肋头),Pigen (痞根), Xinglong (兴隆), Xinleitou (新肋头),Mingguan (命关), Piheng (脾横) etc.[8]], cooperateed with acupuncture points [Zusanli (足三里), Pishu (脾俞), Neiguan (内关), Sanjiaoshu (三焦俞), Ganshu (肝俞), Shangjuxu (上巨虚), Xingjian (行间), Taichong(太冲) etc.], once a day, 10 times a month intermittent treatment, every 10 times for a course of treatment,a total of 8 courses at the end of the treatment. In the control group, 110 patients were given propranolol tablets, 10 mg each time, three times a day, for 8 months until the end of observation. The liver function, blood routine, hepatic fibrillation, four-protein ratio, liver, gallbladder, spleen, abdomen and color doppler ultrasound were observed at 1 month, 4 months and 8 months after the start of the treatment.
Methods of Efficacy Evaluation
The guideline for diagnosis and treatment of liver cirrhosis and the consensus treatment standard of integrated traditional Chinese (2019) and Western medicine (2011) for liver cirrhosis were used as the criteria of efficacy evaluation.
Statistical Methods
All the data were analyzed by SPSS22.0 statistical software, and the data of each group were expressed by mean standard deviation(s). Thetvalues of samples were tested before and after treatment,and the calculated data were tested by χ2test.
RESULTS
There were significant differences in clinical symptoms, signs and chemistry between two groups after treatment (P<0.01). There were significant differences in test, color ultrasound related examination and so on (P<0.01). Those in the treatment group were significantly better than the control group (P<0.01).
There were no significant differences in the clinical typing cases number and proportion of the 2 groups before treatment (P>0.05), and there were significant differences after treatment (P<0.01). After 8 months of treatment, there were 0 case of prehepatic type accounted, 3 cases of hepatic type and 1 case of post-hepatic type accounted in the treatment group; there were 1 case of pre-hepatic type accounted, 50 cases of hepatic type and 5 cases of post-hepatic type accounted in the control group.Thus, that in treatment group was significantly better than the control group (P<0.01) (Table 1).
There was no significant difference in ascites,pleural effusion, edema of lower limbs, abdominal wall varices and varicose veins of lower limbs between the 2 groups before treatment (P>0.05).There were significant differences in the 1 month,the 4 months and the 8 months after treatment(P<0.01), and the longer the course of treatment, the greater the difference. After 8 months, other signs were completely eliminated in the treatment group except for 4 cases (3 cases of hepatic type and 1 case of retrosinus hepatica). In the control group,2 cases of pleural effusion, ascites and bilateral lower extremity edema disappeared completely.44 cases of ascites disappeared, and 2 cases of pleural effusion disappeared. There were 52 cases of ascites, 12 cases of pleural effusion, 30 cases of lower extremity edema, 20 cases of abdominal varicose veins, and 14 cases of lower extremity varicose veins (Table 2).
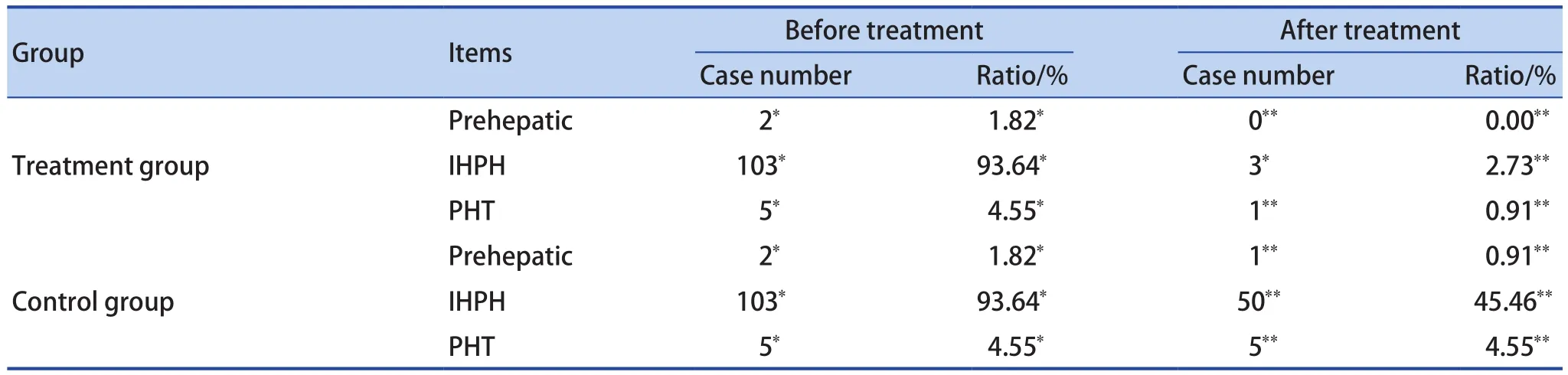
Table 1. Clinical Typing Proportion and Changes Before and After Treatment of Patients in the 2 Groups (n=110)
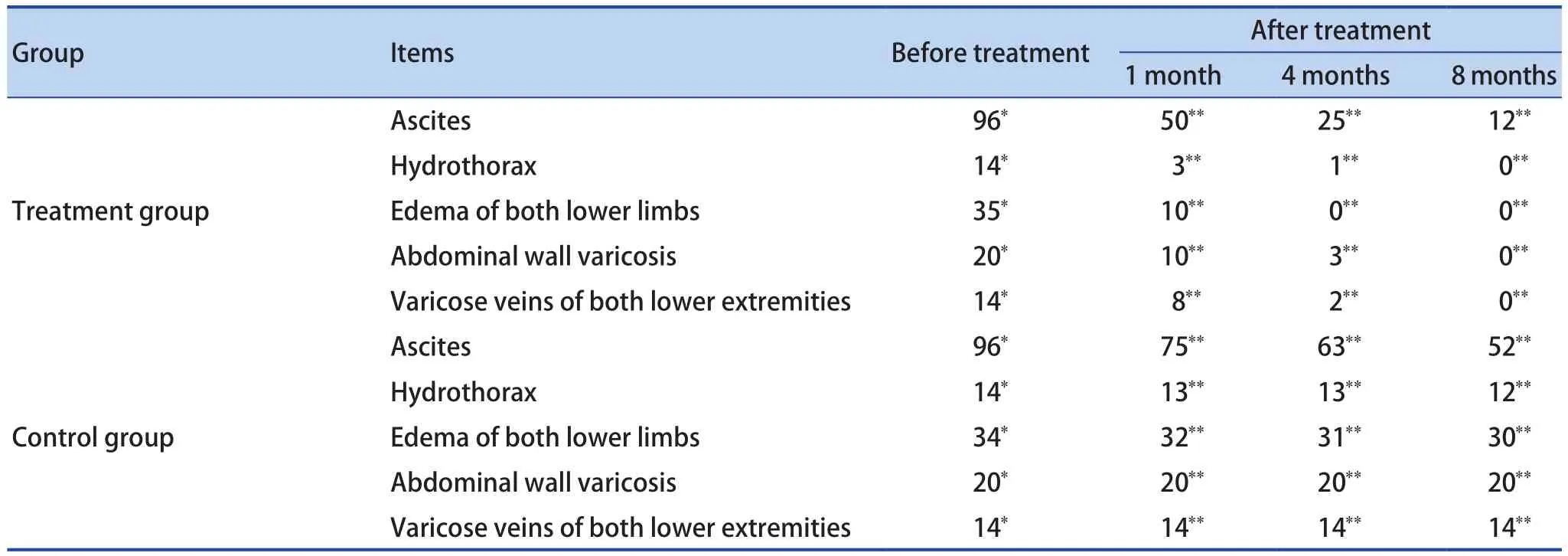
Table 2. Changes of Clinical Signs of Patients Before and After Treatment in the 2 Groups (n=110)

Table 3. Color Ultrasound Data of the 2 Groups of Patients Before and After Treatment (n=110)
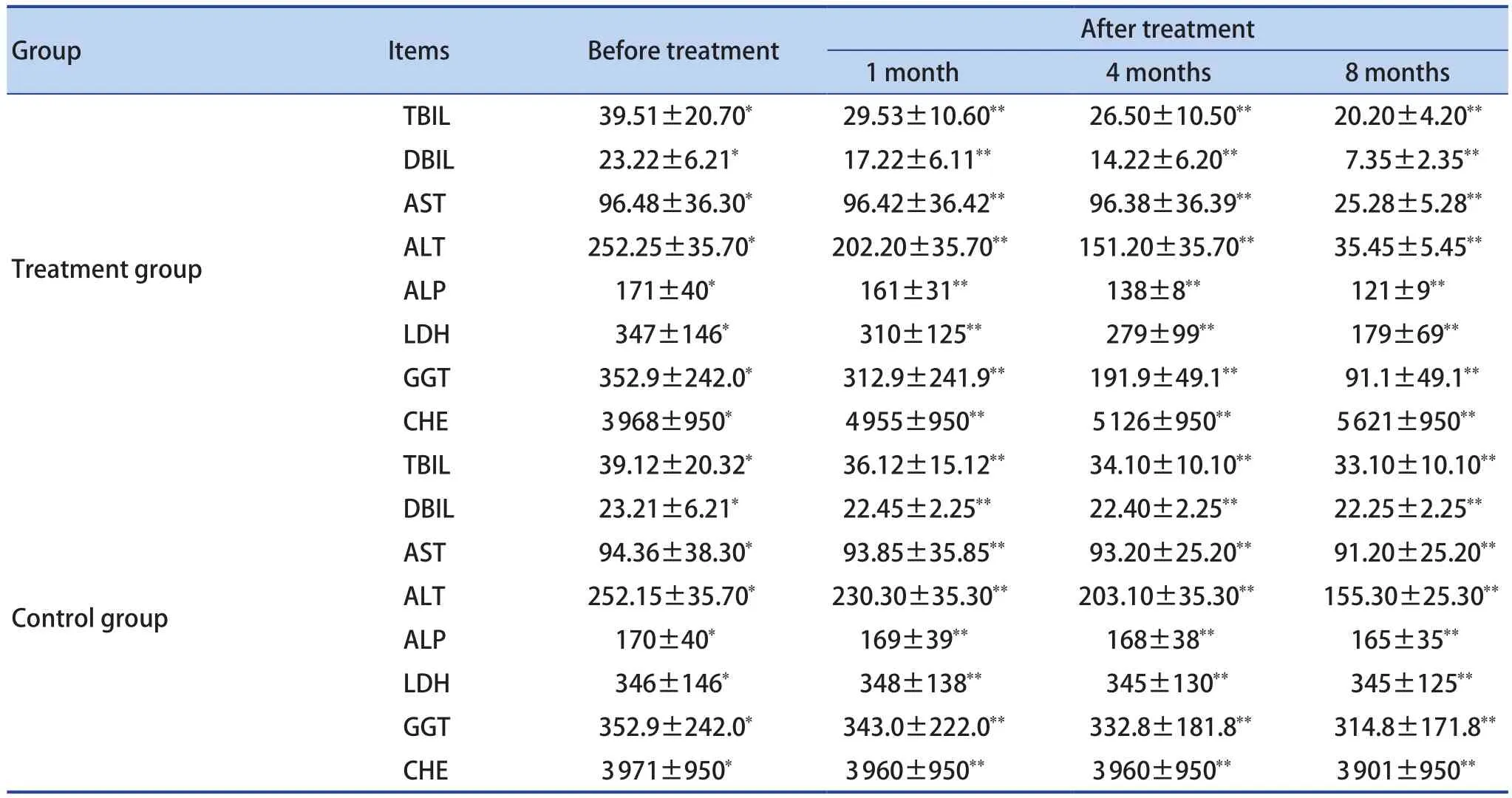
Table 4. Changes of Liver Function in Patients Before and After Treatment in the 2 Groups (n=110)
Before treatment, there was no significant difference in color doppler ultrasound data between the 2 groups (P>0.05). After treatment,there were significant differences in 1 month, 4 months and 8 months (P<0.01), and the longer of the treatment course, the greater of the difference(Table 3).
There were no significant differences in liver function and the ratio of albumin, globulin and protein and the four indexes of liver fibers between the 2 groups before treatment (P>0.05). There were significant differences in liver function between the 2 groups after 1 month, 4 months and 8 months(P<0.01), and the longer the course of treatment, the greater the difference (Table 4-6).
There were no significant differences in blood routine between the 2 groups before treatment(P>0.05), but there were significant differences in 1 month, 4 months and 8 months after treatment(P<0.01), and the longer the course of treatment, the greater the difference (Table 7).
DISCUSSIONS
PH refers to a series of clinical manifestations caused by elevated pressure of the portal vein system. Ayad Ahmad Mohammed[9]has clinical findings that caput medusae sign is a clinical sign indicating PH. It results from shifting of blood flow from the portal venous system to the systemic circulation. It is a comprehensive clinical manifestation of portal vein circulation disordercaused by various reasons, rather than a single disease. All of them can cause portal vein blood flow disorder and/or increase of blood flow, and can cause portal hypertension. In our clinical statistics, 4 cases of pre-hepatic type accounted for 1.82%, 206 cases of liver type accounted for 93.64%, and 10 cases of post-hepatic type accounted for 4.55%. This shows that hepatitis cirrhosis is the main cause of PH. PH manifests as splenomegaly, esophagogastric varices and ascites,which is often accompanied by hypersplenism,upper gastrointestinal hemorrhage, portosystemic shunt encephalopathy and spontaneous bacterial peritonitis, and the symptoms of the primary disease vary with the disease. Other manifestations were spider nevus, palmar of liver and hypofunction of liver, especially the establishment and opening of collateral circulation, which are characteristic for the
diagnosis of PH. The fluctuation range of portal vein pressure in normal people is large, ranging from 0.981 to 1.47 kPa, but it can still be normal within 1.862 kPa. PH can be diagnosed when the pressure of portal vein exceeds 2.45 kPa or 1.47 kPa above the pressure of inferior vena cava. When the pressure of splenic marrow exceeds 2.27 kPa or the wedge pressure of hepatic vein (WHVP) is higher than that of inferior vena cava 0.533 kPa, PH can also be diagnosed. Hepatic portal vein pressure gradient (HVPG) is currently recognized as the gold standard for measuring portal vein pressure.CSPH is defined as HVPG (>10 mm Hg). HVPG is traumatic and difficult to carry out routinely and apply many times. The direct measurement of portal vein pressure is traumatic and risky, and is disturbed by the change of intra-abdominal pressure. It is difficult to popularize it in clinical practice[10]. YI FF and other researchers[11]believed that spontaneous splenorenal shunt can effectively reduce the pressure of portal vein, but also reduce the blood flow into the liver.
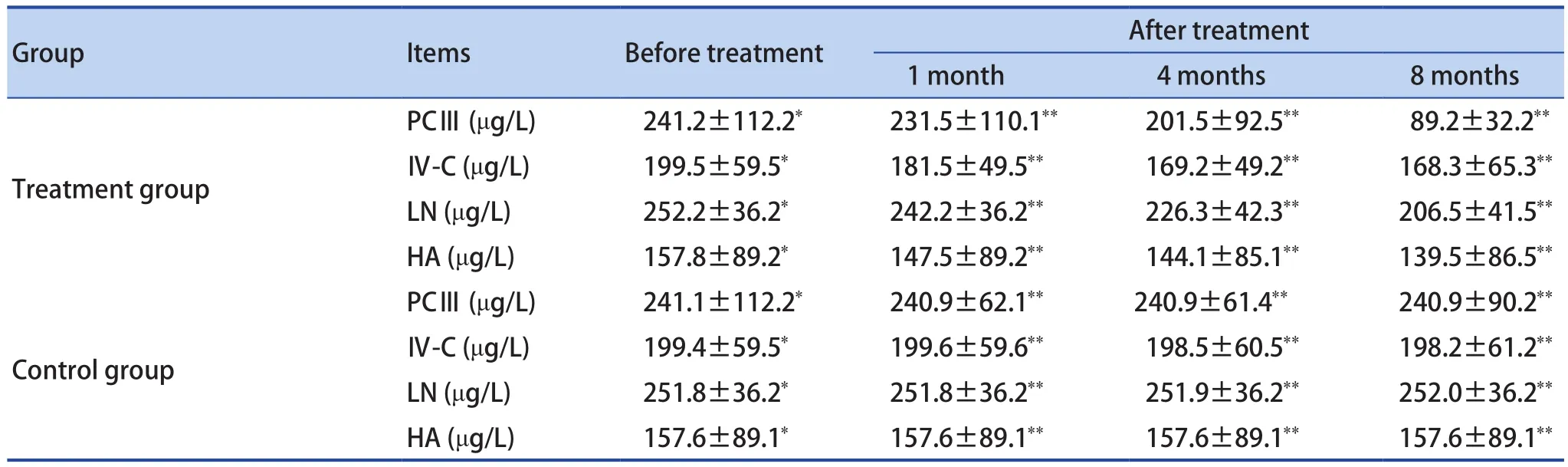
Table 5. Changes of Liver Fibers in the 2 Groups Before and After Treatment (n=110)
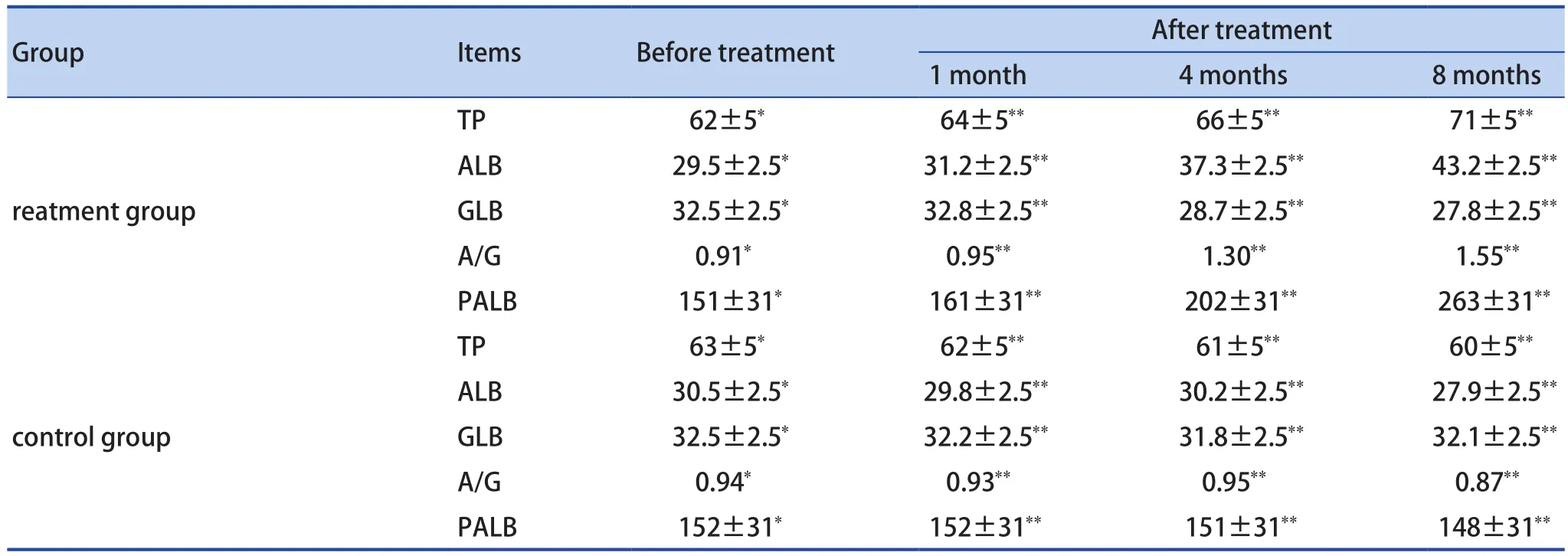
Table 6. Changes of Protein Ratio Before and After Treatment in the 2 Groups (n=110, %)
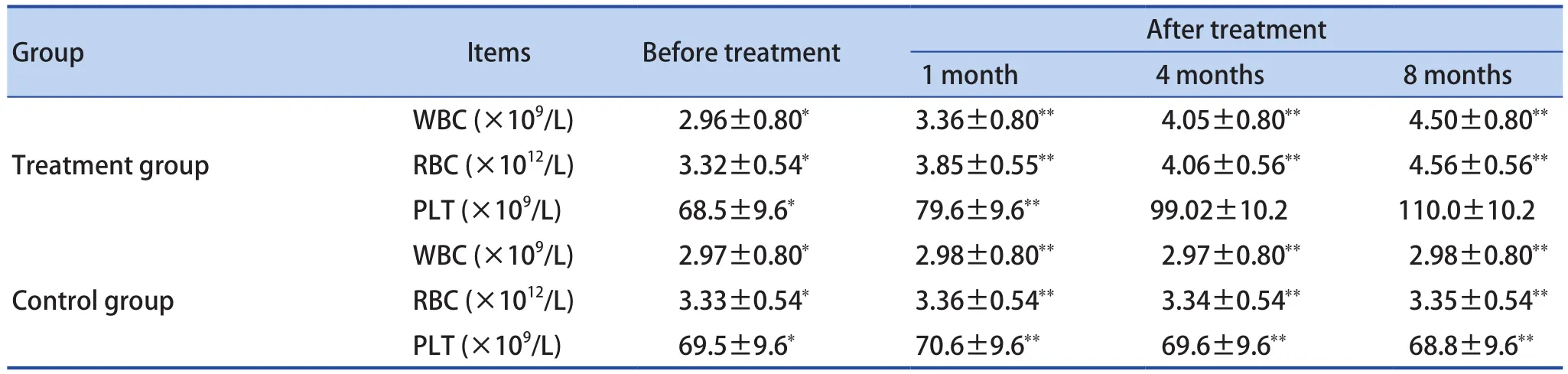
Table 7. Changes of Blood Routine Before and After Treatment in the 2 Groups (n=110)
The concept of PH is a modern medical pathology. TCM do not have the same name,but they have a large number of clinical cases.Relevant records can be classified into the categories of "accumulation", "bloating", "jaundice","hemorrhage", "Qingjin (Blue veins)", "Caput medusae sign" and "abdominal blue veins(abdominal varices)" in TCM.
In 1980, Benoit used propranolol to treat PH, which has been recognized as an effective treatment for PH. Spironolactone tablets and non-peptidyl vasopressin are often used in the treatment of refractory ascites in cirrhosis with PH.Non-peptide vasopressin Vaptans mainly include tovaptan and sartoptan. However, the drawbacks of its treatment are becoming more and more obvious.It is necessary to maintain blood pressure drop by about 1/4 with lifelong medication. Most patients underwent splenectomy with splenic vein shunt or TPIS because of massive upper gastrointestinal hemorrhage. The biggest drawback is that the immunity of patients is seriously reduced and hepatic encephalopathy may occur at any time[12]. Carmelo Cicciò etc.[13]thinks that interventional radiology may offer an effective treatment option in case of variceal bleeding in advanced liver disease with PH resistant to conventional therapies. Lotto Topit[14]and other follow-up statistics revealed that PH in children is a heterogeneous disease. It needs multi-channel treatment, and continues to follow up. Although bleeding events recurred in adulthood, the health status of long-term survivors reported by patients was encouraging. Garcia Tsao Guadalupe[15]and other randomized controlled trials found that the treatment of non-alcoholic steatohepatitis-related cirrhosis with severe PH with imricasson could not prove the benefit of patients. Emricasan treatment appeared safe and well-tolerated. Cirrhosis (scarring of the liver) is the main consequence of nonalcoholic steatohepatitis (NASH). Cirrhosis leads to high pressure in the portal vein which accounts for most of the complications of cirrhosis. Reducing portal pressure is beneficial in patients with cirrhosis.Troisi, Roberto Ivan, FEBS and other study[16]established the efficacy of somatostatin as a liver inflow modulator. GU Y, et al.[17]believed that shortterm use of statins to improve portal vein pressure parameters, follow-up found that long-term treatment is conducive to the prognosis of cirrhosis.
This topic highlights the application of the theory of "TCM preventive treatment of disease"and "seeking the basis for treating the disease"in the clinical practice of liver diseases. Director XU YB[18]of our hospital used Qi-acupuncture therapy to solve the cirrhosis of PH, which is a scientific research subject of Hebei TCM program research on the clinical effect of acupuncture on cirrhosis of portal hypertension. In January 2018,he has obtained the scientific and technological achievements of Hebei Province, and won the second prize of science and technology progress award of Hebei Academy of TCM in the same year.On this basis, the application and expansion of the treatment scope (except for liver cancer) has achieved good results.
It is the first time to put forward the basic theory of TCM clinical practice that blood is often more than enough and Qi is insufficient. Here "Blood"refers to congestion or blood stasis and scurvy, and"Qi" refers to genuine Qi (真气) and Healthy Qi (正气). It is different from the "Qi and blood" in the "Qi and Blood Deficiency and Excessiveness" in our syndrome differentiation and treatment. WHO[19]believed TCM is based on theories about Qi, a vital energy, which is said to flow along channels called meridians and help the body to maintain health.In acupuncture, needles puncture the skin to tap into any of the hundreds of points on the meridians where the flow of Qi can be redirected to restore health. Treatments, whether acupuncture or herbal remedies, are also said to work by rebalancing forces known as Yin and Yang. We recognize that the essence of PH in cirrhosis is the pathological changes of blood caused by insufficient Qi, that is,the problem of Qi leads to the pathological changes of blood and collaterals, so solving the problem of Qi can solve the pathological changes of blood.
Among of the prescription, Leitou point (肋头穴) is an extra point through external channels,which has the effect of relieving cough, relieving asthma, resolving phlegm and dispersing knots.InQian Jin Yi Fang(<<千金翼方>>)[20]: "To treat abdominal mass, moxibustion the same side acupoint on the affected area". Moxibustion of Leitou point is mainly used to treat abdominal mass,fullness in the chest, inability to eat and drink,hepatosplenomegaly, cirrhosis, etc. The Pigen acupoint (痞根穴) can strengthen the spleen and stomach, regulate Qi and relieve pain, mainly treat lump (hepatosplenomegaly) not healing for a long time[21]. The Xinglong point (兴隆穴) and Xinleitou point (新肋头穴) mainly treats hepatosplenomegaly,intercostal neuralgia, pleurisy, bronchitis, hiccup,etc. The Shidou point (食窦穴) is mainly used for all spleen diseases, postpartum abdominal distention and edema. The Piheng point (脾横穴) is mainly used for all spleen diseases. The meridian points Zusanli(足三里) are the key for liver disease treatment of stomach meridian of Foot-Yangming (足阳明胃经). It can change spleen dampness, generate stomach Qi,regulate body immunity, enhance disease resistance,regulate spleen and stomach, replenish middle Qi,activate meridians and collaterals, dredge weathering dampness, and strengthen healthy and eliminate pathogenic factors. It is found that acupuncture at Zusanli[22]is the necessary acupoint for the treatment of portal hypertension in liver cirrhosis. WANG W[23]and other animal experimental findings whether alone or in combination with TCM, electroacupuncture or acupoint injection can improve the blood flow of portal hypertension, reduce the four indexes of liver fibrosis(HA, PⅢ, LN, Ⅳ-C in serum), improve the function of stomach and intestine, eliminate ascites, etc. YANG YP et al.[24]found that electroacupuncture at Zusanli and Shangjuxu (上巨虚) plays an important role in promoting the recovery of gastrointestinal function and alleviating the discomfort caused by operation. The Pishu (脾俞) are the acupoints of the Foot-Taiyang meridian (足太阳经), which is good at evacuating the dampness and heat of the spleen. Neiguan (内关) belongs to pericardium meridian hand-Jueyin(手厥阴经), one of the eight meridians intersecting points, which can pass Yinwei meridian (阴维脉), and is beneficial to the heart and mind, stomach, chest and qi, calming and pain relief. Sanjiaoshu (三交俞)belongs to the stomach meridian of Foot-Yangming,which has the function of regulating large intestine Qi. The heat of external dispersion goes up along the bladder meridian, and the cold descending liquid goes down the bladder meridian. Ganshu acupoints(肝俞穴) in Foot-Taiyang bladder meridian (足太阳膀胱经) can distribute the heat of liver effectively. The heat of external dispersion goes up along the bladder meridian, and the cold descending liquid goes down along the bladder meridian. Shangjuxu (上巨虚)belongs to the Stomach Meridian of Foot-Yangming(足阳明胃经), and the large intestine meridians are combined at the lower points, which has the function of regulating the large intestine Qi mechanism. It is suitable for regulating the stomach and intestines,dredging channels and activating collaterals. It has the functions of dredging the intestines and transforming stagnation, regulating the spleen and stomach, and dispersing channels and regulating Qi.It belongs to points of liver meridian of foot-Jueyin (足厥阴经), which can clear the liver and reduce heat,cool the blood and calm the nerves, and quench the wind and activate collaterals. It has the functions of soothing the liver and relieving the heat, relieving the chest and threatening. Taichong (太冲) belongs to the liver meridian of foot-Jueyin (足厥阴肝经), points of infusion and original points, generating the wind by drying the dampness, and the Qi and blood materials are the wind of the heaven's rush, which is hot and dry in nature.
Qi-acupuncture therapy of the TCM can eliminate pleural effusion and ascites, edema of both lower extremities, abdominal wall varices and collateral circulation are the objective indicators for the effective treatment of portal hypertension in cirrhosis[25]. It is helpful to improve the immunity of the body, reduce the enlargement of the spleen,reduce the portal hypertension, so as to reduce or avoid the rupture of the esophageal and gastric fundus vein and hepatic encephalopathy caused. It can effectively reduce the ascites, so as to avoid the occurrence of hepatorenal syndrome and uremia,and effectively reduce the mortality.
REFERENCE
1. The Chinese Research Group on Diagnosis and Detection of Portal Hypertension (CHESS). The Minimally Invasive Intervention Cooperative Group of the Digestive Branch of the Chinese Medical Association,the Emergency Intervention Committee of the Intervention Physician Branch of the Chinese Medical Association, the Chinese Expert Consensus on Clinical Application of Hepatic Vein Pressure Gradient (2018 Edition). Journal of Clinical Hepatobiliary Diseases,2018, 34(12):2526-2536.
2. World Health Organization, Hepatitis B, https://www.who.int/news-room/fact-sheets/detail/hepatitis-b.
3. Xu XY, Ding HG, Li WG, et al. Guidelines for the diagnosis and treatment of liver cirrhosis. Journal of Clinical Hepatobiliary Diseases, 2019, 35(11):2408-2425.
4. Xu LM, Liu P, Shen XZ, et al. Guide to diagnosis and treatment of liver fibrosis with integrated traditional and Western Medicine (2019). Chinese Journal of Integrated Traditional and Western Medicine, 2019,39(11):1286-1295.
5. Liu CH, Wei BH, Yao SK. Consensus on diagnosis and treatment of liver cirrhosis with integrated traditional Chinese and Western Medicine. Chinese Journal of Integrated Traditional and Western Medicine and Digestion, 2011, 19(4):277-279.
6. Chinese expert consensus on clinical application of hepatic vein pressure gradient (2018). Chinese Journal of Digestive Surgery, 2018, 17(11):1059-1070.
7. Society of Hepatology of Chinese Medical Association,Society of Digestive Diseases of Chinese Medical Association, Society of Digestive Endoscopy of Chinese Medical Association. Prevention and treatment of esophagogastric varices bleeding in cirrhotic portal hypertension. Chinese Journal of Internal Medicine,2016, 55(1):57-72.
8. Gao XZ, Hu L. Chinese Dictionary of acupuncture.Nanjing: Jiangsu Science and Technology Press,2010:722.
9. Ayad Ahmad Mohammed. Caput medusae sign; a unique finding during abdominal examination in patients with portal hypertension; case report. Annals of Medicine and Surgery, 2020, 54:54-56.
10. Guadalupe Garcia-Tsao, Juan G. Abraldes, Annalisa Berzigotti, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology,2017, 65(1):310-335.
11. Yi FF, Bai ZH, Xu XB, et al. Research progress of spontaneous splenorenal shunt in patients with cirrhosis. World Journal of Chinese Digestion, 2019,27(24):1502-1508.
12. Xu YB, Geng SH. Clinical research status and progress of portal hypertension in cirrhosis. Clinical Research of Traditional Chinese Medicine, 2017, 9(31):140-143.
13. Carmelo Cicciò, Giovanni Foti, Luigi Romano, et al. The role of diagnostic imaging and interventional radiology in liver schistosomiasis: A case report of advanced disease. Radiology of Infectious Diseases, 2020.
14. Luoto Topi T, Koivusalo Antti I, Pakarinen Mikko P. Long-term Outcomes and Health Perceptions in Pediatric-onset Portal Hypertension Complicated by Varices. Journal of Pediatric Gastroenterology and Nutrition, 2020, 70(5):628-634.
15. Garcia-Tsao Guadalupe, Bosch Jaime, Kayali Zeid, et al. Randomized placebo-controlled trial of emricasan for non-alcoholic steatohepatitis-related cirrhosis with severe portal hypertension. Journal of Hepatology,2020, 72(5).
16. Troisi Roberto Ivan, Vanlander Aude, Giglio Mariano Cesare, et al. Somatostatin as Inflow Modulator in Livertransplant Recipients With Severe Portal Hypertension:A Randomized Trial. Annals of Surgery, 2018.
17. Gu Y, Yang XQ, Liang H, et al. Comprehensive evaluation of effects and safety of statin on the progression of liver cirrhosis: a systematic review and meta-analysis. BMC Gastroenterology, 2019, 19(1).
18. Xu YB. Acupuncture Research on Liver Cirrhosis Portal Hypertension Clinical Curative Effect. World Traditional Chinese Medicine, 2017, 12(1):152-156,160.
19. David Cyranoski. Why Chinese medicine is heading for clinics around the world. Nature, 2018, 561:448-450.
20. Gao XZ, Hu L. Chinese Dictionary of acupuncture.Nanjing: Jiangsu Science and Technology Press,2010: 722.
21. Wang MJ, Zhu J, Yang YQ. Chinese acupuncture book.Zhengzhou: Henan Science and Technology Press,2012:395.
22. Guo ZL, Guo SS. Zusanli. Chinese Acupuncture Points Series: Zusanli. Beijing: China Medical Science and Technology Press, 2012:1-344.
23. Wang W, Dong BQ, Yu H. Effect of acupuncture at Zusanli point on rat model of liver fibrosis. Chinese Journal of Traditional Chinese Medicine Information,2005 (11):23-24.
24. Yang YP, An BQ, Tan QW. Comparative observation on clinical effect of electroacupuncture at Zusanli and Shangjuxu on postoperative abdominal distention.Journal of Zhejiang University of Traditional Chinese Medicine, 2009(2):114-115.
25. Xu YB, Wang BY. Clinical study on the treatment of refractory ascites due to cirrhosis by air acupuncture combined with characteristic drugs. Clinical Study of Traditional Chinese Medicine, 2017, 9(32):20-24.
 World Journal of Integrated Traditional and Western Medicine2020年7期
World Journal of Integrated Traditional and Western Medicine2020年7期
- World Journal of Integrated Traditional and Western Medicine的其它文章
- Effects of Medicated Bamboo Cupping Therapy of Zhuang Nationality Medicine on Long-term Efficacy and Quality of Life in the Treatment of Functional Dyspepsia with Stagnation of Liver Qi and Spleen Deficiency Syndrome
- Rapid Recovery Strategy of Treating Hemorrhoids in Perioperative Period by Multimodal Analgesia with Traditional Chinese Medicine
- Based on FP-Growth Algorithm to Excavate Medication Rule of Chinese Materia Medica for Radiation Esophagitis
- Application Status of Infrarde Thermography in the Evaluation of Curative Effect of Traditional Chinese Medicine
- A Review on Treating Postoperative Perianal Abscess by the TCM External Therapy
- INSTRUCTION FOR AUTHORS
