A comparison of simulation versus didactics for teaching ultrasound to Swiss medical students
Sagar Shah, Steven Tohmasi, Emily Frisch, Amanda Anderson, Roy Almog, Shadi Lahham, Roland Bingisser, John C. Fox
1 School of Medicine, University of California, Irvine, USA
2 Department of Emergency Medicine, University of California Irvine, Irvine, USA
3 University Hospital Basel, Basel, Switzerland
KEY WORDS: Ultrasound education; POCUS; Switzerland; Medical education
INTRODUCTION
Point of care ultrasound (POCUS) is an increasingly common diagnostic imaging modality that is used in a variety of clinical settings. Over the past few decades,ultrasound machines have become more affordable,compact, and powerful. POCUS has been shown to offer physicians a rapid form of initial assessment without harmful effects. Several studies have demonstrated the potential for long term clinical skills.[1,2]As the utility and scope of POCUS expands, it is important to ensure that physicians are competent with this technology and have a good understanding of the abilities and limitations of this imaging modality.
Many medical schools have begun integrating ultrasound education into their medical school curriculum.[3,4]Jamniczky et al[5]surveyed 108 medical students from such programs and found that students perceived learning and interpreting ultrasound images to be of “high cognitive load”. The training required to become prof icient in interpreting ultrasound images has,therefore, understandably placed focus on anatomy and structure identif ication. To date, many studies measuring the efficacy of ultrasound education in medical school curriculum have done so in the context of anatomy.[6]While anatomy is important in understanding ultrasound,POCUS machines also produce irremediable artifacts that are as conceptually diff icult to understand as they are diagnostically significant. The interpretation of such an imaging modality leaves signif icant room for user error.
Given the increased utilization of POCUS in the clinical setting, it is important to introduce this skill during medical education. Many programs have attempted to integrate ultrasound into the anatomy portions of their curriculum.[6]However, measures of the efficacy of ultrasound education in anatomy are equivocal.[7]Currently, assessments of the efficacy of ultrasound education in improving competence in physiology is lacking. Furthermore, simulation-based medical education is becoming a highly touted strategy to improve clinical competence and patient safety and is perceived by medical students to be a highly positive educational experience.[7-9]
The objective of this study is to assess the efficacy of a simulation-based ultrasound education curriculum for medical physiology. We hypothesize that pre-clinical medical education is heavily classroom based. Thus,greater emphasis is placed on memorization rather than understanding. By placing students in simulated clinical scenarios and engaging them in ultrasound material, we hypothesize that medical students would retain more ultrasound knowledge, have an improved understanding of the associated physiology of each exam and would perceive the educational content to be of greater value than content taught in the standard didactic style.
METHODS
Study design
We performed a prospective, observational study using a convenience sample of subjects recruited from the University of Basel Medical School in Basel, Switzerland. The study was approved by the Institutional Review Board (IRB) with the support of University of Basel Medical School administration.Each participant provided verbal, informed consent before participating in the study. Study participants were randomly divided into eight cohorts and each cohort was enrolled in a two-day, focused ultrasound course. The study spanned a period of four weeks with two full courses taking place per week.
Study protocol Subject recruitment
Research participants were recruited to participate in a focused ultrasound training course at the University of Basel via internal email correspondence prior to the arrival of the research team. A total of 116 students were approached for enrollment. Among them, 39 were male and 76 were female. One student was unable to complete the second day of the course and was thus excluded from the analysis. The 115 study subjects included medical students from the University of Basel Medical School, University of Zurich Faculty of Medicine,and University of Bern Faculty of Medicine. Medical education in Switzerland consists of six years of training after completion of secondary school and completion of a qualifying examination. Study participants were in various stages of their medical education. All research participants were provided with detailed information regarding the purpose and design of the study. Each research participant voluntarily enrolled in this study and attended the corresponding ultrasound education sessions. Participant privacy was protected by deidentifying all personal information using assigned,study-specif ic codes.
Study site details
The research study took place over a period of 4 weeks in July 2018 at the University of Basel Hospital in Basel, Switzerland. Study participants took part in a two-day focused medical ultrasound course over this time period. Half of the participants were randomly assigned to the didactic ultrasound education group while the other half received simulation-based ultrasound education. Prior to initiation of the ultrasound curriculum, all participants were given two separate precourse examinations to determine baseline ultrasound and physiology competency, respectively. The same examinations were given again as at the conclusion of the teaching course to assess for differences in ultrasound and physiology competency. Education and testing were done in English.
Course instructor preparation
Courses were administered by U.S. based allopathic medical students who had successfully completed their first year of medical education. Participating medical students served as course instructors as part of a student organized international trip to Switzerland taking place in the summer between the f irst and second years of their medical education. All participating medical students satisf ied all mandated requirements to complete the f irstyear medical school curriculum. More specifically, all participating medical students achieved passing grades in human physiology, anatomy, and POCUS. As part of the POCUS curriculum, f irst-year medical students received ten hours of hands-on training in a small group setting.Medical students also were required to view pre-recorded lectures that taught POCUS imaging of various organ systems. First-year medical students received lectures and hands-on training on topics such as ultrasound physics and instrumentation, cardiac, hepatobiliary,renal, pulmonary, vascular, pelvic, and musculoskeletal ultrasound. Students were evaluated with multiple written examinations to assess POCUS competence throughout their first-year of medical school. A final grade of 70% or greater for each system was required to achieve a passing grade in the clinical foundations course.
All participating medical students also underwent an additional 4-hour training to simulate pre-designed clinical vignettes using standardized models. Instructors were trained on the pathognomonic signs and symptoms of particular diseases in order to role-play realistic presentations of a given clinical scenario for students receiving simulation-based ultrasound education. A total of nine unique simulation cases were presented.
Ultrasound curriculum
Study participants were randomly divided into eight cohorts and each cohort was enrolled in a two-day,focused ultrasound course. All instruction was provided in English. The study spanned a period of four weeks with two 2-day courses taking place per week for a grand total of 8 classes. The focused ultrasound course covered basic ultrasound principles including ultrasound physics and instrumentation, pulmonary ultrasound, abdominal/gastrointestinal ultrasound, cardiac ultrasound, and Focused Assessment with Sonography for Trauma(FAST). The material was presented in PowerPoint format and included diagrammatic, video, pictorial,and textual content centered on spatial orientation,pathology, physiology, and physical concepts. The first day consisted of presentations on basic concepts, the abdominal exam, and the pulmonary exam. The second day consisted of cardiac and FAST scans. Following each 30-minute presentation, one hour was allotted for small group hands-on training with the presented materials.For the hands-on portions, scans were performed using the following portable ultrasound units: Konted C9 Plus, Hitachi Aloka Noblus, and Hitachi EUB-5500. All students became proficient in using the phased array,curvilinear, and linear transducers. Following the two presentations and the two hands-on sessions, the didactic group (control group) received additional didactic ultrasound instruction for 1 hour while the simulation group (experimental group) received case-based simulation instruction for 1 hour.
The didactic group was allowed to move between several stations, each manned by an instructor. The students were given the freedom to practice any scans covered during the day. As students practiced various scans, instructors were to review associated physiology concepts. The instructors covered the same concepts underlying the case-based instruction that the simulation group was receiving. The simulation group rotated through several stations at which pairs of instructors acted out a clinical scenario. One instructor acted as the patient while the other moderated the scenario, providing necessary clinical details and interjecting when necessary to ask questions or provide instruction. The moderator reviewed associated physiology as the cases unfolded.Students developed a short differential at which point they were allowed to perform whichever ultrasound exam they saw f it. Instructors then showed videos of pathophysiological ultrasound findings to bring the case to a close. Instructors rotated weekly between didactic and simulation groups to minimize bias due to instructor variation.
Assessment
Prior to the course, a 20-question multiple-choice physiology exam was given along with a 30-question multiple-choice ultrasound competency exam. At the conclusion of the focused ultrasound course, the same two examinations were again administered to evaluate each participants’ mastery of ultrasound and physiology(Figures 1 and 2). Additionally, participants were asked to rate their comfort level of using ultrasound in their future medical practice and to rate the perceived value of course content on a scale of 1 (lowest) to 5 (highest).The question asked students to respond to the statement“I would feel comfortable using ultrasound in my future practice of medicine”. A response of 1 meant they “strongly disagreed”, a response of 2 meant they“disagreed”, a response of 3 meant they felt “neutral”,a response of 4 meant they “agreed”, a response of 5 meant they “strongly agreed”. Subjects were graded with a composite of their performance on the f inal ultrasound and physiology examinations. A cumulative grade of 65% qualified as a “pass”. Any score of 64% or lower was considered a “fail”.
Data collection and statistics
We collected data from the pre-course examination,post-course examination, demographic survey, and perceived value content survey. Data was analyzed separately for the control and experimental groups.Pre- and post-course examination scores of both groups were then compared using a student’s t-test. A P-value of <0.05 was used to determine statistically significant improvement in the mastery of physiology and/or ultrasound between the control and experimental group.All t-tests were two-tailed and assumed non-equal variances between groups.
RESULTS
A total of 115 participants were included in the study. The year in medical school of participants ranged from year 1 to year 6. About 33.9% of participants were male and 66.1% of participants were female (Table 1).Fifty-five participants were randomized to the didactic(DID) group and 60 participants were randomized to the simulation (SIM) group. One participant was unable to complete the ultrasound course in its entirety, and was excluded from the statistical analysis.
Following randomization, the average year in medical school was 2.28 for the SIM group and 2.50 for the DID group (P>0.05). The mean pre-course ultrasound exam score was 39.5% for the SIM group (n=60) and 41.6% for the DID group (n=55) (P>0.05). The mean pre-course physiology exam score was 54.1% for the SIM group and 59.30% for the DID group (P>0.05).When asked to subjectively assess individual comfort with ultrasound techniques, the average response was 2.7 out of 5 for the SIM group and 2.5 out of 5 for the DID group (P>0.05). These results demonstrate that prior to the ultrasound course, there were no statistically significant differences in level of education, knowledge of physiology or ultrasound, or familiarity with ultrasound machines between SIM and DID groups.
Following the two-day course, all students werere-administered the same ultrasound and physiology exams. All participants of the simulation group and of the didactic group achieved passing grades on both examinations. The simulation group showed statistically signif icant improvement on the physiology exam, going from a pre-test average of 54.12% to a post-test average of 75.32% (P<0.01). The didactic group also showed statistically significant improvement on the physiology exam, going from a pre-test average of 59.30% to a posttest average of 70.00% (P<0.01). These improvements correspond to an average improvement of +21.20%and +10.70% for the SIM and DID group respectively.T he magnitude of improvement of the SIM group was signif icantly greater than that of the DID group (P<0.01).The simulation group demonstrated statistically significant improvement on the ultrasound exam, going from a pre-test average of 39.5% to a post-test average of 71.6% (P<0.01). The didactic group also showed significant improvement on the ultrasound exam, going from a pre-test average of 41.6% to a post-test average of 71.52%. H owever, for the ultrasound exam, there was no statistically significant difference in the magnitude of these improvements (P>0.05). At the completion of the course, all participants were asked to assess the validity of the following statement on a scale from 1 to 5:“The material covered in this course was of value to my medical education”. The average response was 4.1 for the SIM group and 4.0 for the DID group. This was not statistically signif icant.
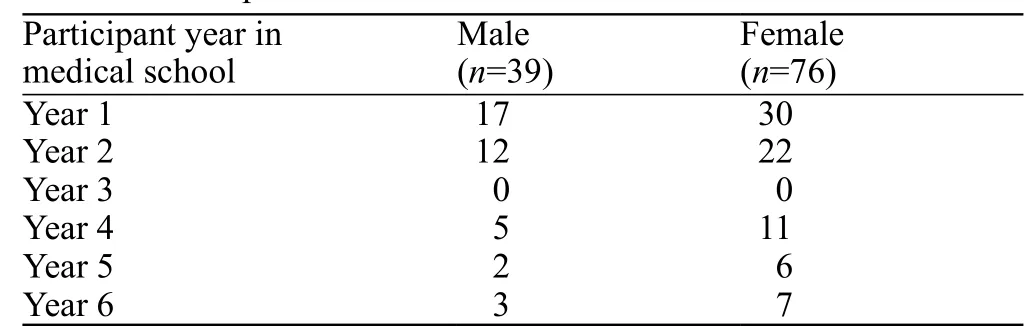
Table 1. Participants in ultrasound course
DISCUSSION
Our study aimed to assess the eff icacy of simulationbased ultrasound instruction in improving medical student mastery of physiology and ultrasound concepts.The specific goals of the two-day course included mastery of the abdominal/gastrointestinal, pulmonary,cardiac, and FAST ultrasound exams and underlying physiological concepts. Both the didactic and simulation groups had passing exam averages in physiology and ultrasound following the two-day ultrasound course.Additionally, both groups showed statistically signif icant improvement following the course, suggesting that either teaching style was suff icient to convey the basic concepts of ultrasound and associated physiology. However,our data indicates students taught in the context of simulated clinical vignettes improved their physiology scores more than students taught with standard didactics(+21.20% and +10.70% respectively). However, there was no statistically signif icant difference in magnitude of improvement on the ultrasound exam, suggesting there was no concurrent trade-off in retention of information of ultrasound mechanics due to time spent performing simulations. Because our instructors were trained to deliver the same teaching points during the didactic training sessions that were being covered during the simulated clinical vignettes, we were able to minimize the differences in the total content that didactic and simulation groups received. Therefore,our results suggest that the context provided by the clinical vignettes allows for greater understanding and retention of such physiology content. Alternatively, the simulation-based teaching may simply keep students more engaged and interested in the material, thereby improving retention.
As ultrasound is expanding into an increasing variety of clinical settings, the integration of ultrasound education into medical school curriculum has become quite prevalent.[10-12]A survey conducted in 2014 suggested that medical school curricular administrators were ambivalent in regards to placement of ultrasound education within medical school anatomy courses.[13]Our results, in conjunction with prior studies, suggest that medical students may benef it from ultrasound taught in the context of physiology.[7]Placing too much focus on anatomy may yield diminishing returns given an experienced ultrasound user can become sufficiently familiar with standard exam images without a detailed understanding of associated anatomy. Placing a focus on anatomical structure can make it difficult to capitalize on the integrative nature of ultrasound. In the context of physiology, instructors can cover structures while also discussing pathology and clinical manifestations, thereby merging content from several different medical courses.To date, no other study has looked at the relative value of case-based simulation in ultrasound education compared to didactic instruction. Our results demonstrate both noninferiority in improving ultrasound knowledge, as well as superiority in bolstering mastery of associated physiology.
As medical schools experiment with different methods of integration of ultrasound education into their curricula, modalities of education that promote student engagement should be valued, given there exists a significant body of research demonstrating that the passive role students play in lecture-based learning contributes to poor learning outcomes.[14,15]Our results suggest that simulation-based ultrasound education is of great subjective value to students. Especially in programs that divide medical education into “preclinical” and “clinical” years, simulated ultrasound scenarios provide younger students the opportunity to apply their knowledge in an environment that most resembles the clinical setting. Integrating ultrasound through case-based simulation may be helpful to improve understanding and retention of POCUS.
Limitations and future research
There are several limitations to our study. All data was collected from a single education system utilizing a convenience sample of Swiss medical students. It is unclear if these results are generalizable to American or other international medical students.Furthermore, our relatively small sample size also limits the generalizability of conclusions drawn from our research. Additionally, our study did not longitudinally assess competence and we cannot comment on how well simulation-based ultrasound education or didacticbased education promotes long-term retention. We did not systematically assess the physical skills and techniques of the ultrasound exam. Additional studies will be required to determine the ability of POCUS to be taught using didactics and simulation. Competence in these skills may or may not be completely independent from improved understanding of underlying ultrasound concepts. Lastly, the pre-test and post-test were the same examination. Future studies may consider using different examinations to test ultrasound knowledge retention.
Future large-scale studies are needed to validate our data and further explore the efficacy of simulationbased POCUS education. In particular, a large-scale,longitudinal study that assesses long-term retention of ultrasound and associated physiology following case-based simulation sessions could benefit medical educators tasked with designing an eff icient and effective medical school curriculum.
CONCLUSIONS
Our data suggests that simulation-based POCUS training for Swiss medical students resulted in statistically significant improvement on physiology examination.However, there was no difference in ultrasound knowledge improvement between the simulation-based and didactic-based groups. Future, large-scale studies are needed to validate this promising data.
ACKNOWLEDGMENTS
UC Irvine Health Department of Emergency Medicine, UC Irvine School of Medicine.
Funding:None.
Ethical approval:The study was approved by the Institutional Review Board (IRB) with the support of University of Basel Medical School administration.
Conflicts of interest:Dr. J Christian Fox receives stock options from Sonosim for consulting. However, no Sonosim products were used in this research project.
Contributors:SS, EF, AA, RA proposed the study and prepared the f irst draft. All authors read and approved the f inal version of the paper.
Received December 9, 2018 Accepted after revision April 16, 2019
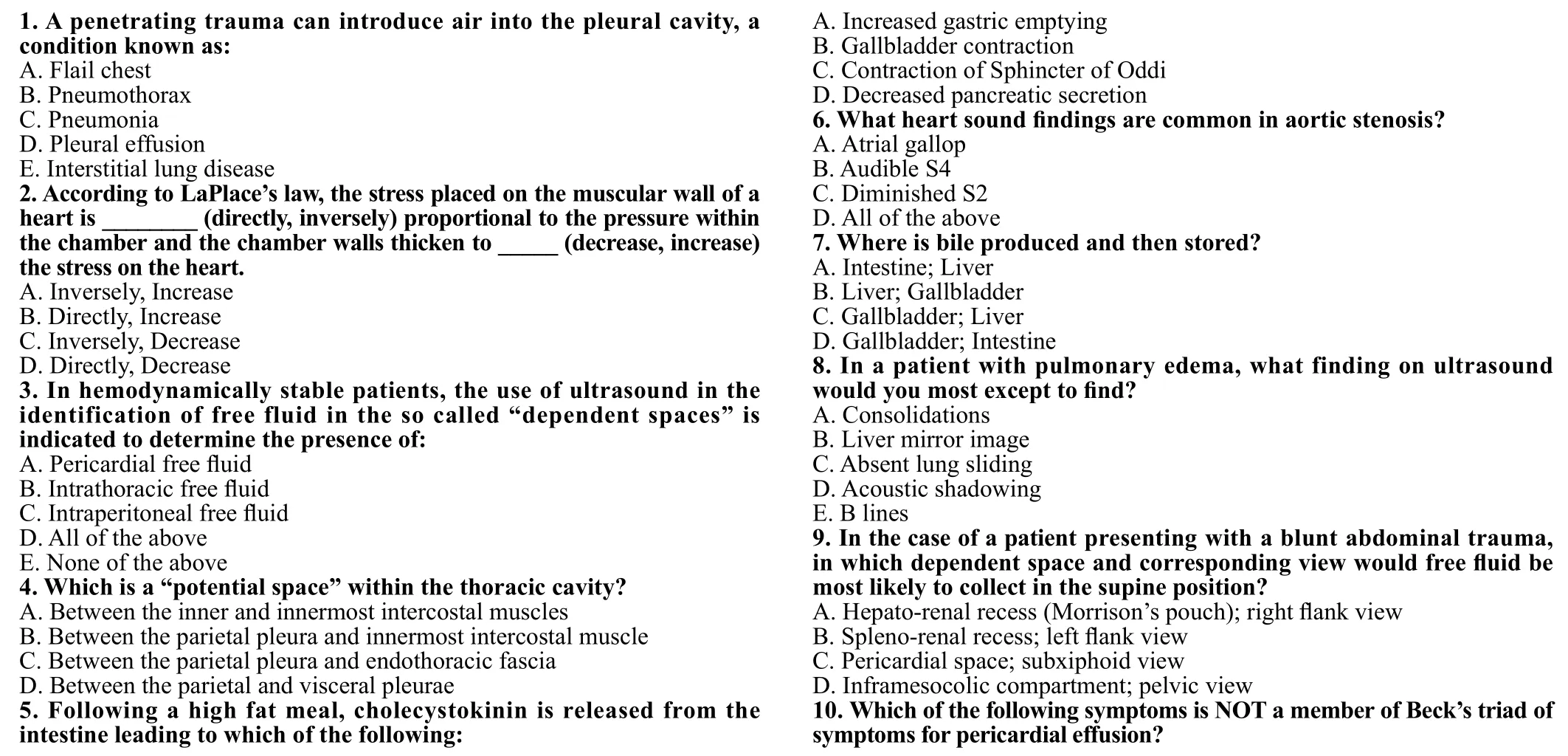
Physiology Written Exam Summer 2018
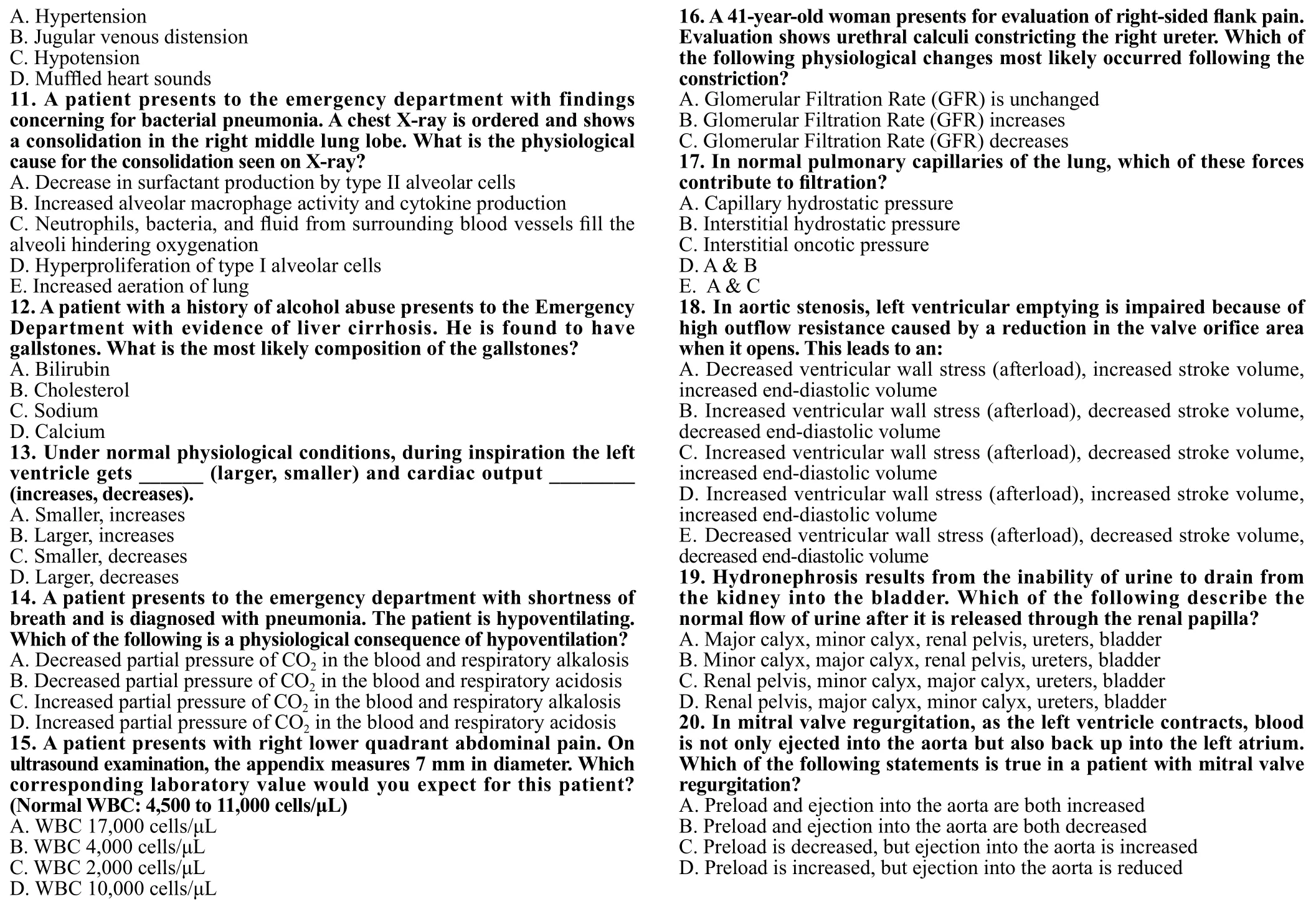
Figure 1. Physiology exam.
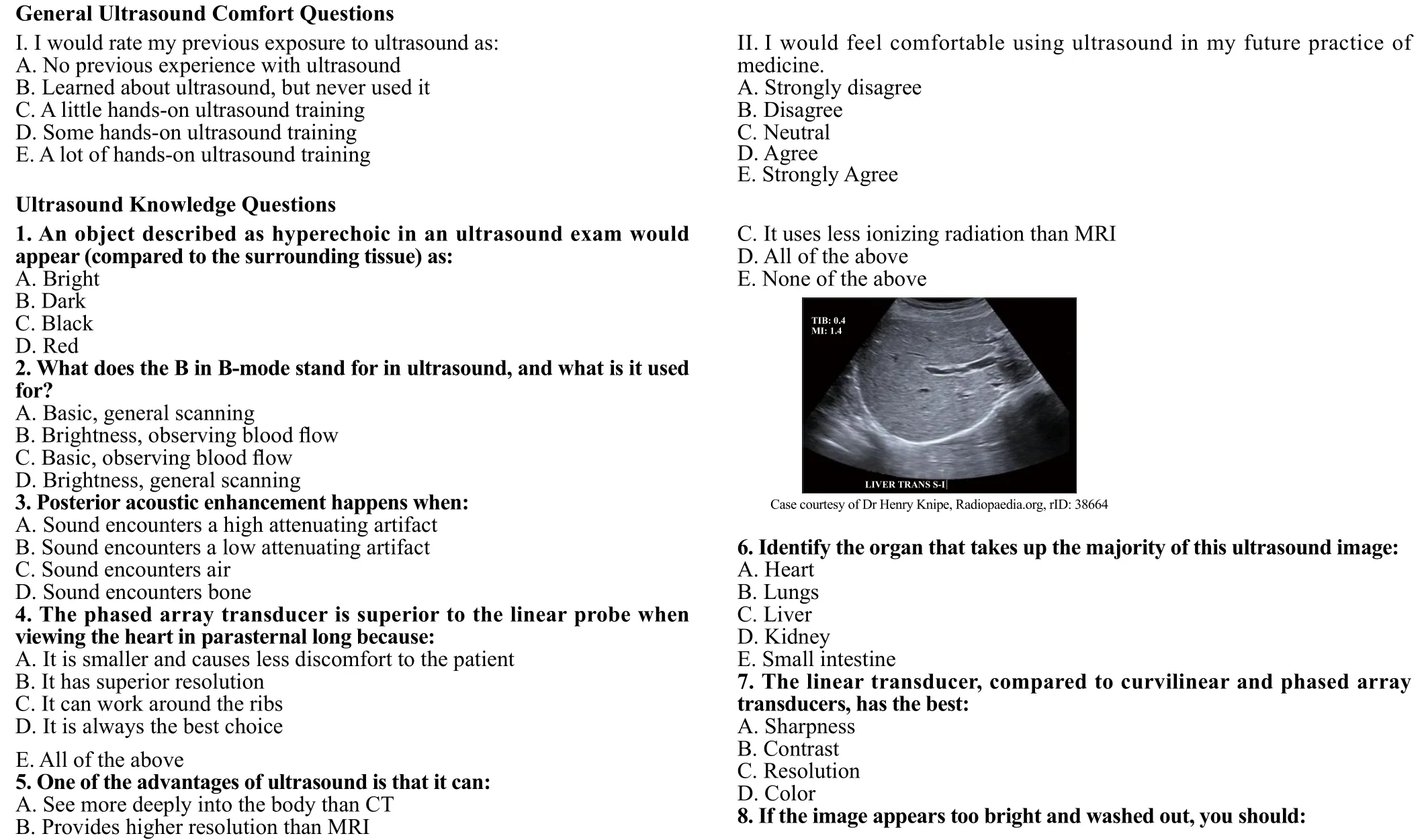

Figure 2. Ultrasound Written Exam.
 World journal of emergency medicine2019年3期
World journal of emergency medicine2019年3期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Retroperitoneal hematoma following common iliac artery injury in a child
- Benef its of using an endotracheal tube introducer as an adjunct to a Macintosh laryngoscope for endotracheal intubation performed by inexperienced doctors during mechanical CPR: A randomized prospective crossover study
- Are radiological modalities really necessary for the long-term follow-up of patients having blunt solid organ injuries? A single center study
- Prioritization of factors related to mental health of women during an earthquake: A qualitative study
- Clinical characteristics of patients with Haff disease after eating crayf ish
