改良单开门椎板成形术治疗儿童自发性椎管内硬膜外血肿2例分析
赵胜利 李鑫 闵少雄

[摘要] 自发性椎管内硬膜外血肿(SSEH)指不明原因引起的椎管内硬膜外腔内异常积血,该病儿童发病率较低。延迟的手术减压可能造成患儿严重的神经功能障碍甚至终身瘫痪。椎板切除减压血肿引流是治疗SSEH的首选方法,但该方法创伤大,破坏后柱稳定性,在儿童病例中的应用尚存争议。本文报道了2例SSEH儿童病例,最初症状为颈部疼痛或肢体麻木无力,血肿经MRI已证实。入院完善检查后急诊行改良单开门椎板成形血肿引流术,术后患儿颈痛症状消失,神经功能缺损恢复,随访3个月未见明显脊柱后凸畸形。本文旨在強调改良单开门椎板成形术在治疗儿童SSEH中的潜在优势。
[关键词] 自发性椎管内硬膜外血肿;儿童;单开门椎板成形术;治疗;微创手术
[中图分类号] R651.1 [文献标识码] A [文章编号] 1673-7210(2020)03(c)-0160-04
[Abstract] Spontaneous spinal epidural hematoma (SSEH) is an unexplained abnormal accumulation of blood in the spinal epidural space, and the disease has a lower incidence in children. Delayed surgical decompression can lead to severe neurological impairment or even lifelong paralysis. Decompression hematoma drainage by laminectomy is the preferred treatment for SSEH. However, the application of this method in children cases is still controversial because it is highly invasive and damages the stability of posterior column. Two cases of SSEH children with initial symptoms of neck pain or limb numbness and weakness were reported. The hematoma was confirmed by MRI. After complete examination at admission, hematoma drainage with modified single open door laminoplasty was performed in the emergency department. Postoperative symptoms of neck pain disappeared. Recovery of neurological impairment. No obvious kyphosis deformity was found during 3 months of follow-up. This article aims to highlight the potential advantages of improved single-door laminoplasty in the treatment of SSEH in children.
[Key words] Spontaneous spinal epidural hematoma; Children; One-side open door laminoplasty; Treatment; Minimally invasive surgery
自发性椎管内硬膜外血肿(SSEH)是引起脊髓压迫的少见原因。根据既往报道,只有10%的SSEH患儿有明确的病因[1]。SSEH的临床表现与脑膜炎[2]、蛛网膜下腔出血[3]、格林-巴利综合征(GBS)[4-5]或脑瘫[6]相似,但与以上疾病比较,SSEH对脊髓的压迫更直接、更迅速。手术时间窗和术前神经功能状态是目前公认的影响预后的重要因素[7-8]。然而,与成年人比较,儿童似乎更能忍受脊髓压迫,及时的外科减压更有可能恢复失去的神经功能[6,9]。儿童处于生长发育关键时期,传统椎板切除减压术创伤大,术后脊柱失稳风险高,手术方法的正确选择对儿童未来成长和发展将产生深远的影响[10]。本文报道2例儿童SSEH病例,我们采用改良的单开门椎板成形术引流血肿,术后影像学检查证实血肿得到充分引流,患儿疼痛和神经功能缺损症状得到完全恢复。现报道如下:
1 病例资料
1.1 病例1
患儿男,7岁,因“摔倒后颈痛16 d,右上肢麻木无力3 d”于2017年1月25日来南方医科大学珠江医院(以下简称“我院”)脊柱外科就诊。患者伤后即至当地医院就诊,予以保守治疗(具体不详),效果欠佳。近3 d症状加重,逐渐出现右上肢麻木无力。我院脊柱外科查体示:右上肢肘关节以下尺侧感觉减退,肌力Ⅳ级,右侧臂丛牵拉试验(+),双下肢肌张力高,腱反射活跃。实验室检查(如血小板计数、凝血酶原时间、活化部分凝血活酶时间、肝肾功能等)结果未见明显异常。入院后即行头颈CT检查,示C6~T1椎管内硬膜外等密度团块,临近脊髓受压。MRI检查示C6~T1矢状位短T1、长T2信号改变,增强扫描为高信号,脊髓向左后方移位明显,并出现缺血性改变(图1A、B、C)。诊断为脊柱椎管内硬膜外血肿(急性或亚急性期)。立即行C6~T1改良开门椎板成形血肿引流术。手术过程简述如下:麻醉成功后,患儿取俯卧位,头稍前屈。常规碘伏消毒,铺无菌单,贴无菌膜。取颈部后正中切口,长约6 cm,切开皮肤、皮下组织及颈项筋膜,沿棘突行骨膜下剥离,显露C6~T2棘突、椎板和双侧侧块。用磨钻将C6~T1右侧椎板与侧块结合处磨断,磨去左侧椎板与侧块结合处外侧皮质,保留内侧皮质。将椎板向左侧打开。此时,大量黑褐色陈旧性血液经间隙流出。显露硬膜囊,大量生理盐水冲洗。可见硬膜囊表面已无积血,搏动良好。将打开的椎板复原,用丝线将棘突与左侧椎旁肌缝合。冰盐水冲洗创面,确定无活动性出血。放置负压引流管1根,纱布、棉片及器械清点无误后逐层缝合切口,无菌纱布包扎,颈围外固定,术毕。术后第1天,患者右上肢麻木症状改善,11 d后肌力恢复。术后复查MRI(图1D、E、F)示血肿引流彻底,未见脊柱后凸畸形。
1.2 病例2
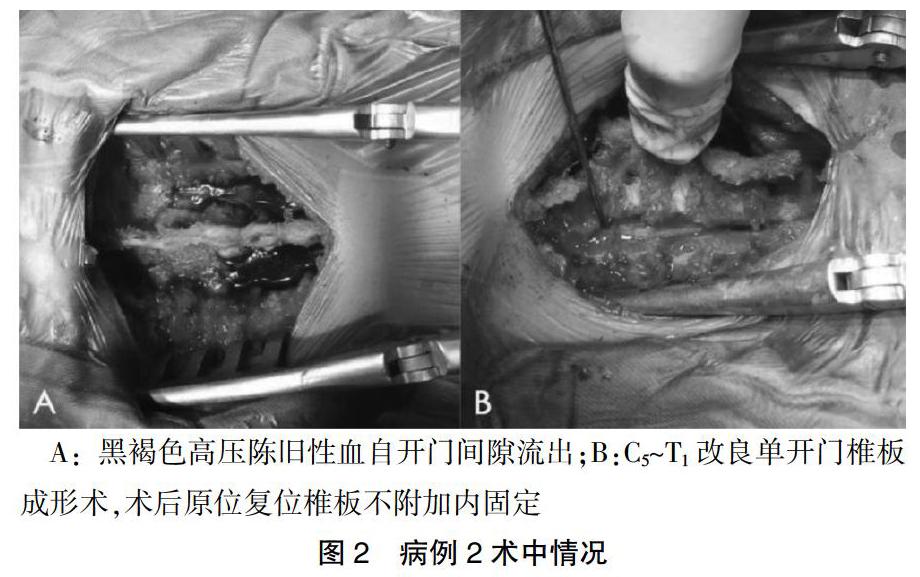
患儿女,4岁,因“颈痛伴双上肢无力1周”于2016年12月29日入我院。患儿病后曾于当地医院行牵引治疗,未见好转。双手无力症状几天来逐渐加重。当地医院头颈CT检查示椎管占位。我院脊柱外科查体示臂丛神经牵拉试验(+),双上肢肌力Ⅲ级,双下肢肌力正常,肌张力高,腱反射活跃,病理征(-)。血液常规、生化、肝肾功能、凝血6项等实验室检验结果正常。入院当天行头颈MRI检查评估脊髓受压情况,提示脊髓腹侧硬膜外间隙梭形肿块,从C6延伸至T3,高度怀疑急性硬膜外血肿。综合评估后行C5~T1改良单开门椎板成形血肿引流术。术中磨钻磨去右侧椎板外皮质,左侧椎板与侧块结合处切断椎板,黑褐色高压陈旧性血液自间隙流出(图2A,B)。患者术后恢复良好。第8天出院时双上肢肌力完全恢复。术后3个月复查MRI提示脊髓前仍有少量血肿,但患者颈部活动良好,无神经功能缺损。
2 讨论
SSEH是一种可能导致永久性残疾的少见疾病。该病多见于中年人,随着辅助检查技术的提高,SSEH在儿童中的诊断率逐渐提高[7,11-12]。动静脉畸形(AVM)[13-14]和凝血障碍[15]是SSEH的常见病因,镰状细胞病[16]和轻微外伤[17]偶有报道。Yu等[18]分析了55例患者,平均年龄(31.8±15.7)岁,认为血肿多位于颈段和胸段。在儿童中,血肿常见于C5~T1[19]。颈、胸段缺乏静脉瓣结构,该区域后静脉丛大于腰段[20]。同时,颈胸交界处活動范围大,臂丛自该区域穿行。这一特殊位置提示SSEH的发生与颈段和胸段的解剖学因素有关。
MRI可清楚显示血肿的位置、范围、与邻近组织的关系、脊髓水肿[20]、异常扩张的硬膜外血管[14],推测血肿形成时间,甚至预测预后[21-22]。Skin等[23]对15例脊髓动静脉瘘(AVF)患者进行MRI检查,发现其中14例(93.3%)患者T2加权像呈现典型的“流动征”。Parla等[24]和Min等[6]报道了基于MRI发现高度怀疑AVM的患者,随后的脊髓造影或术后病理检查证实了诊断。Ratre等[8]建议在大多数情况下应优先行影像学检查,当影像学检查未提示明显的血管畸形时,无需再进行血管造影,因为在紧急情况下,有创检查将延误及时治疗。
SSEH的治疗目标是及时解除脊髓压迫,可以保守治疗,也可以采取手术。当体格检查及影像学检查证实非严重神经压迫患者,可采取保守治疗,分以下两种情况:①病因明确,查体未见明显神经缺损症状,或影像学未提示明显血肿压迫[25],类似Rathi等[26]的报道;②病因不明,但最初症状轻微,或最初症状严重,但恢复迅速[27]。Kim等[28]建议,对于初始ASIA分级为E,或初始ASIA分级为C或D但有早期恢复迹象的患者,可采用保守治疗。然而,临床大多情况下患儿问诊不清晰,查体不能配合,无法及时准确评估最初神经功能状态。因此,很难判断保守治疗在短期内是否有效。为了避免可能的永久性神经损伤,建议在高度怀疑SSEH时积极行术前准备。
椎板切除术是SSEH的一线治疗方法,可以实现脊髓压迫部位的直接减压和彻底的血肿引流[12,22,28-29],该方法同样适用于儿童[19]。然而,该手术最大的缺点是它对脊柱机械稳定性的影响。整个椎板、部分关节面和韧带的切除在脊柱失稳的发生或进展中起着重要作用[10]。这种风险在儿童中可能更为突出。在儿童发育过程中,涉及颈椎和胸椎手术可能导致胸椎后凸增加[29-30]。为减少脊柱失稳的发生,有学者建议只要适应证允许,应行部分椎板切除或跨节段椎板切除术[10]。椎板成形术是一种比椎板切除术创伤更小的脊髓减压技术,但在以往的报道中很少采用这种方法清除血肿。在本报道的2例病例中,使用该方法治疗儿童SSEH。切开患侧椎板,而另一侧仍保留着内侧皮质。可见黑褐色高压陈旧性血自间隙流出。用生理盐水彻底冲洗创面,椎板复位不固定,棘突与椎旁肌缝合。该方法相比传统椎板切除术创伤小、术中出血少、手术时间缩短,对脊柱后柱稳定性影响较小。本文报道的2例患者在术后3个月的随访过程中均未发现任何脊柱畸形或血肿复发的迹象。
近年来,有学者报道采取更加微创的方法治疗SSEH。Tanriverdi等[31]描述在血肿中间去除一个节段的椎板,使用软导管经硬膜外腔达血肿两端,生理盐水持续冲洗。术后复查颈胸MRI检查显示血肿得到完全清除。Fu等[32]使用管状牵开器到达病变部位,达到血肿部位直接减压,从而尽可能避免了手术部位骨结构和软组织损伤。术中出血量仅50 mL,术后MRI显示血肿完全清除。建议术前应充分考虑患者年龄、血肿部位、长度及性质,选择合适的外科干预手段,在适应证允许的情况下,应积极推广使用更加微创的方法来降低继发性创伤和长期并发症的发生率。
综上所述,儿童SSEH是一种少见的急诊病例。早期诊断、制订个体化手术方案、及时减压可以改善疾病预后。MRI是一种可靠的早期诊断工具。改良单开门椎板成形术相对于椎板切除创伤小,对脊柱稳定性影响小,能达到血肿的彻底引流,可能是治疗儿童SSEH的更佳选择。
[参考文献]
[1] D′Angelo V,Bizzozero L,Talamonti G,et al. Value of magnetic resonance imaging in spontaneous extradural spinal hematoma due to vascular malformation:case report [J]. Surg Neurol,1990,34:343-344.
[2] Schoonjans AS,De DJ,Kenis S,et al. Spontaneous spinal epidural hematoma in infancy:review of the literature and the "seventh" case report [J]. Eur J Paediatr Neurol,2013, 17(6):537-542.
[3] Aristedis R,Dimitrios B. Spinal epidural hematoma mimicking subarachnoid hemorrhage:A case study [J]. Surg Neurol Int,2017,8(1):182-184.
[4] Lee CH,Song GS,Kim YH,et al. Spontaneous Spinal Epidural Hematoma Coexisting Guillan-Barré Syndrome in a Child:A Case Report [J]. Korean J Spine,2016,13(3):167-169.
[5] Kondo A,Yamaguchi H,Ishida Y,et al. Spontaneous spinal epidural hematoma mimicking Guillain-Barre Syndrome [J]. Brain Dev-Jpn,2019,41(4):392-395.
[6] Min S,Duan Y,Jin A,et al. Chronic spontaneous cervicothoracic epidural hematoma in an 8-month-old infant [J]. Ann Saudi Med,2011,31(3):301-304.
[7] Wang M,Zhou P,Jiang S. Clinical Features,Management,and Prognostic Factors of Spontaneous Epidural Spinal Hematoma:Analysis of 24 cases [J]. World Neurosurg,2017,102:360-369.
[8] Ratre S,Yadav Y,Choudhary S,et al. Spontaneous ventral spinal epidural hematoma in a child:A case report and review of literature [J]. J Neurosci Rural Pract,2016,7(2):297-299.
[9] Tewari MK,Tripathi LN,Mathuriya SN,et al. Spontaneous spinal extradural hematoma in children [J]. Childs Nerv Syst,1992,8(1):53-55.
[10] Iida Y,Kataoka O,Sho T,et al. Postoperative lumbar spinal instability occurring or progressing secondary to laminectomy [J]. Spine,1990,15(11):1186-1189.
[11] Ravid S,Schneider S,Maytal J. Spontaneous spinal epidural hematoma:an uncommon presentation of a rare disease [J]. Child′s Nerv Syst,2002,18(6/7):345-347.
[12] Liu Z,Jiao Q,Xu J,et al. Spontaneous spinal epidural hematoma:analysis of 23 cases [J]. Surg Neurol,2008,69(3):253-260.
[13] Paraskevopoulos D,Magras I,Polyzoidis K. Spontaneous spinal epidural hematoma secondary to extradural arteriovenous malformation in a child:a case-based update [J]. Child Nerv Syst,2013,29(11):1985-1991.
[14] Kitagawa RS,Mawad ME,Whitehead WE,et al. Paraspinal arteriovenous malformations in children [J]. J Neurosurg Pediatr,2009,3(5):425-428.
[15] Dildar N,Ayaz SB,Aamir MO,et al. Spontaneous spinal epidural hemorrhage following disseminated intravascular coagulation resulting in paraplegia:a case report [J]. J Spinal Cord Med,2017,42(2):265-269.
[16] Sathyamoorthy M,Walker B,Rhodes MM,et al. Spinal epidural hematoma following a thoracic epidural in a child with sickle cell disease [J]. Clin Case Rep,2017,5(7):1115-1118.
[17] Chang HJ,Su FJ,Huang YC,et al. Spontaneous spinal epidural hemorrhage from intense piano playing [J]. Am J Emerg Med,2014,32(6):688.e3-e5.
[18] Yu JX,Liu J,He C,et al. Spontaneous spinal epidural hematoma:a study of 55 cases focused on the etiology and treatment strategy [J]. World Neurosurg,2016,98:546-554.
[19] Patel H,Boaz JC,Phillips JP,et al. Spontaneous spinal epidural hematoma in children [J]. Pediatr Neurol,1998,19(4):302-307.
[20] Gala F,Aswani Y. Imaging in spinal posterior epidural space lesions:A pictorial essay [J]. Indian J Radiol Imaging,2016,26(3):299-315.
[21] Martínez-Pérez R,Paredes I,Rayo N,et al. Factors predicting outcome of surgical treatment of spontaneous spinal hematomas:a retrospective cohort study in four tertiary reference centers [J]. J Neurosurg Sci,2017. DOI:10.23736/s0390-5616.17.03975-3.
[22] Ghasemi A,Haddadi K,Shad AA. Comparison of Diagnostic Accuracy of MRI with and Without Contrast in Diagnosis of Traumatic Spinal Cord Injuries [J]. Medicine (Baltimore),2015,94(43):1942-1947.
[23] Shin DA,Park KY,Ji GY,et al. The Use of Magnetic Resonance Imaging in Predicting the Clinical Outcome of Spinal Arteriovenous Fistula [J]. Yonsei Med J,2015,56(2):397-402.
[24] Parla G,Ameh V. Cervical spine arterio venous malformation [J]. BMJ Case Rep,2013. DOI:10.1136/bcr-2012-006928.
[25] Gundag M,Hakan M,Dogan K,et al. Spontaneous Resolution of Paraparesis Because of Acute Spontaneous Thoracolumbar Epidural Hematoma [J]. Iran Red Crescent Med J,2012,14(1):45-48.
[26] Rathi N,Rathi A. Haemophilia A presenting as spontaneous spinal epidural haematoma in a 3-month-old infant [J]. BMJ Case Rep,2010,2010(10):e25494.
[27] Soltani S,Nogaro MC,Rougelot C,et al. Spontaneous spinal epidural haematomas in children [J]. Eur Spine J,2019,28(7):1-8.
[28] Kim T,Lee CH,Hyun SJ,et al. Clinical Outcomes of Spontaneous Spinal Epidural Hematoma:A Comparative Study between Conservative and Surgical Treatment [J]. J Korean Neurosurg Soc,2012,52(6):523-527.
[29] Kreppel D,Antoniadis G,Seeling W. Spinal hematoma:a literature survey with meta-analysis of 613 patients [J]. Neurosurg Rev,2003,26(1):1-49.
[30] Yasuoka S,Peterson HA,Maccarty CS. Incidence of spinal column deformity after multilevel laminectomy in children and adults [J]. J Neurosurg,1982,57(4):441-445.
[31] Tanriverdi O,Gungor A,Coban MK,et al. A New Less Invasive Technique for Multiple-Level Spontaneous Spinal Epidural Hematomas:Wash-and-Go Technique [J]. J Neurol Surg A Cent Eur Neurosurg,2016,78(2):198-201.
[32] Fu CF,Zhuang YD,Chen CM,et al. Spontaneous spinal epidural hematoma management with minimally invasive surgery through tubular retractors:A case report and review of the literature [J]. Medicine (Baltimore),2016,95(26):3906-3910.
(收稿日期:2019-11-25 本文編辑:封 华)