Benef its of using an endotracheal tube introducer as an adjunct to a Macintosh laryngoscope for endotracheal intubation performed by inexperienced doctors during mechanical CPR: A randomized prospective crossover study
Hüseyin Cahit Halhalli, Asım Enes Özbek, Emrah Çelİk, Yavuz Yİğİt, Serkan Yilmaz, Müge Çardak
Department of Emergency Medicine, University of Health Sciences, Kocaeli Derince Training and Research Hospital,Kocaeli, Turkey
Dear editor,
Out-of-hospital cardiac arrest survival rates vary between 7% and 46% and are lower than those for inhospital cardiac arrests (IHCA).[1,2]Therefore, efforts are being made to increase survival rates for out-ofhospital cardiac arrests (OHCA). According to advanced cardiac life support (ACLS) guidelines, out-of-hospital cardiac arrest survival rates may be increased by performing cardiopulmonary resuscitation (CPR) with minimal interruptions.[3]According to the latest ACLS,does the patient need an advanced airway? If yes, use the airway that is appropriate to your skill level: King Airway System™, LMA, Combitube™, or endotracheal intubation. However, endotracheal intubation together with continuous CPR will be the basis of a permanent and safe airline management to prevent risk of aspiration,and in respiratory-induced OHCA administration as well as IHCA during long-term procedures such as percutaneous transluminal coronary angioplasty (PTCA).[3]
There are no differences in the survival rates of manual versus mechanical CPR. However, mechanical CPR devices can be used in appropriate situations, such as performing CPR in an ambulance in motion, in cases where quality CPR is diff icult to perform, or in cases with operator limitations.[4]An endotracheal tube introducer(ETI) is an effective, inexpensive, and easy-to-use tool for opening airways[5]in adult patients with a Cormack-Lehane score of 3.[6]Endotracheal intubation using an ETI can be learned quickly with brief instructions.[7]In adult patients, there is no study evaluating the experience of ETI during Lucas with CPR.
The study is to compare the f irst-attempt success rates of inexperienced doctors in an ambulance simulation for endotracheal intubation performed on mannequins with a Macintosh laryngoscope (ML) with or without an ETI while performing CPR using a continuous mechanical CPR device.
METHODS
This study was designed as a randomized prospective crossover ambulance simulation study utilizing mannequins. It was approved by the ethics committee of Kocaeli University (GOKAEK-2017/16.15). The study was registered with ClinicalTrials. gov, and all of the doctors volunteering signed informed consent before participating in the study.
This study was conducted between January and February 2018 and included 40 inexperienced doctors who had just started their professional careers within the province of Kocaeli in the Emergency Department of Derince Training and Research Hospital. Junior doctors underwent a routine 8-hour training module,during which an emergency medicine specialist instructed them about theoretical and practical airway training. The instructor was blinded to the study in order to eliminate any possible bias. The doctors were informed about the study following this instruction.Those who volunteered to participate were enrolled in the study after providing written informed consent. The participating doctors received a general briefing about the study but were blinded to its specific purposes. The doctors were allowed to practice on the mannequin for 5 minutes, either alone or with advice from the emergency specialist, as requested.
This study was performed using a Life/form®Deluxe Crisis™ Mannequin Torso with advanced airway management. As airway interventions in an ambulance are performed in a sitting position, the height of the stretcher was adjusted to the height of an ambulance stretcher. The participating doctors were requested to perform all of the interventions while sitting in a chair that was the same height from the f loor as an ambulance seat. A number 8 cuffed endotracheal tube was used for intubation. First,the endotracheal tube and mannequin airway were lubed with pump-spray lubricant provided with the simulator.The airway mannequin was positioned supine. In order to achieve CPR standardization and to eliminate possible bias caused by the doctor performing CPR during interventions, CPR was performed using an automated CPR device (Lund University Cardiac Arrest Systemversion 2 [LUCAS 2TM], 100 chest compressions per minute with 5 cm compression depth). All airway devices were placed at the mannequin’s side.
In order to minimize the effects of learning, this study was conducted as a randomized crossover study.For randomization, cards of equal sizes were labeled with the number 1 or 2, with an equal number of cards for each number. All of the cards were identically folded in half and placed in a brown opaque envelope. All of the envelopes were placed in a box. After the training module, each participating doctor was requested to pick an envelope from the box. Those who picked the card labeled with number 1 initially performed the endotracheal intubation using a laryngoscope with a number 3 ML blade, while those who picked a card labeled with number 2 initially performed the intubation using an 8 Fr Muallem ETT Stylet (METTS) (VBM Medizintechnik GmbH; Sulz am Neckar, Germany)ETI as an adjunct to a laryngoscope with a numner 3 ML blade (ETI+ML). After completing these initial interventions, those who picked number 1 performed their second intubation using the ETI+ML, while those who picked number 2 performed their second intubation with the ML alone.
Each doctor was given 1 minute to complete a successful intubation.[8]In both groups, the doctors were allowed a second attempt if the first failed. The intubation time began when the doctor initially handled the laryngoscope and ended when the mannequin was ventilated with a bag-valve mask. The presence of upand-down movement in the mannequin’s chest with ventilation was accepted as a successful intubation. All procedures were recorded on a camera placed inside the room, of which all the doctors were aware. First-attempt success rates, intubation times, and number of attempts were recorded.
Following the intubations, the doctors were requested to evaluate the difficulty levels of both methods on a 5-point Likert scale (1: very easy, 2: easy, 3: moderate,4: difficult, and 5: very difficult). Additionally, the doctors were questioned as to whether they had any prior experience using an ML with or without an ETI, and their replies were recorded.
The study’s primary outcome measure was defined as the success rate of the first intubation attempt. The secondary outcome measures were defined as the intubation times, number of intubation attempts, and the difficulty level of the methods as defined by the Likert scale.
For an intubation time of 20 seconds, a 5-second difference was accepted as significant. Accepting an α error probability as 0.05 and a β error probability as 0.2,the sample size for each group was calculated as 23.Kaplan Meier test was used to evaluate the mean tracheal intubation times between the ETI+ML and ML groups.McNemar’s test was used to compare the success rates between the ETI+ML and ML groups.
RESULTS
Initially, 43 doctors were supposed to be included in this study, but since 3 did not provide written consent,the study was conducted with 40 doctors (Figure 1).Endotracheal intubation with the ETI+ML was more successful than endotracheal intubation with the ML.The overall intubation success rate was 96% (38/40) with the ETI+ML and 75% (30/40) with the ML (P=0.021).The first-attempt success rate for tracheal intubation was higher with the ETI+ML (77.5%, 31/40) than with the ML alone (65%, 26/40), but this difference was not signif icant (Table 1). While 17.5% (7/40) of participants using the ETI+ML were successful during the second attempt, this rate was 10% (4/40) for those using the ML alone.
However, the average successful intubation time was longer with the ETI+ML (28 seconds 95% CI 25.8-30.2 seconds) than with the ML alone (24 seconds 95% CI 20.4-27.6 seconds), but this difference was not statistically signif icant (P=0.637) (Figure 2).
The study participants generally reported that the ETI made intubation easier. While 77.5% (31/40) of the respondents rated the use of the ETI+ML as easy or very easy, only 40% (16/40) of the respondents rated the use of the ML alone as easy or very easy. However, only 5%(2/40) of the respondents rated the use of the ETI+ML as diff icult, while this rate was 22.5% (9/40) for the use of the ML alone (P=0.001).
DISCUSSION
Users with ETI have achieved a high first pass success within an acceptable average time. Respondents stated that the ETI provided convenience when performing endotracheal intubation and that intubation with the ML alone was more difficult compared to intubation using the ETI as an adjunct. However, the use of an ETI led to prolonged endotracheal intubation times.
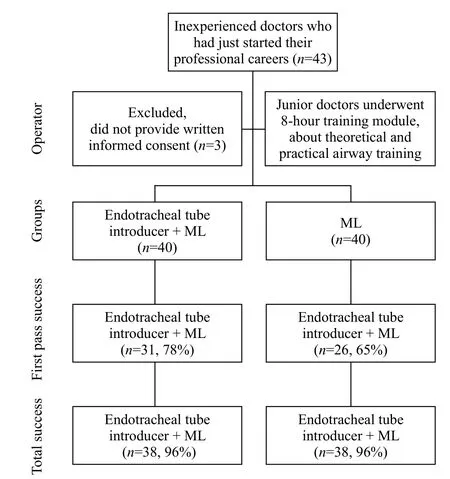
Figure 1. Patients f low.
Unexpected airway problems may occur in emergency departments or outside the hospital.Performing endotracheal intubation during chest compressions can be difficult, as every compression results in vibrations in the glottis.[9]Therefore, the ETI provides great aid during difficult airway interventions performed in emergency departments or out of the hospital.[7,10]The participants performing intubation in the present study were inexperienced doctors who used an ETI for the f irst time. It has been reported that tracheal intubation success rates during chest compressions are especially low among inexperienced doctors.[11]We hypothesize that the second-attempt success rates in the current study were significantly higher than the firstattempt success rates because the doctors were gaining more experience. These results suggest that, as clinicians gain experience, their first-attempt success rates for endotracheal intubation with an ETI should increase.
Although this study’s participants had no prior experience with an ETI, successful intubation rates were higher with the use of an ETI for the second attempt,suggesting that better first-attempt success rates may be obtained in comparison to classical methods as the doctors gain more experience using an ETI.
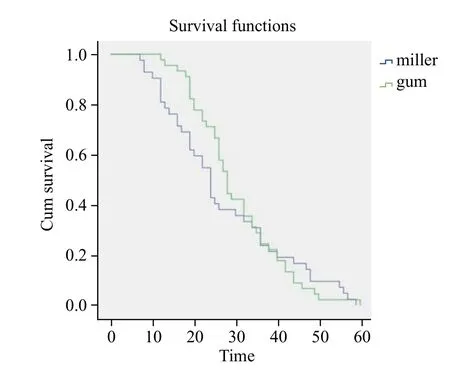
Figure 2. Kaplan Meier analysis of time to success rate.
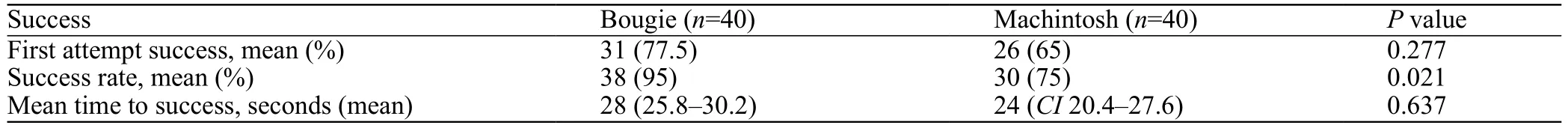
Table 1. Successful intubation rates and times
Advanced life support guidelines emphasize the importance of uninterrupted chest compressions during cardiopulmonary resuscitation.[12]According to the guidelines, these interruptions, which adversely affect coronary and cerebral blood flow and venous return,should not exceed 5 seconds. Nonetheless, 25% of the time elapsed without applying chest compressions in an out-of-hospital CPR setting is spent performing tracheal intubation interventions. It has been reported that some out-of-hospital intubation interventions exceed 3 minutes.[13]Prolonged interruptions in resuscitation have serious adverse effects on survival, and successful endotracheal intubation rates in out-of-hospital ambulance settings are low.[13]Therefore, increasing the first-attempt success rate is key to preventing complications. Results of the current study indicate that success rates increase as operators gain experience using an ETI and that the use of an ETI results in greater success rates. Therefore, the use of an ETI is expected to reduce complications caused by interruptions in chest compressions.
Results of the current study reveal longer than average intubation times when an ETI was used for endotracheal intubation. This is in accordance with previous studies.[14]However, the total intubation times in both groups were longer than those previously reported.[15]This may be due to operator inexperience, ongoing chest compressions making intubation more difficult, or position restraints of operators in the ambulance simulation. Prolonged intubation times can lead to complications, such as hypoxia, aspiration, hypotension, and arrhythmia.[16]Nevertheless, shorter times have been reported with more experienced operators.[17]
In the present study, participants indicated that performing endotracheal intubation with an ETI was easier than using a Macintosh laryngoscope alone. An ETI has a smaller diameter than the endotracheal tubes,and the anteriorly angled tip makes it easier to guide and advance through the glottis.[15]This may explain why the participants indicated that using an ETI was more convenient.
Limitations
The current study has some limitations. First,this study was conducted using a mannequin. The actual airway in a living patient may present various complicating factors, including blood, vomit, a foreign body, and airway edema. Moreover, the stress associated with living patients cannot be reproduced with simulation mannequins. However, our study utilized an ambulance simulation and continuous chest compressions to mimic the clinical setting as closely as possible. Second, in comparison to living patients, airway interventions take longer when performed on simulation mannequins.[18]This may also have affected our results. Third, the short instruction period may have had adverse effects on the results of both groups. Last, in our study we asked the practitioners a single question and asked whether it was easy or difficult to implement. This is not an adequate satisfaction survey. Therefore, we could not calculate the reliability of this single-question survey.
CONCLUSION
Results of the current study indicate that the use of an ETI as an adjunct for intubation did not provide signif icant improvements in the success rates of the f irst intubation attempts during CPR with a mechanical CPR device in an ambulance simulation. However, after the first attempt, the use of an ETI facilitated endotracheal intubation. Nevertheless, further randomized controlled prospective studies are needed to compare the use of an ETI and ML in an actual out-of-hospital ambulance setting.
Funding:None.
Ethical approval:The study was approved by the ethics committee of Kocaeli University (GOKAEK-2017/16.15).
Conf licts of interest:Authors have no f inancial or other conf licts of interest related to this submission.
Contributors:HCH and AEÖ conceived the study, designed the trial, and obtained research funding. HCH, EÇ, MÇ and AEÖ supervised the conduct of the trial and data collection. HCH, YY,EÇ and AEÖ undertook recruitment of participating centers and patients and managed the data, including quality control. YY and SY provided statistical advice on study design and analyzed the data; HCH chaired the data oversight committee. AEÖ drafted the manuscript, and all authors contributed substantially to its revision.HCH takes responsibility for the paper as a whole.
 World journal of emergency medicine2019年3期
World journal of emergency medicine2019年3期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Retroperitoneal hematoma following common iliac artery injury in a child
- Are radiological modalities really necessary for the long-term follow-up of patients having blunt solid organ injuries? A single center study
- A comparison of simulation versus didactics for teaching ultrasound to Swiss medical students
- Prioritization of factors related to mental health of women during an earthquake: A qualitative study
- Clinical characteristics of patients with Haff disease after eating crayf ish
