Are radiological modalities really necessary for the long-term follow-up of patients having blunt solid organ injuries? A single center study
Mehmet Ilhan, Recep Erçin Sönmez, Abdullah Kut, Safa Toprak, Ali Fuat Kaan Gök, Mustafa Kayıhan Günay,Cemalettin Ertekin
1 Department of General Surgery, İstanbul University İstanbul Medical Faculty, İstanbul, Turkey 2 Department of General Surgery, İstanbul Medeniyet University, İstanbul, Turkey
Dear editor,
During the past two decades, management of blunt solid organ injuries had shifted from conventional surgery to more conservative approach, namely nonoperative management (NOM).[1]The non-operative approach mainly depends on the trauma experience of surgeons and the institution, quality of radiographic imaging and its interpretation.[2-5]If the surgeon decides to observe the patients by NOM, close monitoring of vital signs and frequent physical examinations must be done accordingly with radiological evaluations if needed.
Since the first application of computed tomography(CT) for blunt trauma in 1980, progress in technology had let its way for improvements in CT scans.[6,7]By the application of helical scanning together with multidetector CT (MDCT), much more detailed images have become able to be captured through faster scanning periods.[8]
All these modifications give CT a much bigger role in the era of solid organ injuries.[9]MDCT had become the standard choice of modality at the most institutions for the evaluation of abdominal injuries for its highly accurate diagnostic quality and short acquisition time.[10-12]On the contrary, the facts of contrast-induced nephropathy with radiation exposure start the discussions about its liberal usage limiting to certain cases.
A number of large series have attempted to examine the management of blunt solid organ injuries; however,only a few studies regarding management for the long term follow-up after discharge from the hospitals exist.[13]According to our research in recent literature, there is no published work so far with high volume of patient population (considering at least 100 cases) which is focused on the application of CT scanning for the postdischarge evaluation of blunt solid organ injured patients having history of NOM.
In the present study, we wanted to share our institutional experience about the clinical course of patients having blunt solid organ injuries during 1-year follow-up by physical examinations and simple blood tests only, and to give advices for future studies according to our results and clinical observations.
METHODS
From January 2010 through December 2017,patients who were hospitalized in General Surgery Department with the diagnosis of blunt solid organ injury were retrospectively analyzed. Within all, 115 patients who had been evaluated by MDCT scans were included into the study (including the ones under 18 years of age). All the patients were managed nonoperatively during the hospital stay. Having different time intervals of hospital stay, some of them had multivisceral injuries. Exclusion criteria of the study were hemodynamic instability, signs of peritonitis, and need of surgical intervention.
The patient anamnase was achieved from the medical database of the department. Data collection included patient characteristics (gender, age, any known comorbidities, record of physical examination on admission, blood analysis), length of hospital stay,count of MDCT scans during hospitalization and at postdischarge, need of intensive care unit (ICU), morbidity and mortality rates, radiological evaluations and Organ Injury Scale (OIS) scaling system which were assessed for each patient according to severity of organ injury, and evaluation of long-term follow-ups.
A standard management protocol (Eastern Association for the Surgery of Trauma [EAST] in the Practice Management Guidelines)[14]was used and consisted of treating all hemodynamically stable and without signs of peritonitis patients nonoperatively irrespective of injury grade. Hemodynamic stability was assessed using routine vital signs (blood pressure, pulse rate), serum lactate, and base excess measurements.Determination of peritonitis was done according to abdominal examinations done routinely every day throughout the hospitalization period.
All patients who were hemodynamically stable and had no indication for immediate surgery underwent focused abdominal sonography for trauma (FAST)and MDCT scanning of the abdomen and pelvis.Depending on the severity of injury, some of the patients were evaluated by control MDCT scans during the hospitalization and at post-discharge period. Assessments of long-term follow-up had been made according to the findings which were recorded during the 1st, 6thmonths and the 1styear of post-discharge controls.
The images of the patients were saved in our hospital’s “Picture Archiving and Communication System” (PACS), and they were retrospectively reviewed in this sections on axial, coronal, and sagittal planes.Grading of injuries done by the radiologists was assigned according to OIS which is established by American Association for the Surgery of Trauma (AAST).[15,16]
The primary outcomes of the study were long-term clinical observations, general complications and failure of NOM. Secondary outcomes were length of hospital stay, number of readmissions and ICU-stay.A P value less than 0.05 was considered statistically signif icant.
RESULTS
Patient characteristics
A total of 115 patients (M=75 [65,2%] / W=40[34,8%]) with a calculated mean age of 23.53±19.11 years (52 [45.2%] of them under 18 years old), who had sustained blunt solid organ, were admitted for further treatment (Tables 1 and 2). Average length of stay at the hospital was 10.54±12.21 days (1-108). One patient with 108 days of hospital stay had severe associated head injury which caused neurological sequelae, and was referred for home health care after his discharge.The overall mortality rate was 2.6% (n=3). These three patients had high grade multivisceral injuries besides solid organs which necessitated massive blood product transfusions including both erythrocyte suspensions and fresh frozen plasma (FFP). They had become exitus during their ICU follow-up.
Statistical analysis
Student’s t test was used for statistical analysis. All statistical analyses were performed using SPSS statistical package version 23.0 (SPSS Inc., Chicago, IL, USA).
Radiological assessments and in-hospital outcomes
Retrospective evaluation of CT scans revealed liver injury (n=65, 56.5%), splenic injury (n=54, 47%),kidney injury (n=13, 11.3%) and other solid organ injuries def ined as pancreas and/or surrenal (n=15, 13%)in all of the patients involved in the study. According to OIS scaling system which were interpreted by the Radiology Department, 64 patients (55.6%) (average calculated age=25) had severe solid organ injury (OIS score: 3-5). Twenty-seven (42%) of them had a history of ICU admission, with an average of 10 days of stay at the hospital which was the same as the average of total population. Within the group of severely injured according to OIS scaling system, 2 patients having grade 3-4 liver injuries consecutively and 1 patient having grade 4 splenic injury were treated with angioembolization by the radiologists due to vascular contrast extravasation observed on CT scan.
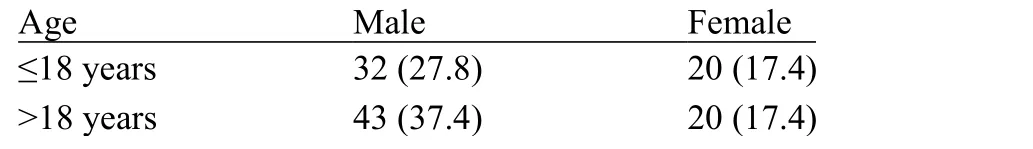
Table 1. Patient distribution according to gender and age, n (%)
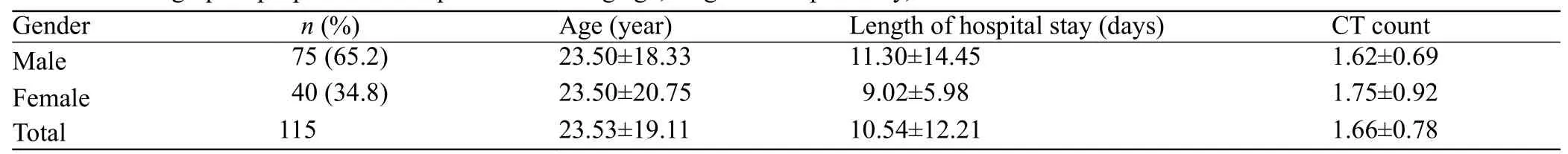
Table 2. Demographic properties of the patients showing age, length of hospital stay, CT count
As all of the patients were evaluated at least by one CT scan before discharge, average count was found as 2 (range=1-5), and 52 patients (45.2%) were evaluated by one CT scan only during hospitalization period and at post-discharge out-patient controls. Within this group,29 patients (55.8%) had been categorized in the severely injured group. Average length of stay in this subgroup was calculated as 11.4 days, and had a mortality rate of 6.9% (n=2).
All of the candidates included in the study were followed-up by NOM despite of severity of organ injury.Forty-three patients (37.4%) required “erythrocye suspension (ES)” transfusion (with an average of 2 transfusions, range=1-19), and “fresh frozen plasma(FFP)” was given to 26 patients (22.6%) (with an average of 1 transfusion, range=1-20).
Long-term evaluations
Patients having blunt solid organ injury with a history of NOM were evaluated during the first, sixth months and at the first year of post-discharge controls by only physical examinations, asking about complaints if any, and with simple blood tests analysis. There was no mortality noted during the post-discharge period eventually. Irregular bowel movements were reported in 15 (13%) patients which were due to constipation mostly and 22 (19%) patients complainded of chronic abdominal pain during their examinations though which were confirmed by plain films and control USG as without pathological f indings. Mean follow-up time of the study was 1 year.
DISCUSSION
There has been great improvement in NOM of abdominal solid organ injury in recent decades. For most of the cases, treatment strategy has shifted from surgical interventions to more conservative approach.[17-19]During the past three decades, multiple studies have shown that NOM of abdominal solid organ injuries is effective, with a success rate of 90%.[20-23]Although a large number of series had attempted to examine the management of blunt solid organ injuries, there are only few studies present based upon the clinical surveillance regarding the long term follow-up after discharge.
In the present study, we focused on the clinical follow-up of blunt solid organ injured patients during post-discharge period. All of the patients came back at the 1st, 6thmonths and the 1styear of post-discharge for control evaluations. Other than mild symptoms like irregular bowel movements and chronic abdominal pain for some, none of the patients had major complaints including severely injured ones.
As mentioned before, substantial amount of severely injured patients (OIS score: 3-5) were included into the study (n=64, 55.6%). There was no statistical difference found when compared with the ones having OIS score less than 3 regarding length of stay at the hospital.Although all of the mortalities occurred in the severely injured group with a percentage of 2.6, all had been reported during the hospitalization period.
Detailed evaluation of the patients with multidisciplinary approach (close follow-up of hemodynamic parameters,routine physical examinations, blood analysis and radiological observations if needed) has utmost importance for NOM during hospitalization and for longterm follow-up. Grading systems like “Injury Severity Score”, and “Radiological Organ Injury Grading System”are helpful tools to decide the type of management, but none of them is above the clinical sense of a clinician.
Radiological evaluation of trauma will keep going to evolve and so the CT scans will be improved as much more multi-sliced images with higher resolutions will be captured. On the other hand, performing control CT scans for every trauma patient is an irrational procedure according to our institutional experience. Besides undesirable side effects like to be a non cost-effective procedure mostly and possible contrast nephropathy,it exposes large number of patients to high doses of radiation.[24-26]Maria et al[27]stayed the problem in a published EAST guidelines in 2003 by indicating that there is no evidence for serial CT scans without clinical indications influenced either the outcome or the management of the patient. Considering the possible side effects of MDCT, ultrasonographic evaluations were preferred for patients involving pediatric population(under age of 18) at f irst sight during control scans unless for need of more detailed examinations. Moreover, it is unnecessary for the evaluation of a patient with control CT scan at post-discharge control independent of severity of injury if she/he has no major physical complaint. Through this approach, undesirable effects of CT can be prevented.
Some limitations exist with the present study. Postdischarge follow-up period is limited considering this type of patients, so delayed presentation of symptoms related to past injuries may have been missed.Although all of the patients included in the study had been evaluated at least by one CT scans, there was no algorithm guiding the decision of which patients underwent for control scans. Also, the patients who had need of surgical intervention were excluded from the study. Their presence in the study can change the interpretation of long-term results.
CONCLUSION
Increasing experience in trauma management throughout the years let the way from only surgical treatments to NOM mostly in present day. Despite of these progressions, the clinicians’ approach towards trauma patients depending on his/her experience has a value above all, other than radiological procedures, blood tests, grading systems etc. For selected patient groups of solid organ injury, post-discharge control CT scans are mostly unnecessary and have low cost-effect rate.Physical examination of an experienced clinician with appropriate blood tests, are mostly enough and accurate to determine the clinical follow-up of the patients.
Funding:This study did not receive any funding.
Ethical approval: The Institutional Review Board approved the study.
Conf licts of interest:Authors declare that they have no conf lict of interest.
Contributors: Mİ, RES, ST: study concept and design; MKG, CE,ST: acquisition, analysis, or interpretation of data; Mİ, AFKG:statistical analysis; Mİ, RES, AK: drafting of the manuscript;RES, AFKG: critical revision of the manuscript for important intellectual content; MKG, CE: study supervision.
 World journal of emergency medicine2019年3期
World journal of emergency medicine2019年3期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Retroperitoneal hematoma following common iliac artery injury in a child
- Benef its of using an endotracheal tube introducer as an adjunct to a Macintosh laryngoscope for endotracheal intubation performed by inexperienced doctors during mechanical CPR: A randomized prospective crossover study
- A comparison of simulation versus didactics for teaching ultrasound to Swiss medical students
- Prioritization of factors related to mental health of women during an earthquake: A qualitative study
- Clinical characteristics of patients with Haff disease after eating crayf ish
