淋巴血管间隙浸润与子宫内膜癌预后的相关性研究
杨倩 周怀君 凌静娴 李荣 韩克 朱湘虹 汤晓秋


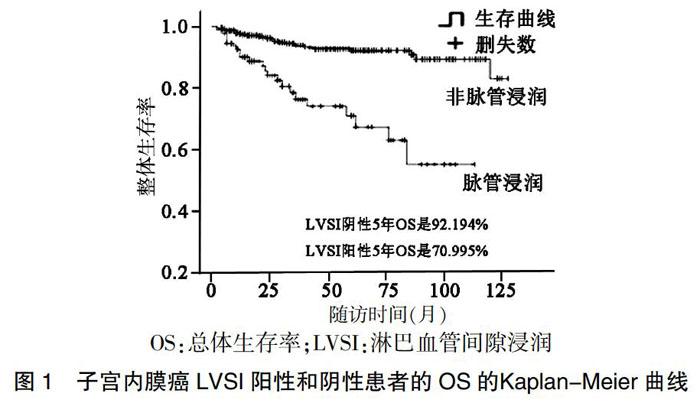
[摘要] 目的 研究淋巴血管間隙浸润(LVSI)的子宫内膜癌的临床病理特征,以及与预后的相关性。 方法 回顾性分析2007年1月~2017年12月在南京鼓楼医院治疗的671例子宫内膜癌患者的病例资料,其中LVSI阳性组120例,LVSI阴性组551例;分析患者的临床病理信息,建立Kaplan-Meier曲线,并进行单因素和多因素分析。结果 与LVSI阴性组比较,LVSI阳性组已绝经、手术病理期别晚、深肌层浸润、组织分化差、伴淋巴结转移、发生复发及死亡患者占比升高,差异有统计学意义(P < 0.05);两组有内科合并症(高血压、糖尿病)或子宫肌瘤患者占比比较,差异无统计学意义(P > 0.05 )。多因素分析结果显示,宫颈间质累及(OR = 0.342, 95%CI:0.134~0.873,P < 0.05)、LVSI(OR = 0.110,95%CI:0.051~0.238,P < 0.01)与淋巴结转移显著相关;生存率分析结果表明,在LVSI阳性的患者中,总生存率和无复发生存率均显著降低(P < 0.05);COX回归结果显示,手术期别晚、非内膜样癌、LVSI影响子宫内膜癌患者的生存时间及结局(P < 0.05)。 结论 LVSI与淋巴结转移密切相关,可作为预测淋巴结转移的重要因素;LVSI是子宫内膜癌不良预后的重要危险因素。
[关键词] 子宫内膜癌;淋巴血管间隙浸润;Kaplan-Meier曲线
[中图分类号] R737.33 [文献标识码] A [文章编号] 1673-7210(2019)07(b)-0091-04
Correlation between lymphovascular space invasion and prognosis of endometrial carcinoma
YANG Qian1,2 ZHOU Huaijun1,3 LING Jingxian3 LI Rong3 HAN Ke3 ZHU Xianghong3 TANG Xiaoqiu3
1.Drum Tower Clinical Medical College of Nanjing Medical University, Jiangsu Province, Nanjing 210008, China; 2.Department of Obstetrics and Gynecology, Nanjing Pukou Hospital, Jiangsu Province, Nanjing 210031, China; 3.Department of Gynecology, Nanjing Drum Tower Hospital, Jiangsu Province, Nanjing 210008, China
[Abstract] Objective To study the clinicopathological features and prognosis of endometrial carcinoma with lymphovascular space invasion (LVSI). Methods The data of 671 cases of endometrial carcinoma treated in Nanjing Drum Tower Hospital from January 2007 to December 2017 was retrospectively analyzed, including 120 cases in LVSI positive group and 551 cases in LVSI negative group. The clinicopathological information of patients was analyzed, and Kaplan-Meier curves were established. Univariate and multivariate analyses were performed. Results Compared with LVSI negative group, LVSI positive group was significantly higher in proporation of patients with menopause, late stage of operation and pathology, infiltration of deep muscle layer, poor tissue differentiation, lymph node metastasis, recurrence and death, the differences were statistically significant (P < 0.05). There was no statistical difference between the two groups in the proporation of patients with medical complications of hypertension, diabetes and uterine leiomyoma (P > 0.05). Multivariate analysis showed that cervical stroma involvement (OR = 0.342, 95%CI: 0.134-0.873, P < 0.05) and LVSI (OR = 0.110, 95%CI: 0.051-0.238, P < 0.01) were significantly correlated with lymph node metastasis. Survival rate analysis showed that both OS and RFS were significantly decreased in LVSI positive patients (P < 0.05). The results of COX regression showed that the survival time and outcome of endometrial carcinoma were affected by the late stage of operation and pathology, the nonendometrial carcinoma and LVSI (P < 0. 05). Conclusion LVSI is closely related to lymph node metastasis and may be an important predictor of lymph node metastasis. LVSI is an important risk factor for poor prognosis of endometrial carcinoma.
[Key words] Endometrial carcinoma; Lymphovascular space invasion; Kaplan-meier curve
子宫内膜癌是女性生殖系统三大恶性肿瘤之一,占女性恶性肿瘤的7%,居女性生殖系统恶性肿瘤的20%~30%[1],且发病率越来越高。有些学者研究发现,淋巴血管间隙浸润(lymphovascular space invasion,LVSI)是子宫内膜癌患者不良预后的独立影响因素[2-4],该指标可作为子宫内膜癌患者术后进行辅助治疗的重要参考指征。因此,本项研究选取南京鼓楼医院671例子宫内膜癌患者的临床病理资料进行回顾性分析,总结LVSI的特征,分析其与淋巴结转移之间的相关性,评估其在子宫内膜癌术后治疗及预后诊断中的重要临床价值。
1 资料与方法
1.1 一般资料
选择2007年1月~2017年12月在南京鼓楼医院妇科治疗的、有完整的临床病理资料的、经术后病理学确诊为子宫内膜癌的671例患者的临床资料,其中有完整随访资料的是555例。排除标准:①疑似病例,缺少术后病理学证实诊断;②术前接受过放化疗或激素治疗以及此次于南京鼓楼医院行再次手术治疗的病例;③子宫内膜癌为转移性癌的病例;④临床、病理资料缺失的病例。671例患者中有LVSI的120例,占17.9%。统计相关临床病理资料:发病年龄、绝经情况、内科合并症(高血压、糖尿病史)、子宫肌瘤、手术病理分期期别、组织病理类型、组织分化程度、淋巴结转移情况、术后是否复发以及复发的时间、部位以及生存结局状态等。
1.2 方法
根据《WHO子宫体肿瘤组织学分类(2014)》[5-6]标准进行组织学分型,将子宫内膜癌分为内膜样癌和非内膜样癌,非内膜样癌中的浆液性乳头状癌、透明细胞癌等归属组织低分化类[7];手术病理分期采用国际妇产科联盟(FIGO 2009)最新分期标准进行[8]。随访采用门诊及电话随访相结合,截至2018年4月1日。
1.3 统计学方法
采用SPSS 19.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验及Wilcoxon秩和检验;计数资料用率表示,组间比较采用χ2检验或Fisher精确检验。采用单因素、多因素的COX回归分析方法及Log-rank检验进行相关性分析,建立Kaplan-Meier生存曲线进行生存率分析。以P < 0.05为差异有统计学意义。
2 结果
2.1 LVSI与子宫内膜癌患者的临床病理特征的关系
671例子宫内膜癌患者发病的中位年龄是57.35岁(24~88岁),术后常规病理报告证实120例伴有LVSI,阳性率为17.9%(120/671)。671例患者中成功随访的有555例,术后复发82例,术后死亡52例;绝经、手术病理分期Ⅲ~Ⅳ期、组织分化程度差(中、低分化)、非内膜样癌以及淋巴结发生转移的子宫内膜癌患者,容易同时发生LVSI(P < 0.05)。与LVSI阴性组比较,LVSI阳性组淋巴结转移、复发及死亡率显著升高,差异有高度统计学意义(P < 0.01);两组在是否有子宫肌瘤及内科合并症(高血压、糖尿病)方面,差异无统计学意义(P > 0.05)。见表1。
2.2 LVSI与淋巴结转移的相关性研究
发生淋巴结转移是患者术后复发及死亡的重要危险因素,通过单因素条件的Logistic回归筛选出与淋巴结转移相关的因素分别有肌层浸润、宫颈间质累及、LVSI、年龄≥65岁,在此基础上进行多因素Logistic回归分析,结果提示宫颈间质累及、LVSI是子宫内膜癌淋巴结转移的影响因素(P < 0.05)。见表2。
2.3 有LVSI和无LVSI的子宫内膜癌患者生存率比较
随访成功的555例子宫内膜癌病例,术后复发82例,术后死亡52例,采用Kaplan-Meier曲线和对数秩检验,分别計算有LVSI、无LVSI患者的5年总体生存率(OS)及无复发生存率(RFS),并评估其差异性。结果提示,无LVSI组5年OS为92.194%,LVSI组5年OS为70.995%(P < 0.001),见图1。无LVSI组5年RFS为88.938%,LVSI组5年RFS为61.658%。(P < 0.001),见图2。
2.4 555例子宫内膜癌的OS和RFS的Cox风险回归分析
采用单因素Cox回归方法分析影响OS和RFS的相关因素,结果显示年龄≥65岁、LVSI、非内膜样癌、手术期别晚(Ⅲ~Ⅳ期)与内膜癌RFS增高明显相关(P < 0.01)。见表3。将这些因素应用于多因素Cox回归分析,结果显示手术期别晚、非内膜样癌、LVSI阳性与RFS增高显著相关(P < 0.01);而年龄≥65岁、非内膜样癌、手术期别晚与总体OS下降显著相关(P < 0.05)。见表4。
3 讨论
LVSI又称脉管浸润,即脉管内可见癌栓,包括淋巴管壁或血管壁上有癌细胞,常提示癌细胞发生转移扩散,表明其发生远处转移的概率大[9-10],多项研究证明,子宫内膜癌的LVSI与淋巴结转移相关[10],LVSI能更早地提示淋巴结转移的潜在危险,是影响内膜癌预后的独立因素[2-4,10]。本研究结果显示,在已绝经、手术病理分期在Ⅲ~Ⅳ期、组织分化程度差、特殊类型内膜癌以及淋巴结转移的子宫内膜癌患者中发生LVSI阳性占比显著增高。82例术后复发的子宫内膜癌患者中,伴LVSI阳性者32例(33.7%);发生死亡的52例子宫内膜癌患者中,LVSI阳性者22例(23.2%),提示LVSI子宫内膜癌患者术后有着显著的高复发率及高死亡率。这与既往国外的研究[11-15]结果相一致。
众所周知,发生淋巴结转移是子宫内膜癌已知的不良预后因素[16-18],本次研究采用单因素、多因素多层分析的方法,对与淋巴结转移相关的因素进行比较,结果提示发生宫颈间质累及、发生LVSI与淋巴结转移密切相关。本次研究的病例中,淋巴结阳性的38例患者中,LVSI阳性者25例,占65.8%,LVSI与淋巴结转移相关度高,是其重要预测因素。数位学者对于LVSI在早期子宫内膜癌中的预后意义进行过一系列的研究,总结出LVSI在无淋巴结转移的早期内膜癌中,其OS有显著差异[19-20]。Jorge等[21]也指出对于无淋巴结转移的子宫内膜癌患者,LVSI是OS降低的显著指标;另一项研究[22]也证实,对于未发生淋巴结转移的早期复发的子宫内膜癌患者,LVSI是疾病复发的重要预测因子。本次回顾的病例资料中,淋巴结阴性633例,发生LVSI者95例,占15%,同样对其进行生存率分析,显示在淋巴结阴性的有LVSI内膜癌患者的OS和RFS均明显降低,进一步证实LVSI、淋巴结转移在评估子宫内膜癌预后中均具有重要价值。
通过对影响生存率及复发率的单因素分析,本研究发现,LVSI作为一个单一的预后因素也与复发时间缩短和OS下降显著相关;在多因素分析中,其他因素(如年龄≥65岁、合并基础疾病、手术分期、肿瘤组织类型、肿瘤组织分化程度)进行调整后,LVSI是术后复发的重要预测因素,但不会导致明显OS的下降,分析此结果的出现,与临床治疗中LVSI已成为医生判断术后复发重要的危险指标,在手术后即联合进一步辅助治疗,故对本研究中的统计资料进行的多因素分析中,LVSI对OS下降的影响不明显;而年龄≥65岁对术后RFS升高影响小,但在OS下降的预测因素中占有重要作用,与高龄本身引起的自然死亡致OS下降有叠加效应。
综上所述,LVSI与淋巴结转移密切相关,可作为预测淋巴结转移的重要因素;LVSI是子宫内膜癌不良预后的重要危险因素[22-23],尤其对于早期、淋巴结阴性的子宮内膜癌患者,进行辅助治疗的决策和术后复发风险的评估、生存时间的评估等方面,LVSI的结果具有重要的指导作用。
[参考文献]
[1] Desantis CE,Siegel RL,Sauer AG,et al. Cancer statistics for African Americans,2016:Progress and opportunities in reducing racial disparities [J]. CA Cancer J Clin,2016,66(4):290-308.
[2] Bri?觕t JM,Hollema H,Reesink N,et al. Lymphvascular space involvement:an independent prognostic factor in endometrial cancer [J]. Gynecol Onco,2005,96(3):799-804.
[3] Guntupalli SR,Zighelboim I,Kizer NT,et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer [J]. Gynecol Onco,2012,124(1):31-35.
[4] Sahin H,Sarioglu FC,Bagci M,et al. Preoperative magnetic resonance volumetry in predicting myometrial invasion,lymphovascular space invasion,and tumor grade:is it valuable in international federation of gynecology and obstetrics stage i endometrial cancer? [J]. Int J Gynecol Cancer,2018,28(4):666.
[5] Kurman RJ,Carcangiu ML,Herrington CS,et al. WHO classification of tumours of female reproductive organs [M]. Lyon:IARC,2014.
[6] 许春伟,张博,薛卫成.WHO(2014)子宫颈肿瘤组织学分类[J].临床与实验病理学杂志,2014,30(11):1326
[7] 谢幸,苟文丽.妇产科学[M].8版.北京:人民卫生出版社,2013.
[8] Pecorelli S,Zigliani L,Odicino F. Revised FIGO staging for carcinoma of the cervix[J]. Int J Gynaecol Obstet,2009, 105(2):0-108.
[9] Bacac M,Stamenkovic I. Metastatic cancer cell [J]. Annu Rev Pathol,2008,3(3):221.
[10] Han SS,Lee SH,Kim DH,et al. Evaluation of preoperative criteria used to predict lymph node metastasis in endometrial cancer [J]. Acta Obstet Gynecol Scand,2011, 89(2):168-174.
[11] Colombo N,Creutzberg C,Amant F,et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer:diagnosis,treatment and follow-up [J]. Int J Gynecol Cancer, 2016,26(1):2-30.
[12] Creutzberg CL,van Putten WL,Koper PC,et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma:multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma [J]. Lancet, 2000,355(9213):1404-1411.
[13] Keys HM,Roberts JA,Brunetto VL,et al. A phase Ⅲ trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma:a Gynecologic Oncology Group study [J]. Gynecol Onco,2004,92(3):744-751.
[14] Pecorelli S. Revised FIGO staging for carcinoma of the vulva,cervix,and endometrium [J]. Int J Gynaecol Obstet,2009,105(2):107-108.
[15] Narayan K,Khaw P,Bernshaw D,et al. Prognostic significance of lymphovascular space invasion and nodal involvement in intermediate- and high-risk endometrial cancer patients treated with curative intent using surgery and adjuvant radiotherapy [J]. Int J Gynecol Cance,2012, 22(2):260.
[16] Puljiz M,Puljiz ,Danoli D,et al. Prognostic value of lymphovascular space invasion in endometrial cancer [J]. Med Glas (Zenica),2012,10(2):288-292.
[17] 董洪芳.子宮内膜癌临床病理特点与淋巴结转移的相关性分析[J].实用癌症杂志,2017,32(5):811-813.
[18] 杨菁,雷源,邢辉,等.子宫内膜癌伴卵巢转移影响因素分析[J].中国医药导报,2017,14(14):73-76.
[19] Cusano E,Myers V,Samant R,et al. Prognostic Significance of Lymphovascular Space Invasion in the Absence of Lymph Node Metastases in Early-Stage Endometrial Cancer [J]. Int J Gynecol Cancer,2018:1.
[20] Aristizabal P,Graesslin O,Barranger E,et al. A suggested modification to FIGO stage I endometrial cancer [J]. Gynecol Onco,2014,133(2):192-196.
[21] Jorge S,Hou JY,Tergas AI,et al. Magnitude of risk for nodal metastasis associated with lymphvascular space invasion for endometrial cancer [J]. Gynecol Onco,2016, 140(3):387-393.
[22] 徐珍,彭芝兰,曾俐琴,等.358例子宫内膜癌手术方式及影响预后的危险因素分析[J].实用妇产科杂志,2015, 31(4):274-277.
[23] Neal SA,Graybill WS,Garrett-Mayer E,et al. Lymphovascular space invasion in uterine corpus cancer:What is its prognostic significance in the absence of lymph node metastases? [J]. Gynecol Onco,2016,142(2):278-282.