牙周基础治疗联合曲安奈德口腔软膏对牙龈扁平苔藓的疗效观察
王翔 张鹏 郑丽纯 王文梅 段宁 储志娟

[摘要] 目的 研究分析牙周基础治疗联合曲安奈德外用治疗牙龈扁平苔藓的临床效果。 方法 选择2019年1—9月于南京大学医学院附属口腔医院·南京市口腔医院就诊的牙龈扁平苔藓并伴有慢性牙周炎的患者40例,按随机数字表法分为治疗组和对照组,每组各20例。治疗组牙周基础治疗联合局部涂抹曲安奈德口腔软膏进行治疗,对照组局部涂抹曲安奈德口腔软膏进行治療,两组均用药3个月。观察两组治疗前后疼痛程度、病损面积及总有效率。 结果 不同时间、分组患者疼痛程度不同,且时间、分组存在交互作用,差异有统计学意义(P < 0.05)。进一步两两比较,组内比较:两组治疗后1周、2周、1个月、6个月疼痛程度低于治疗前,差异有统计学意义(P < 0.05);组间比较:治疗后1周、2周,治疗组疼痛程度低于对照组,差异有统计学意义(P < 0.05)。不同时间病损面积不同,差异有统计学意义(P < 0.05),时间、分组存在交互作用,差异有统计学意义(P < 0.05)。进一步两两比较,组内比较:两组治疗后1周、2周、1个月、6个月病损面积小于治疗前,差异有统计学意义(P < 0.05);组间比较:治疗后2周、1个月和6个月治疗组病损面积小于对照组,差异有统计学意义(P < 0.05)。治疗后1周、2周、1个月和6个月治疗组的总有效率高于对照组,差异有统计学意义(P < 0.05)。 结论 牙周基础治疗联合曲安奈德口腔软膏治疗牙龈扁平苔藓短期见效快,维持效果好,长期疗效佳。
[关键词] 口腔扁平苔藓;曲安奈德;牙周基础治疗;临床疗效
[中图分类号] R781.5 [文献标识码] A [文章编号] 1673-7210(2020)10(c)-0130-04
Analysis of clinical effects of initial periodontal treatment and Triamcinolone Acetonide oral ointment on gingival lichen planus
WANG Xiang1 ZHANG Peng2 ZHENG Lichun3 WANG Wenmei1 DUAN Ning1 CHU Zhijuan1
1.Department of Oral Mucosal Diseases, Nanjing Stomatological Hospital Medical School of Nanjing University, Jiangsu Province, Nanjing 210008, China; 2.Department of Periodontal Disease Division, Nanjing Stomatological Hospital Medical School of Nanjing University, Jiangsu Province, Nanjing 210008, China; 3.Department of Preventive Stomatology, Nanjing Stomatological Hospital Medical School of Nanjing University, Jiangsu Province, Nanjing 210008, China
[Abstract] Objective To analyze the clinical effect of periodontal therapy combined with Triamcinolone Acetonide for treatment of lichen planus gingiva. Methods From January to September in 2019, 40 patients affected with gingival lichen planus and chronic periodontitis diagnosed in the clinics of Nanjing Stomatological Hospital Medical School of Nanjing University, according to the random number table method, the patients were randomly divided into the treatment group and the control group, with 20 patients in each group. The treatment group was treated with periodontal therapy combined with topical triamcinolone acetonide oral ointment, while the control group was treated with topical triamcinolone acetonide oral ointment. Both groups were given the drug for three months, the pain degree, lesion area and total effective rate before and after treatment were observed. Results The pain degree of patients in different time and groups was different, and there was interaction between time and groups, and the differences were statistically significant (P < 0.05). Further pair comparison and intra-group comparison: the pain degree of the two groups at one week, two weeks, one month and six months after treatment were lower than those before treatment, and the difference were statistically significant (P < 0.05). Comparison between groups: one week and two weeks after treatment, the pain degree of the treatment group was lower than that of the control group, with statistically significant differences (P < 0.05). The lesion area was different at different times, and the difference was statistically significants (P < 0.05); there was interaction between time and groups, and the difference was statistically significant (P < 0.05). Further pairwise comparison and intra-group comparison: the lesion area at one week, two weeks, one month and six months after treatment were smaller than that before treatment, and the differences were statistically significant (P < 0.05). Two weeks, one month and six months after treatment, the lesion area of the treatment group were smaller than that of the control group, with statistically significant differences (P < 0.05). The total effective rate of the treatment group at one, two weeks, one month and six months after treatment were higher than those of the control group, and the differences were statistically significant (P < 0.05). Conclusion Periodontal basic treatment combined with Triamcinolone Oral Ointment for lichen planus gingival has quick short-term effect, good maintenance effect and good long-term effect.
[Key words] Oral lichen planus; Triamcinolone Acetonide; Initial periodontal treatment; Clinical effect
口腔扁平苔藓(oral lichen planus,OLP)是口腔黏膜病中的常见病、多发病,患病率为0.1%~4.0%[1]。对于OLP的治疗,国内外均将局部使用糖皮质激素作为一线治疗方法[2]。曲安奈德是一种中效糖皮质激素,其外用剂型可局部应用于口腔黏膜病的治疗[3],对OLP患者颊部或舌腹等非角化上皮病损具有较好疗效[4-5],但其对牙龈或硬腭等角化上皮病损效果有限,且长期应用可能耐药,并产生一定的不良反应[6]。
慢性牙周炎(chronic periodontitis,CP)是人类最常见的慢性感染性疾病之一,是成人缺失牙齿的主要原因[7]。CP的主要治疗方法是牙周基础治疗。有研究[8-9]表明,OLP和CP具有一定的临床和分子特征相关性。因此,本研究旨在观察牙周基础治疗联合曲安奈德口腔软膏治疗牙龈扁平苔藓的疗效,为临床治疗OLP提供新的思路和方法。
1 资料与方法
1.1 一般资料
选择2019年1—9月于南京大学医学院附属口腔医院·南京市口腔医院(以下简称“我院”)门诊就诊的OLP并伴有CP的患者40例,其中男14例,女26例;年龄30~65岁,平均(48.78±8.01)岁。治疗组20例,男6例,女14例;平均年龄(48.00±9.44)岁;对照组20例,男8例,女12例;平均年龄(49.55±6.44)岁。两组患者的一般资料比较,差异无统计学意义(P > 0.05),具有可比性。本研究经我院医学伦理委员会批准,批准号:2014NL-002(KS),所有研究对象均知情同意。入选标准:①患有牙龈扁平苔藓[10];②患有轻中度CP[11]。排除标准:①患有血液疾病、自身免疫性疾病、肿瘤、心血管疾病和糖尿病等系统性疾病;②3个月内经过牙周基础治疗;③3个月内服用过激素、抗生素和免疫抑制剂;④对曲安奈德药物过敏史;⑤有其他口腔黏膜疾病;⑥有银汞充填体、补物悬突及修复体等局部刺激因素;⑦3个月内吸烟、嗜酒;⑧处于妊娠期、哺乳期的女性,研究期间有生育计划的女性;⑨智力障碍、认知障碍和精神疾患患者;⑩不能遵守医嘱用药和定期复查的患者。
1.2 方法
按随机数字表法将患者分为治疗组和对照组。对照组:牙龈扁平苔藓局部涂抹曲安奈德口腔软膏(澳美制药厂,曲安奈德含量0.1%,5 g),用量0.1 g/次,3次/d,连续3个月,并对患者进行口腔卫生宣教及饮食指导。治疗组:入组当日,患者接受牙周基础治疗(龈上洁治、龈下刮治和根面平整),所有操作均由同一位工作经验10年以上的牙周专科医师按照标准程序完成。龈上洁治采用超声洁牙机完成,龈下刮治使用P5多功能超声治疗仪,采用中低功率和侧向轻压力操作。龈下刮治后,手工根面平整使用Gracey刮治器。牙龈扁平苔藓局部涂抹曲安奈德口腔软膏(用量、用药方法及疗程同对照组),并进行口腔卫生宣教及饮食指导。
记录所有入组患者的数据,并在治疗后1周、2周、1个月和6个月对疗效进行评价。所有操作均由同一位医生完成。
1.3 评价标准
本研究疗效的判定是根据中华口腔医学会口腔黏膜病专委会制订的OLP疗效评价标准及指南[12-13]。
1.3.1 主观指标 采用直观类比标尺法(visual analogue scale,VAS),计分标准:3:重度疼痛(VAS:7~10分);2:中度疼痛(VAS:4~6分);1:轻度疼痛(VAS:1~3分);0:无疼痛(VAS:0分)[12]。
1.3.2 客观指标 由观察者测算患者病损面积的大小。计分标准:5分:白色条纹伴糜烂面积≥1 cm2;4分:白色条纹伴糜烂面积<1 cm2;3分:白色条纹伴充血或萎缩面积≥1 cm2;2分:白色条纹伴充血或萎缩面积<1 cm2;1分:轻微白色条纹,无充血、萎缩或糜烂面积;0分:无损害[12-13]。
1.3.3 扁平苔藓的疗效标准 显效:充血及糜烂完全消失,白色条纹无或轻微,疼痛完全消失(体征记分为0或1;症状记为0);有效:充血及糜烂面积缩小,白色条纹减少,疼痛減轻(体征和症状记分均有所下降);无效:充血及糜烂无变化或增加,白色条纹无变化或增加,疼痛无减轻或加重(体征和症状记分不变或增加)[12-13]。总有效率=(显效+有效)例数/总例数×100%。
1.4 统计学方法
采用SPSS 17.0统计学软件对所得数据进行统计学分析,计量资料采用均数±标准差(x±s)表示,重复测量资料,采用重复测量设计的方差分析。组间比较采用t检验,计数资料采用例数和百分率表示,组间比较采用χ2检验,两组总有效率的比较采用连续矫正的χ2检验或Fisher′s精确概率法检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 两组治疗前后疼痛程度比较
不同时间、分组患者VAS评分不同,且时间、分组存在交互作用,差异均有统计学意义(P < 0.05)。进一步两两比较,组内比较:治疗组或对照组治疗后1周、2周、1个月、6个月VAS评分低于治疗前,差异有统计学意义(P < 0.05);组间比较:治疗前,两组VAS评分差异无统计学意义(P > 0.05),治疗后1、2周,治疗组VAS评分低于对照组,差异有统计学意义(P < 0.05),治疗后1、6个月,两组VAS评分比较,差异无统计学意义(P > 0.05)。见表1。
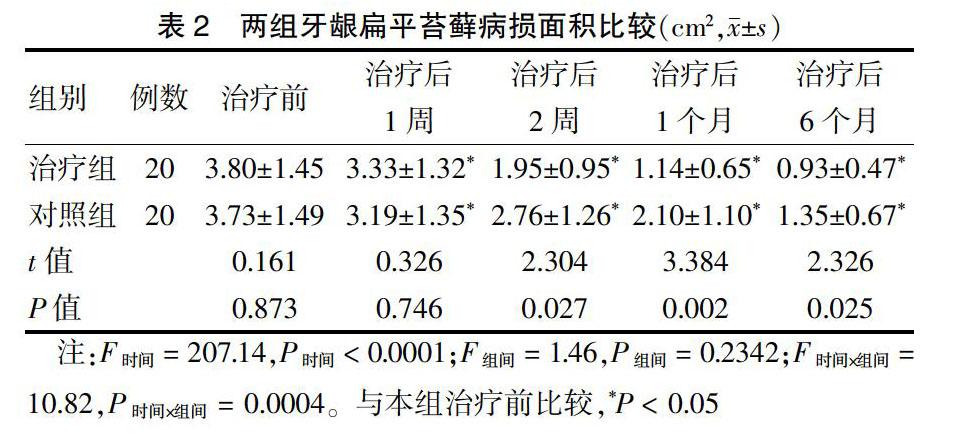
2.2 两组治疗前后病损面积比较
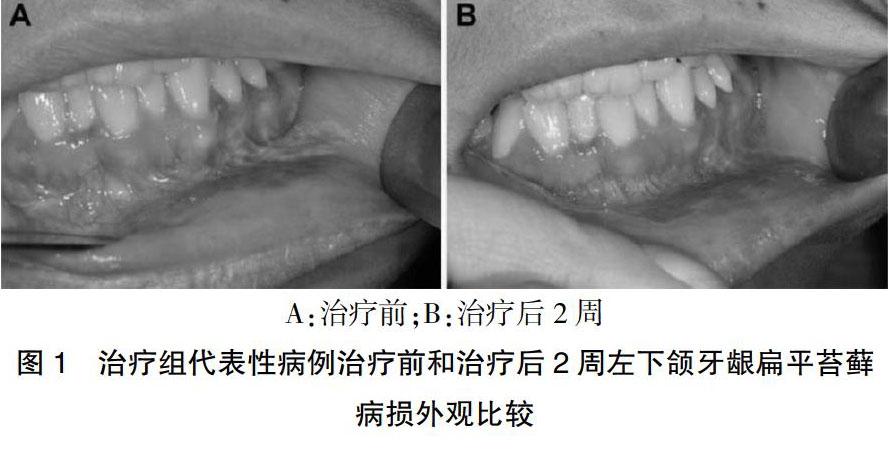
不同时间病损面积不同,差异有统计学意义(P < 0.05),时间、分组存在交互作用,差异有统计学意义(P < 0.05)。进一步两两比较,组内比较:治疗组或对照组治疗后1周、2周、1个月、6个月病损面积小于治疗前,差异有统计学意义(P < 0.05);组间比较:治疗前和治疗后1周,两组病损面积比较,差异无统计学意义(P > 0.05),治疗后2周、1个月和6个月治疗组病损面积小于对照组,差异有统计学意义(P < 0.05)。见表2。治疗组代表性病例经牙龈基础治疗及曲安奈德口腔软膏治疗后2周,牙龈白纹病损面积明显缩小,充血面消退。见图1。
2.3 两组治疗前后总有效率比较
治疗后1周、2周、1个月和6个月,治疗组总有效率均高于对照组(P < 0.05)。见表3。
3 讨论
CP是以菌斑为始动因子的牙周支持组织的慢性感染性疾病。大量研究[14-16]表明,CP与OLP有临床和分子相关性,发病机制和危险因素可能相关。
本研究结果显示,治疗组在治疗后1、2周疼痛程度明显低于对照组,提示牙结石和菌斑等微生物局部刺激因素的彻底清除可快速消退牙龈炎症,从而有助于快速减轻炎症引发的疼痛症状,这与文献报道结果是一致的[17-18]。而两组在治疗后1个月和6个月疼痛程度无明显差异,该结果提示,虽然曲安奈德口腔软膏具有牙龈局部消炎作用,但是起效过慢,究其原因,可能与病原微生物导致的慢性感染和炎症有关[19]。本研究结果还显示,治疗后2周、1个月和6个月治疗组病损面积显著小于对照组,而治疗后1周两组无明显差异,该结果提示OLP病损局部淋巴细胞的聚集和炎症反应的形成是缓慢发生发展的。牙周炎始动因素牙结石和菌斑病原微生物感染源的去除,可能无法消退长期持续的慢性炎症,尚需曲安奈德的消除炎症作用。糖皮质激素通过对多种细胞因子的抑制作用,可迅速减轻炎症反应,缓解OLP的急性症状[20]。CP和OLP病损区分享了病理性的微生态环境,且共有炎症性组织微环境,两者都存在免疫功能障碍的基础[21-24]。CP局部的始动感染因素的刺激促进了OLP发展,反过来CP的基础治疗又影响了OLP的局部微生态和炎症微环境[25]。在对CP治疗后局部刺激因素消除,使得OLP的治疗的进程得以加快。随着疼痛症状的快速减轻,患者的生活质量得到明显提高,对治疗的效果及预后增加了信心,有助于提高治疗依从性[8]。
本研究结果为提高OLP临床疗效提供了新思路,特别是对于牙龈扁平苔藓患者,药物联合牙周基础治疗是必要的,有助于快速增加療效,并维持长期效果。
[参考文献]
[1] Warnakulasuriya S. Oral potentially malignant disorders:A comprehensive review on clinical aspects and management [J]. Oral Oncol,2020,102:104550.
[2] Husein-ElAhmed H,Gieler U,Steinhoff M. Lichen planus:a comprehensive evidence-based analysis of medical treatment [J]. J Eur Acad Dermatol Venereol,2019,33(10):1847-1862.
[3] Fantozzi PJ,Treister N,Shekar R,et al. Intralesional triamcinolone acetonide therapy for inflammatory oral ulcers [J]. Oral Surg Oral Med Oral Pathol Oral Radiol,2019,128(5):485-490.
[4] Lavaee F,Shadmanpour M. Comparison of the effect of photodynamic therapy and topical corticosteroid on oral lichen planus lesions [J]. Oral Dis,2019,25(8):1954-1963.
[5] 刘青兰,刘琳,李留炀,等.曲安奈德口腔软膏治疗充血糜烂型口腔扁平苔藓的疗效及安全性观察[J].实用口腔医学杂志,2017,33(4):536-540.
[6] Brignardello-Petersen R. Important limitations in a trial comparing hyaluronic acid with triamcinolone acetonide for treating oral lichen planus compromise the usefulness of its results [J]. J Am Dent Assoc,2019,150(6):e102.
[7] Silva-Junior MF,Sousa ACC,Batista MJ,et al. Oral health condition and reasons for tooth extraction among an adult population(20-64 years old) [J]. Cien Saude Colet,2017, 22(8):2693-2702.
[8] Rai NP,Kumar P,Mustafa SM,et al. Relation Between Periodontal Status and Pre-Cancerous Condition (Oral Lichen Planus):A Pilot Study [J]. Adv Clin Exp Med,2016,25(4):763-766.
[9] 邱澈,宋忠臣.慢性牙周炎与口腔扁平苔藓相关性研究进展[J].口腔医学,2019,39(12):1144-1148.
[10] 陈谦明.口腔黏膜病学[M].4版.北京:人民卫生出版社,2012:64-65.
[11] 孟焕新.牙周病学[M].4版.北京:人民卫生出版社,2013:168-171.
[12] 周刚,刘宏伟,林梅,等.口腔扁平苔藓(萎缩型、糜烂型)疗效评价标准(试行)[J].中华口腔医学杂志,2005, 40(2):92-93.
[13] 中华口腔医学会口腔黏膜病专业委员会,中华口腔医学会中西医结合专业委员会,周红梅.口腔扁平苔藓诊疗指南(试行)[J].中华口腔医学杂志,2012,47(7):399-401.
[14] Wang H,Han Q,Luo Z,et al. Oral lichen planus may enhance the expression of Th17-associated cytokines in local lesions of chronic periodontitis [J]. Clin Oral Investig,2014,18(6):1647-1654.
[15] Maderal AD,Lee Salisbury P,Jorizzo JL. Desquamative gingivitis:Clinical findings and diseases [J]. J Am Acad Dermatol,2018,78(5):839-848.
[16] 程鳳峡,孙喜龙,杨玉鹏,等.牙周炎伴口腔扁平苔藓中IL-17激活NF-κB调控hPDLFs促进MMPs的分泌[J].实用口腔医学杂志,2019,35(6):805-809.
[17] Alsarraf A,Mehta K,Khzam N. The Gingival Oral Lichen Planus:A Periodontal-Oral Medicine Approach [J]. Case Rep Dent,2019,2019:4659134.
[18] Garcia-Pola MJ,Rodriguez-López S,Fernánz-Vigil A,et al. Oral hygiene instructions and professional control as part of the treatment of desquamative gingivitis. Systematic review [J]. Med Oral Patol Oral Cir Bucal,2019,24(2):e136-e144.
[19] Bianco L,Romano F,Maggiora M,et al. Effect of sonic versus manual supervised toothbrushing on both clinical and biochemical profiles of patients with desquamative gingivitis associated with oral lichen planus:A randomized controlled trial [J]. Int J Dent Hyg,2019,17(2):161-169.
[20] Anitua E,Pi?觡as L,Alkhraisat MH. Histopathological features of oral lichen planus and its response to corticosteroid therapy:A retrospective study [J]. Medicine (Baltimore),2019,98(51):e18321.
[21] Choi YS,Kim Y,Yoon HJ,et al. The presence of bacteria within tissue provides insights into the pathogenesis of oral lichen planus [J]. Sci Rep,2016,6:29186.
[22] Ejaz I,Ghafoor S. WNT signalling pathway in oral lesions [J]. J Pak Med Assoc,2019,69(11):1687-1692.
[23] Wang H,Luo Z,Lei L,et al. Interaction between oral lichen planus and chronic periodontitis with Th17-associated cytokines in serum [J]. Inflammation,2013,36(3):696-704.
[24] Ertugrul AS,Arslan U,Dursun R,et al. Periodontopathogen profile of healthy and oral lichen planus patients with gingivitis or periodontitis [J]. Int J Oral Sci,2013,5(2):92-97.
[25] Romano F,Arduino PG,Maggiora M,et al. Effect of a structured plaque control on MMP-1 and MMP-9 crevicular levels in patients with desquamative gingivitis associated with oral lichen planus [J]. Clin Oral Investig,2019, 23(6):2651-2658.
(收稿日期:2020-03-23)
[基金项目] 国家自然科学基金资助项目(81870767、815709 78);江苏省青年医学重点人才项目(QNRC2016118);江苏省卫生计生委预防医学科研课题(Y2015004);南京市卫生计生委医学科技发展项目(ZKX17033、YKK16162)。
[作者简介] 王翔(1979.12-),男,博士;研究方向:口腔黏膜病学。
[通讯作者] 张鹏(1978.8-),男,硕士;研究方向:牙周病学。

