Tonsil-derived stem cells as a new source of adult stem cells
Kyung-Ah Cho,Hyun Jung Lee,Hansaem Jeong,Miri Kim,Soo Yeon Jung,Hae Sang Park,Kyung-Ha Ryu,Seung Jin Lee,Byeongmoon Jeong,Hyukjin Lee,Han Su Kim
Kyung-Ah Cho,Department of Microbiology,College of Medicine,Ewha Womans University,Seoul 07985,South Korea
Hyun Jung Lee,Byeongmoon Jeong,Department of Chemistry and Nano Science,Ewha Womans University,Seoul 03760,South Korea
Hansaem Jeong,Miri Kim,Seung Jin Lee,Hyukjin Lee,College of Pharmacy,Graduate School of Pharmaceutical Sciences,Ewha Womans University,Seoul 03760,South Korea
Soo Yeon Jung,Han Su Kim,Department of Otorhinolaryngology,College of Medicine,Ewha Womans University,Seoul 07985,South Korea
Hae Sang Park,Department of Otorhinolaryngology,College of Medicine,Hallym University,Chuncheon 24252,South Korea
Kyung-Ha Ryu,Department of Pediatrics,College of Medicine,Ewha Womans University,Seoul 07985,South Korea
Abstract
Key words:Stem cell; Tonsil-derived stem cell; Differentiation; Endoderm; Mesoderm;Ectoderm; Cell therapy
INTRODUCTION
Recent achievements in the identification,isolation,in vitroculture,and differentiation of various adult stem cells are indicative of the unprecedented potential of these cells in treating various degenerative diseases[1].Mesenchymal stem cells (MSCs) in particular,have been used clinically for more than 10 years.From animal studies to clinical trials,MSCs have demonstrated great promise in treating numerous diseases,particularly tissue injury and immune disorders[2].To obtain the large volumes of cells required for testing and treatment,various tissue sources have been investigated for the isolation of MSCs,including bone marrow,adipose tissue,umbilical cord blood,amniotic fluid,the placenta,dental pulp,and urine[3].However,the isolation yields of MSCs from different tissue sources vary greatly,and the differentiation potential,yield,and maximal lifespan of isolated MSCs decrease significantly with donor age.Therefore,it is important to locate new adult stem cell sources to overcome these limitations.
The human tonsils are located near the oropharynx (palatine tonsils) and nasopharynx (adenoid),which are part of the respiratory and digestive system.Tonsil tissue is one of the primary sensitization systems for the generation of B cells,and tonsil tissue is easily obtained from tonsillectomies,a minimally invasive surgery conducted most often on patients aged between 5 and 19.Tonsil-derived stem cells (TSCs) were first introduced by Janjaninet al[4].Due to the younger donors,the isolation yields of T-SCs are much higher than those from other tissue types.Therefore,T-SCs have received much attention as alternative allogeneic or autologous cell sources for clinical use.In this review,we highlight recent research on the isolation and development of T-SCs,which provides strong evidence of their superior characteristics.In addition to their high proliferation and expansion capacity,T-SCs can undergo differentiation into cells from all three germ layers (i.e.,ectoderm,mesoderm,and endoderm).This unique differentiation potential is described in detail.Finally,we provide an in-depth discussion of the use of T-SCs in cell therapy and regenerative medicine.
ISOLATING AND IDENTIFYING TONSIL-DERIVED MSCS
Isolating T-SCs consists of two major steps:Enzymatic disaggregation and density gradient centrifugation[5].Briefly,small pieces of tonsillar tissues were exposed to enzymes,including collagenase type I and DNase for 30 min at 37 °C under stirring.This solution was then filtered through a wire mesh and 70-µm cell strainer to collect single-cell suspensions.The mononuclear cell (MNC) fraction was obtained using Ficoll-Paque (GE Healthcare,Little Chalfont,United Kingdom) density gradient centrifugation.The MNCs were plated at the density of 108cells in a T-150 culture flask with Dulbecco's modified Eagle's medium-high glucose (DMEM-HG;Invitrogen) supplemented with fetal bovine serum and antibiotics.The primary culture (passage 0; P0) was cultivated until the adherent cells reached confluence and were passaged by trypsinization (Trypsin,Life Technologies GmbH,Vienna,Austria).
Immunophenotype characterization,which is based on the expression of cell surface markers,is the most common method for distinguishing different cell clusters.To date,extensive research has identified various cell surface markers that characterize the MSCs derived from different sources.In order to identify T-SCs as a cellular source for new adult MSCs,T-SC surface makers were investigated[5,6].As with other MSCs,T-SCs expressed the standard positive markers for MSCs,CD73,CD90,CD105,CD29,CD44,CD166,CD58,and CD49e.Most of these markers represent cellular adhesion molecules which possibly render MSCs to act on other cell typesviadirect interaction.On the other hand,T-SCs were negative for the hematopoietic markers CD14,CD34,CD45,and CD133,the endothelial marker CD31,and co-stimulatory proteins such as the antigens CD40,CD80,and CD86.In addition,class II MHC antigens are entirely absent on T-SCs[5,6].Because tonsil tissue is part of the mucosal immune system and contains large numbers of follicular dendritic cells(FDCs),additional research has been carried out to verify the lack of FDC markers CD11b,CD21,CD23,CD35,and CD54 in T-SCs[5,7]to confirm no-contamination with FDC.FDCs are known to originate from tonsillar stromata and proliferate on and adhere to plasticin vitro.Therefore,the lack of these markers is an important indicator that can be used to distinguish T-SCs from FDCs.
MAJOR ADVANTAGES OF T-SCS OVER BONE MARROWDERIVED STEM CELLS
Although MSCs can be isolated from various tissue types,they were initially harvested from bone marrow (BM),which requires a highly invasive procedure[4].Here,we highlight the significant benefits of using T-SCs in terms of isolation and clinical use compared with BM-MSCs.
Isolating BM-MSCs has several limitations,including donor morbidity,and they are challenging to harvest,thus requiring a high degree of skill.Bone marrow extraction takes approximately two hours under general anesthesia and requires the hospitalization and recovery of the donor.Therefore,it is always difficult to find a sufficient number of donors.In contrast,T-SCs are easily obtained from discarded tissue; more than 530000 tonsillectomies are performed annually in children younger than 15 years in the United States[8],meaning that tonsils are one of the most abundant tissue sources for stem cell isolation.
The age of the donor affects the isolation yield of MSCs,with the number of MSCs harvested from bone marrow decreasing with donor age.For example,infants have one colony forming units-fibroblast (CFU-f) per 10000 cells in bone marrow,but this falls to 1 per 400000 in donors in their 50 s[9].In contrast,approximately 8-10 × 108MSCs are isolated from one-third of one tonsil (2 cm x 1.5 cm x 1.5 cm) from donors under 10 years old[5].
When compared with BM-MSCs,T-SCs offer superior stem cell properties,such as high self-renewal and proliferation.For example,T-SCs show a doubling time of 37.1± 3.4 h for an initial population,compared to 58.2 ± 2.3 h for BM-MSCs[4].Other research has also confirmed the more rapid proliferation of T-SCs compared with MSCs derived from adipose tissue[10].
The proliferation of BM-MSCs gradually decreases with passage number,whereas T-SCs retain their physiological properties for much longer.In general,most cells become more prominent,longer,less defined,and less proliferative during long-termin vitroculture as they experience senescence.T-SCs also exhibit the signs of senescence from passage 7,but the cells proliferate up to passage 15 with no change in the MSC markers.Tonsil tissue contains as many B cells and T cells as immune organs,and these cells affect the immune modulation of stem cells.Pro-inflammatory cytokines may also affect the positive differentiation and proliferation of T-SCs[4,11,12],and this has been supported by research on tissue obtained from tonsillectomies in response to chronic bacterial infections and chronic tonsillitis[13-15].
Bone marrow and adipose tissue originate from the mesoderm layer,whereas tonsil tissue has two origins:The epithelial cells derive from the second pharyngeal pouch in the endoderm layer,and lymphoid tissue comes from the mesoderm layer,which invades during fetal development.Research has confirmed that T-SCs can be easily differentiated into endodermal,ectodermal,and mesodermal cells (Figure 1).
THERAPEUTIC POTENTIAL OF T-SCS BASED ON THEIR DIFFERENTIATION PROPERTIES
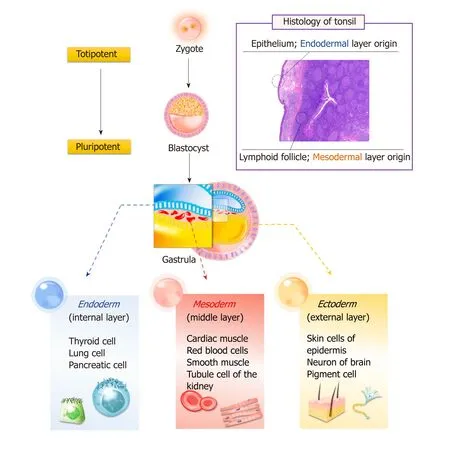
Figure1 Possible reason enables diversity in tonsil-derived stem cells differentiation; constitutive features of tonsil.
Cell therapy and tissue engineering have been investigated to regenerate lost or malfunctioning organs.These approaches utilize biomaterial scaffolds and MSCs to facilitate initial cell adhesion and retention while promoting cell growth for tissue regeneration[16,17].In particular,the differentiation properties of MSCs are of great importance for tissue regeneration.It is generally known that isolated MSCs are often limited to germ-layer specific differentiation.As mentioned earlier,T-SCs offer multipotent differentiation potential that can be applied in regenerating various tissue types without concern for their germ layer origin.
ECTODERMAL DIFFERENTIATION OF T-SCS
Ectodermal differentiation is often difficult to achieve with MSCs isolated from bone marrow and adipose tissue.However,under the right conditions,T-SCs can be differentiated into non-mesenchymal lineages,including ectodermal differentiation into neurons,astrocytes,and Schwann-like cells to support nerve regeneration.
Neuronal differentiation of T-SCs

Figure2 Differentiation potential of tonsil-derived stem cells.
The neuronal differentiation of T-SCs was investigated in a three dimensional (3D)hybrid scaffold system by Patelet al[18].This scaffold was fabricated by increasing the temperature of an aqueous solution of poly (ethylene glycol)-poly(L-alanine) to 37 °C,thus instigating the heat-induced sol-to-gel transition,in which T-SCs and growth factor-releasing microspheres were suspended.The gel exhibited a modulus of 800 Pa at 37 °C,similarly to that of brain tissue,and was robust enough to hold the microspheres and cells within the 3D cell culture.Neuronal growth factors were released over 12-18 d,and the encapsulated T-SCs gradually exhibited morphological changes from spherical to multipolar elongation.Significantly higher expression levels of neuronal biomarkers such as nuclear receptor-related protein,neuronspecific enolase,microtubule-associated protein-2,neurofilament-M,and glial fibrillary acidic protein were observed at both the mRNA and protein level in the hybrid system.This study clearly demonstrates the advantages of 3D hybrid scaffolds and highlights the importance of the sustained release of growth factors from hybrid systems to support the neuronal differentiation of T-SCs.
Schwann cell differentiation of T-SCs
Schwann cells are the glial cells of peripheral nerves that wrap around the axons to form myelin in the peripheral nervous system.Schwann cells promote nerve regeneration by secreting trophic support molecules and establishing a supportive growth matrix[19].Junget al[20]demonstrated that T-SCs could be differentiated into Schwann-like cells over several steps.Briefly,T-SCs were induced to form neurospheres under stimulation with EGF,bFGF,and B27 for 7 d.These neurospheres were then triturated and re-plated onto laminin-coated dishes with Schwann cell differentiation medium.After 10 d of culturing,the cells exhibited morphological changes,including the formation of elongated bipolar and tripolar spindle shapes.Schwann-like cells differentiated from T-SCs highly express the Schwann cell markers GFAP,NGFR,S100B,KROX20,and KROX24.Notably,Schwann cells differentiated from T-SCs were able to produce myelinate axonsin vitrowhen co-cultured with mouse dorsal root ganglion neurons.In a mouse model with a sciatic nerve injury,a marked improvement in gait and increased nerve regeneration were observed with Schwann-cell treatment.Therefore,T-SCs can be a useful source for Schwann cellbased cell therapy to treat neuropathic diseases.
MESODERMAL DIFFERENTIATION OF T-SCS
Mesodermal differentiation is mainly achieved with adult MSCs from the mesodermal germ layer.Previously,a variety of cell sources from bone marrow and adipose tissue was utilized for mesodermal differentiation to treat bone,cartilage,and fat disorders.In this section,we highlight the potential use of T-SCs as an alternative cell source for mesodermal differentiation (Figure 2),and we provide a comparative study that illustrates the advantages of T-SCs.
Osteogenic differentiation of T-SCs
For osteogenic differentiation,Choiet al[21]cultured T-SCs in commercially available osteogenic media (α MEM supplemented with 10% FBS,0.1 mmol/L dexamethasone,10 μmol/L β glycerophosphate,and 50 μg/mL ascorbic acid) for three weeks.Alizarin Red S staining confirmed the successful deposition of extracellular calcium in culture.During osteogenic differentiation,mRNA expression of osteocalcin decreased 0.28-fold after cryopreservation,whereas ALP expression showed no difference.This profile remained stable even after passage 15 (P15).Interestingly,the osteogenic differentiation of T-SCs increased with the number of passages,with the peak osteogenic potential observed for passage 10 (P10),which exhibited a 1.4-fold increase over P3[6].The expression of CCN1,a gene that is closely related to the osteogenic differentiation of MSCs,increased at P10.This finding is consistent with previous studies that have reported that CCN1 expression modulates the osteogenic potential of MSCs by regulating the Wnt3A pathway[6,22].
Various scaffolds have been employed to enhance skeletal regeneration to replace damaged bone.Because bone tissue is highly vascularized,integration with the host tissue followed by subsequent angiogenesis is critical for successful treatment.As an example,Parket al[23]encapsulated T-SCs within highly water-swollen hydrogel through the sol-gel transition of the thermoresponsive polymer poly(ethylene glycol)-poly(L-alanine-co-L-phenyl alanine) (PEG-PAF).The encapsulated T-SCs were culturedin vitroin the presence of an osteogenic-induction medium.The osteogenic differentiation of T-SCs was investigated by evaluating the expression of osteogenic genes,including Runx 2,ALP,and OCN.With support from the hydrogel,osteogenic gene expression was two times higher than that of conventional tissue cultures without soluble factor supplements.
Incorporating specific functional groups into scaffold substrates is also known to affect the osteogenic differentiation of MSCs[24,25].T-SCs were encapsulated in poly(ethylene glycol)-poly(L-alanine) diblock copolymer (PEG-L-PA) thermogel that was modified with the phosphate functional groups of polystyrene microspheres to facilitate the osteogenic differentiation of encapsulated MSCs.The osteogenic differentiation of tonsil-MSCs (T-MSCs) was analyzed,and all osteogenic biomarker expressions were significantly higher for the modified thermogel than for the native thermogel.Immunofluorescence staining also confirmed high OCN expression,and Kyeet al[24]also found that,compared with thermogel modified with carboxylate group microspheres,the phosphate functional group (-PO43-) more readily induced the osteogenic differentiation of T-SCs.
The osteogenic differentiation of T-SCs can be further improved by the overexpression of BMP-2 through genetic material transfer.In Jeonget al[26],BMP-2 minicircle DNA vectors were employed to form nano-sized polyplexes with the CBA-106 polymer.CBA-106 is a bioreducible cationic poly (amido amine) that facilitates the intracellular delivery of genetic material.The osteogenic differentiation of T-SCs was investigated by evaluating the gene expression of osteogenic markers such as osteocalcin,Runx2,and Col 1.In vitrocalcium deposition was also confirmed using Alizarin Red S staining on day 7 and day 14 of the cell culture.In addition,in vivobone regeneration was attempted using T-SCs transfected with the BMP-2 gene.The T-SCs were 3D cultured using PLLA/PLGA scaffolds for one week and then transplanted into the skulls of immunodeficient mice.It was shown that bone regeneration increased 1.96-fold compared to the control group five weeks after treatment.
Chondrogenic differentiation of T-SCs
To mimic a cartilage-like microenvironment,T-SCs were encapsulated in thermogel consisting of the PEG-PAF block copolymer by Parket al[23].Under specific medium conditions (25 μL chondrogenic supplement/2.5 mL basal medium),the much higher expression of Col II and sulfated glycosaminoglycan in T-SCs was achieved using the thermogel than using a monolayer culture.Moreover,unique branching was observed among the encapsulated cells within the hydrogel.These changes in cellular morphology may influence the chondrogenic differentiation of T-SCs during 3D culturing.In vivostudies also confirmed that T-SCs successfully undergo chondrogenic differentiation with high expression levels of biomarkers such as Col II,AGG,and Col X.
Kyeet al[24]also investigated the chondrogenic differentiation of T-SCs within PEGL-PA thermogel.To enhance the cellular attachment in the 3D hydrogel microenvironment,various polystyrene microspheres with thiol (-SH),phosphate (-PO3¬),carboxylate (-COO) and amino (-NH2) functional groups were incorporated into the thermogel.Of the incorporated microparticles,the PS-S,PS-P,and PS-C microspheres exhibited significantly higher COL II expression.COL II mRNA expression was much higher in the PS-S thermogel than in the PS-N thermogel even though the PS-S and the PS-N microspheres had similar sizes,clearly indicating that surface functional groups play an important role in stem cell differentiation.
Similarly,graphene oxide (GO) and reduced graphene oxide (rGO) were incorporated into PEG-L-PA thermogel by Parket al[27]to enhance surface functionality and thus provide good cellular adhesion.GO,or rGO (1 wt%) was suspended in a PEG- L-PA solution.T-SCs in GO/PEG-L-PA or rGO/PEG-L-PA were cultured in DMEM,and the spherical cellular morphology of the T-SCs was observed.When chondrogenic culture media enriched with TGF-β3 was utilized,T-SCs in hybrid systems aggregated extensively,and the expression levels of chondrogenic biomarkers such as SOX 9,COL II A1,COL II,and COL X increased.In particularly,COL II mRNA expression was 13 times higher in the GO/PEG-L-PA hybrid system than in the PEG-L-PA 3D system.Immunofluorescence analysis also revealed a significant increase in COL II expression and cell aggregation in the GO/PEG-L-PA hybrid system.In particular,the GO/PEG-L-PA 2D/3D hybrid system demonstrated the most significant increase in chondrogenic biomarker expression.These results indicate that the cooperative interaction among TGF-β3,COL II,and GO may be closely related to signaling cascades for chondrogenic differentiation.
Adipogenic differentiation of T-SCs
Ryuet al[5]investigated T-SCs as a source for adipogenic differentiation due to their multi-lineage differentiation potential and self-renewal capacity by culturing them using commercially available adipogenic media (Gibco StemPro™ Adipogenesis Differentiation Kit,Thermo Fisher Scientific,Waltham,MA,USA) for three weeks.The adipogenic potential of the T-SCs was evaluated for P3,P7,P10,and P15.Interestingly,unlike other types of T-SC differentiation,the adipogenesis of T-SCs decreased continuously with passage number,with P10 approximately two-thirds that of P3.
Adipogenic differentiation of T-SCs in thermogel was also investigated using PEGL-PA (molecular weight of each block:1000-1080 Da) by Kyeet al[24].The differentiation potential of T-SCs was investigated by incorporating polystyrene microspheres with different functional groups into the hydrogel.mRNA expression and immune histochemical assays indicated that T-SCs preferentially underwent adipogenesis in ammonium (-NH3+)- or thiol (-SH)-functionalized thermogels,whereas chondrogenesis occurred predominantly in phosphate (PO32-)- or carboxylate (-COO-)-functionalized thermogels.This study thus suggests that the surface functional groups of microspheres can control the preferential differentiation of stem cells into specific cell types in 3D cultures.
In addition to functionalized hydrogels,Patelet al[28]reported that a composite system of GO and polypeptide thermogel (GO/P),prepared using the temperaturesensitive sol-to-gel transition of GO-suspended poly(ethylene glycol)-poly(L-alanine)(PEG-PA),significantly enhanced the expression of adipogenic biomarkers,including PPAR-γ,CEBP-α,LPL,AP2,ELOVL3,and HSL when compared with a native hydrogel system.It appears that insulin,an adipogenic differentiation factor,can preferentially adhere to the surface of the GO incorporated into thermogels; insulin is then slowly released into the environment in a sustained manner during the cell culturing period.In contrast,more hydrophobic graphene may interfere with insulin,causing partial denaturation,reducing the adipogenic differentiation of T-SCs.
Myogenic differentiation of T-SCs
Various MSCs and progenitor cells have been evaluated their differentiation capacity into the myogenic cells for skeletal muscle regeneration.MSCs derived from BM,adipose,and umbilical cord tissue,and their use in cell therapy to augment the skeletal muscle injury response,have also been reported[29-31].An alternative cellular source for MSCs,T-SCs have been shown to differentiate into myogenic cellsin vitro,and transplanting the myoblasts and myocytes generated from T-SCs mediates the recovery of muscle function following injuryin vivo[32].For myogenic differentiation,T-SCs are treated in three sequential steps:Sphere formation on a petri dish in lowglucose DMEM,rosette-like spread formation on a collagen-coated dish,and two weeks of myogenic induction.In this final step,the cells express myogenic markers,including desmin,dystrophin,MHC,skeletal markers,α-Actinin,TNNI1,and myogenin.Furthermore,the intramuscular injection of T-MSC-derived myogenic cells into myectomized C57BL/6 mice enhances muscle function as demonstrated by gait assessment and the restoration of the skeletal muscle structure.
ENDODERMAL DIFFERENTIATION OF T-SCS
The endodermal differentiation of MSCs is important because many degenerative diseases are related to organs that originate from the endoderm,including the liver,pancreas,and parathyroid.In this section,we highlight recent research that employs T-SCs to produce functional hepatocytes,pancreatic beta cells,and parathyroid cells(Figure 2).
Hepatocyte differentiation of T-SCs
Many clinical studies have indicated that BM-MSCs are safe and effective in the treatment of liver disease[33].They can alleviate end-stage liver disease and improve symptoms and liver function[34,35].However,some studies have indicated that BMMSCs have the potential to aggravate fibrosis[36-38].Thus,employing BM-MSCs as a therapy for liver fibrosis remains controversial.
As a novel cell source for treating liver disease,Parket al[39]demonstrated that TSCs differentiate into hepatocyte-like cells and ameliorate live fibrosisviathe activation of autophagy and the downregulation of TGF-β.A three-week culture in a differentiation medium containing IGF,HGF,dexamethasone,and oncostatin M led to the development of hepatocyte-like cells from T-SCs,as revealed by the expression of albumin and HNF-4α.In addition,transplanting T-SCs into a carbon tetrachloride(CCl4)-induced liver injury mouse model confirmed that T-SCs have a regenerative effect by migrating to the site of the liver injury and differentiating into hepatocytelike cells.These results prove that T-SCs was able to differentiate into hepatocyte-like cells bothin vitroandin vivo.
In addition to the direct differentiation of T-SCs into liver hepatocytes,T-SCs have also been investigated in terms of hepatogenic differentiation using PEG-L-PA thermogel[40,41].The thermogel exhibited a physical modulus of 1000 Pa,which is similar to that of decellularized liver tissue.Three different 3D culture systems were compared in relation to the use of soluble factors such as hepatogenic growth factors.The spherical morphology and size of the encapsulated cells were maintained in the native 3D culture system during a culture period of 28 d,whereas the cells changed their morphology and aggregated significantly in 3D systems with growth factors.Hepatocyte-specific biomarker expression and metabolic functions were negligible in the native culture system.However,the expression levels of the hepatogenic genes of albumin and cytokeratin 18 and hepatocyte nuclear factor 4α were high in the two systems supplemented with growth factors.In addition,albumin and α-fetoprotein production were also significant[40].PEG-L-PA thermogel thus provides a biocompatible microenvironment for the hepatogenic differentiation of T-SCs.In particular,the successful results of the growth factor encapsulated hydrogel system suggest that PEG-L-PA thermogel is a promising injectable tissue engineering system for liver tissue regeneration[41].
Pancreatic differentiation of T-SCs
Metabolic disturbances associated with diabetes lead to a number of complications ranging from cardiovascular and cerebrovascular disease to neuropathy,retinopathy,nephropathy,and the poor healing of wounds[42].The only curative therapy available is pancreatic islet cell replacement,for which suitable donors are rare and which requires immunosuppressant therapy to reduce rejection.Recently,stem cell therapy has been proposed for the treatment of diabetes.Transplanting insulin-secreting cells produced from various stem cells,including embryonic and induced pluripotent stem cells and MSCs has shown therapeutic effects in diabetic animals[43].In addition,differentiating various MSCs,including BM-MSCs and adipose MSCs,into insulinproducing cells has been suggested[44].Kimet al[10]investigated the efficiency of differentiating T-SCs into insulin-producing cells by comparing two different methods and found that T-SCs differentiated more efficiently with insulin-transferrinselenium (ITS) than with β-mercaptoethanol.The ITS method is composed of three steps:Two days of culturing in high-glucose α-MEM with 1% fatty acid-free bovine serum albumin (BSA) and 1 × ITS on a nonadherent dish; four days of culturing in high glucose α-MEM with 1% fatty acid-free BSA,ITS,3 mM taurine,and 10 mM nicotinamide; and four days of culturing in high-glucose α-MEM with 1% fatty acidfree BSA,ITS,3 mmol/L taurine,10 mmol/L nicotinamide,100 nmol/L glucagon-like peptide,and 10 Nm exendin-4.Notably,T-SCs exhibited a differentiation capability that was superior to that of adipose cell-derived MSCs.Further,implanting T-MSCderived insulin-producing cells significantly alleviated streptozotocin-induced glucose intolerance in mice.These results suggest that T-SCs have the potential to be reprogrammed into pancreatic β-cells and applied to the clinical treatment of diabetes in the future.
Parathyroid differentiation of T-SCs
Hypoparathyroidism is a rare endocrine disorder,resulting in low serum calcium and increased serum phosphorus[45].Hypoparathyroidism is the only hormonal insufficiency state that does not have a hormone-replacement-therapy approved.Current managements include supplementation with oral calcium and active vitamin D,which cause various life-long adverse effects[45].
Stem cells have shown some promise in treating hypoparathyroidism in clinical applications.It has been reported that human embryonic stem cells (hESCs) and differentiated thymic stromal cells can be used in thein vitroregeneration of parathyroid-like cells[46-48].However,the use of hESCs have critical ethical limitations,and it takes over 10 weeks for thymic stromal cells to differentiate and secrete PTH.Because of this,T-SCs have been considered as an alternative cell source for cell therapy.Parket al[49]demonstrated that T-SCs differentiate into parathyroid-like cells that release intact PTH using the modified Bingham protocol.Briefly,T-SCs at 90%confluence were cultured in a differentiation medium containing activin A and soluble sonic hedgehog for 7-21 d.Surprisingly,the T-SC-derived parathyroid-like cells differentially secreted PTH in response to extracellular calcium levels.Further,the therapeutic effects of T-SC-derived parathyroid-like cells embedded in Matrigel in rats that have undergone a parathyroidectomy suggest that embedding differentiated T-SCs in hydrogel scaffolds is a promising strategy for restoring parathyroid function.
ROLE OF T-SCS AS A NATIVE CELL THERAPY SOURCE
In addition to their multipotent differentiation potential,stem cells hold great promise for the treatment of numbers of diseases,especially those related to tissue damage involving immune reactions.The therapeutic effects of MSCs depend largely on their capacity to regulate inflammation and tissue homeostasisviaan array of immunosuppressive factors,cytokines,growth factors,and differentiation factors[50].Interestingly,depending on their type and intensity,inflammatory stimuli can lead MSCs to suppress the immune response in some cases or to enhance it in others.This plasticity of MSCs in immunomodulation leads them to act as suppressors or enhancers in response to the microenvironment[51].In particular,the palatine tonsil is secondary lymphoid tissue that continuously encounters antigens and subsequently drives efficient immune response[52].This tissue specificity may account for the intrinsic property of T-SCs in terms of immune regulatory plasticity.
IMMUNE MODULATION BY T-SCS
Previously,T-SCs have shown excellent immunomodulatory properties in targeting muscular fibrosis[53],skin inflammation[54],B-cell-mediated immune response[55],and autoimmune-mediated colitis[56].In addition,T-SCs have been shown to improve the immune system by facilitating myelopoiesis in an allogeneic BMT mouse model[57].These studies report that non-differentiated,non-stimulated native T-SCs constitutively secrete anti-inflammatory cytokines such as IL-1Ra,PD-L1,and EBI3 protein.Conditioned media from T-SCs that contain high levels of IL-1Ra efficiently regulate the mediation of the pro-fibrogenic process of myotubes by altering their IL-1β activity.Similarly,PD-L1 is a well-known immune-suppressive protein that targets numbers of immune and nonimmune cells.Notably,T-SCs express both soluble and membrane-bound forms of PD-L1 at higher levels compared with BM-MSCs and ATMSCs.Indeed,T-MSC-derived PD-L1 has been demonstrated to attenuate Th17cellmediated skin inflammation in psoriatic skin dermatitis in mice.
Recent studies have reported that IL-35 is a regulatory protein that acts on B cells[58]and that T-SCs constitutively produce EBI3,which is a critical component of IL-35[55].Of note,T-SCs significantly ameliorate the estrogen-induced B-cell response bothin vitroandin vivoin an IL-35-dependent manner.
Allogeneic hematopoietic stem cell transplantation is a routine treatment for intractable hematologic malignancies.The co-transplantation of BM-derived MSCs and donor HSCs promotes hematopoietic cell engraftment and prevents graft-versushost disease with accelerated marrow stromal regeneration[59,60].Research has also found enhanced myelocytic or megakaryocytic engraftment in the co-transplantation of MSCs and HSCs.Ryuet al[57]reported the supporting role of T-SCs in BM reconstitution and in supplementing hematopoiesis in a BMT mouse model.Considering that hematopoietic cells give rise to all of the mature blood cell types,including immune cells,normalizing hematopoiesis may eventually reverse immune deficiency induced by Bu/Cy preconditioning.Parket al[39]reported another study that demonstrated immune activation by T-SCs.In CCl4-induced liver fibrosis in mice,T-SCs migrated directly to injured tissue in the liver and promoted the restoration of liver function.Furthermore,T-SCs have been shown to promote the activation of autophagy,which ultimately resolved fibrotic processes[39].These results indicate that T-SCs can have a dual function on immunity by either activating or inhibiting the immune system.
FUTURE PERSPECTIVES OF T-SCS IN REGENERATIVE MEDICINE
The mass production of stem cells is vital for their widespread use,but,unfortunately,this process is expensive and time-consuming.Therefore,the regular use of stem cells as therapeutic agents lies in the distant future.However,T-SCs present new possibilities for the clinical application of stem cells.Obtaining T-SCs is more costeffective than obtaining other types of stem cell; for example,tonsil tissue is readily obtained from tonsillectomies without the need for additional procedures.The yields and doubling times of T-SCs are also better than those for other stem cell types,and TSCs from multiple donors can be used together[5].The differential potential of T-SCs is also very cost-effective for clinical applications.For example,it takes only 14 d for tonsil tissue to differentiate and secrete PTH,whereas it takes over 10 weeks when thymic cells are employed[32].T-SCs can also differentiate into various tissue types from all three germ layers.These features suggest that T-SCs can be a new cell source for regenerative medicine.
SHORTCOMINGS TO OVERCOME FOR CLINICAL USE
T-SCs have yet to be fully characterized.Tonsils are composed of various tissue types and cells (e.g.,connective tissue,endothelium,epithelium,and lymphocytes),which presents both advantages and disadvantages.As summarized above,T-SCs show promise for differentiation,and this is thought to be due to the various components of T-SCs and to the generally younger age of the donors.However,the histological diversity of T-SCs can be an obstacle to clinical applications because of the risk of tumorigenesis.Further,it possibly made variations of the T-SCs capacities,e.g.,differentiation into certain cell types.Therefore,the thorough characterization,including molecular mechanisms that facilitating differentiation of T-SCs should precede any clinical trials.
CONCLUSION
Tonsil tissue is a promising alternative source for the high-yield isolation of adult stem cells.Although T-SCs exhibit a cellular morphology and surface markers that are similar to those of bone marrow-derived MSCs,T-SCs possess superior stem cell properties that are very useful for various applications in regenerative medicine.Unlike other adult stem cell sources,T-SCs are typically isolated from young donors under age of 10.This is particularly beneficial in that tonsillectomies provide not only with a source of abundant tissue but also with good proliferation and differentiation potential of isolated T-SCs.In particular,isolated T-SCs exhibit multi-lineage differentiation,which is not often observed in other sources.As a result,it is clearly that T-SCs hold great promise for clinical applications in cell therapy and regenerative medicine.
 World Journal of Stem Cells2019年8期
World Journal of Stem Cells2019年8期
- World Journal of Stem Cells的其它文章
- Moving forward on the pathway of cell-based therapies in ischemic heart disease and heart failure - time for new recommendations?
- Neural regeneration by regionally induced stem cells within poststroke brains:Novel therapy perspectives for stroke patients
- Orchestrating stem cell fate:Novel tools for regenerative medicine
- Bone marrow microenvironment:The guardian of leukemia stem cells
- Linking stemness with colorectal cancer initiation,progression,and therapy
- Derivation and applications of human hepatocyte-like cells
