Retroperitoneal hematoma following common iliac artery injury in a child
Aditya Badheka , Madhuradhar Chegondi
1 Division of Critical Care Medicine, Stead Family Children’s Hospital, Iowa City, IA 52242, USA
2 Department of Pediatrics, Carver College of Medicine, University of Iowa, Iowa City, IA 52242, USA
Dear editor,
A six-month-old child with a history of coarctation of aorta repair admitted to our hospital with recoarctation.She underwent cardiac catheterization for stent placement via right femoral access. Reportedly, there was difficulty inserting and removing the sheath. There was no bleeding or hematoma and the distal pulse well felt at the completion of the procedure. While in recovery unit child acutely deteriorated with tachycardia, oxygen desaturation,and hypotension. She was then endotracheally intubated and started on fluid resuscitation and on vasopressors infusion. Upon arrival to the pediatric intensive care unit(PICU) child was tachycardic, pale and noted a mass on the right lower quadrant of the abdomen. Her hemoglobin dropped from 12 gm/dL to 5 gm/dL. Given the child with hemorrhagic shock, and with right lower quadrant abdominal mass, a possibility of retroperitoneal hematoma(RPH) was considered. Other possible causes of hemorrhagic shock, such as vascular access site bleeding,pleural and pericardial effusions were ruled out.
Upon further workup, X-ray imaging with the aortic stent was in place with left side displaced urinary bladder noted (Figure 1). Abdominal ultrasonogram was suggestive of retroperitoneal hematoma (RPH). A bedside angiogram through the left femoral access demonstrated no active bleeding and complete occlusion of the right common iliac artery (CIA) (Figure 2). She received several blood product transfusions with the resolution of shock. Since the child’s hemodynamics improved, she was managed conservatively and extubated to room air following day.Her right lower extremity had mild capillary refill delay.Heparin infusion was started initially then transitioned to low molecular weight heparin before discharging home. At one month follow up child’s right lower extremity perfusion normalized.
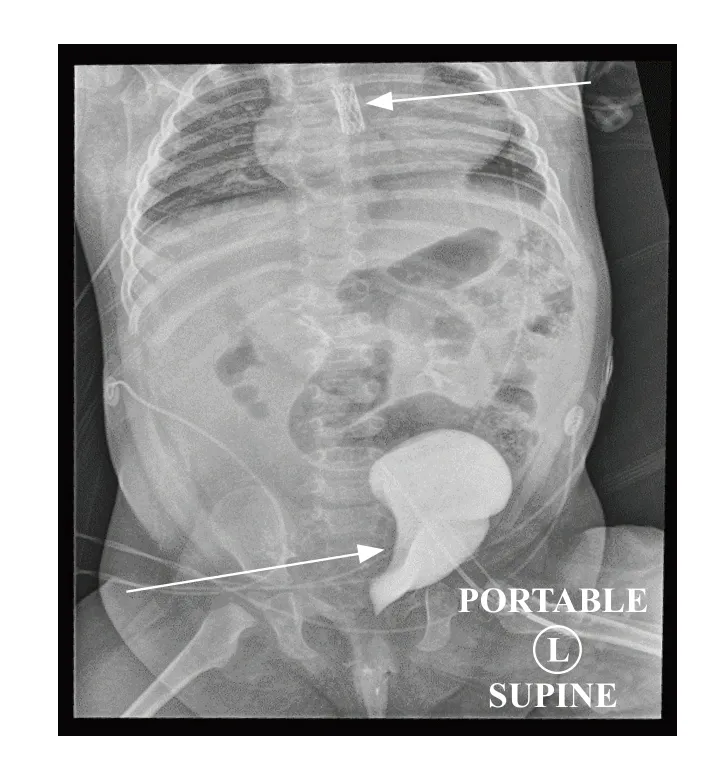
Figure 1. X-ray imaging with the aortic stent was in place with left side displaced urinary bladder noted.
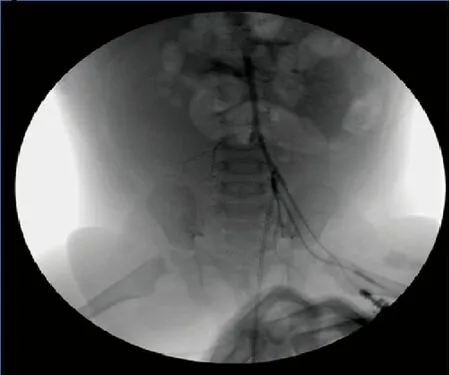
Figure 2. A bedside angiogram through the left femoral access demonstrated no active bleeding and complete occlusion of the right common iliac artery.
DISCUSSION
Although the complications associated with cardiac catheterization declining, vascular complications are still the most common adverse event.[1]The occurrence of retroperitoneal hemorrhage (RPH) following iliac artery injury is rare but it’s potentially fatal.[2,3]The risk of complications was higher in patients with less than 6 months of age, inpatient status, and with interventional procedures.[1,3]Since retroperitoneum can accommodate a large volume of blood volume, patients usually present with hypovolemic shock, lower abdominal mass, as in our index child. Computed tomography(CT) of the abdomen confirms the diagnosis of RPH.[2]Early recognition of RPH and aggressive resuscitation will improve the outcome.[4]In patients with unstable hemodynamics and with active bleeding, endovascular or open surgery is recommended.[5]
Funding: None.
Ethics approval: Not needed.
Competing interests:The authors have no conf lict of interest, no f inancial issues to disclose.
Contribution: All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work;drafting the work or revising it critically for important intellectual content; and f inal approval of the version to be published.
 World journal of emergency medicine2019年3期
World journal of emergency medicine2019年3期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Benef its of using an endotracheal tube introducer as an adjunct to a Macintosh laryngoscope for endotracheal intubation performed by inexperienced doctors during mechanical CPR: A randomized prospective crossover study
- Are radiological modalities really necessary for the long-term follow-up of patients having blunt solid organ injuries? A single center study
- A comparison of simulation versus didactics for teaching ultrasound to Swiss medical students
- Prioritization of factors related to mental health of women during an earthquake: A qualitative study
- Clinical characteristics of patients with Haff disease after eating crayf ish
