Clinical characteristics of patients with Haff disease after eating crayf ish
Cai-jun Wu, Hai-jiang Zhou, Wei Gu
1 Department of Emergency Medicine, Dongzhimen Hospital, Institute of Sepsis, Beijing University of Chinese Medicine,Beijing 100700, China
2 Department of Emergency Medicine, Beijing Chao-yang Hospital, Capital Medical University, Beijing, China
3 Emergency Medicine Center, Chuiyangliu Hospital Aff iliated to Tsinghua University, Beijing, China
KEY WORDS: Haff disease; Rhabdomyolysis; Crayfi sh
INTRODUCTION
Haff disease is a rare syndrome characterized by unexplained myalgia and rhabdomyolysis occurring within 24 hours of consumption of certain types of freshwater f ish or crustacean. Examples of these include buffalo fish, crayfish and carp fish.[1]Haff disease is named after the Königsberg Haff (or lagoon) that borders the Baltic coasts of Russia and Poland. This lagoon is the site at which the disease was f irstly reported in 1924.[2]
In the summer and fall of 1924, it was reported there was an outbreak of illness characterized by sudden and severe muscular rigidity without neurological abnormalities, fever,splenomegaly or hepatomegaly.[2]It was noted the only discernible commonality between patients was a previous consumption of cooked freshwater fish (such as burbot,eel and pike). Most patients presented with coffeecolored urine and there were a few fatalities. Of those who survived, most recovered quickly without sequel.Following this, similarly described outbreaks were reported along the coast of the “Haff” in the following nine years. It is estimated this affected approximately 1,000 people.[2]
Other outbreaks resembling that from the Haff were also reported in Sweden and Soviet Union from 1934 to 1984.[2]Now known as the Haff disease, it is thought to be caused by an unidentif ied heat-stable toxin.[3]Haff disease made its first appearance in the U.S. in 1984 and were reported to be associated with consumption of buffalo f ish, crawf ish and salmon.[4]The f irst reports for Haff disease in Beijing (China) were in 2000,[5]however there are still recent reports about crayfish-related rhabdomyolysis in the middle and lower reaches of the Yangze River.[6-9]
Crayfish accounted for almost all outbreaks and patients were predominately adults. Serious complications included renal failure, multi-organ failure and death, though these are rare.[1]Nonetheless, all suspected cases of Haff disease are requested to report to public health authorities.[1]
Haff disease targets and damages striated muscle and causes rhabdomyolysis with through the release of myoglobin, creatinine kinase (CK) and other muscle cell enzymes.[7]The U.S. Centers for Disease Control and Prevention (CDC) defines Haff disease as a painful myotoxic condition that meets the following criteria: i)a positive cooked seafood ingestion history within 24 hours; ii) a markedly elevated (specifically a 5-fold or greater rise over normal) serum CK level; and iii) a CKmuscle/brain (MB) fraction <5%.[2,10]
Here, we retrospectively analyzed the clinical data of 16 patients admitted to our emergency department with Haff disease after eating crayf ish. The study aimed to explore the clinical characteristics and laboratory f indings, treatments and prognosis of these patients.
METHODS
Data collection
The clinical data of 16 patients with Haff disease after eating crayfish admitted in the Emergency Department of Beijing Chao-yang Hospital between June 2013 and August 2017, were retrospectively analyzed. Rhabdomyolysis caused by trauma, drugs and auto-immune diseases were excluded from this study.Clinical parameters included gender, age, complications,predisposing factors, symptoms, manifestations, prognosis and length of hospital stay. Laboratory parameters included white blood cells count, hemoglobin, platelets,alanine transaminase (ALT), aspartate transaminase(AST), blood urea nitrogen (BUN), creatinine (CREA),myocardial enzymes and myohemoglobin. Treatments included f luid therapy and urine alkalization.
The diagnosis criteria of Haff disease after eating crayfish included the following: unexplained myalgia and rhabdomyolysis with a markedly elevated level of(fivefold or greater increase over normal level) serum creatine phosphokinase (CPK), as well as cooked seafood consumption within the previous 24 hours.[3,4]
Statistical analysis
Continuous variables were described as the mean± standard deviation and were compared using oneway analysis of variance (ANOVA) for the normally distributed data. For skewed distributions, the data was presented as the median (interquartile range) and compared using the Mann Whitney-U nonparametric test.The categorical variables were described as percentages and were compared using the chi-squared test or Fisher’s exact test. Data was analyzed using SPSS 22.0 statistical software package (SPSS Inc, Chicago, IL, USA).
RESULTS
Patients baseline characteristics
Totally 16 patients enrolled in this study. The mean age was 28.38±6.79 years old. Twelve patients ate crayfish in a restaurant, and the remaining 4 patients ate at home. Eleven patients ate crayfish only, while 5 patients had also drank alcohol and 2 patients did strenuous excises. Thirteen patients only ate the crayf ish head. Lastly, 3 patients had a previous allergic history with seafood.
All patients developed symptoms in the summer months between June and August. Myalgia developed in all 16 (100%) patients and fatigue occurred in 14(87.5%). Seven (43.8%) patients developed nausea and vomiting, 10 (62.5%) patients had headache and dizziness, 6 patients had chest tightness and 3 (18.8%)patients had fever (Table 1).
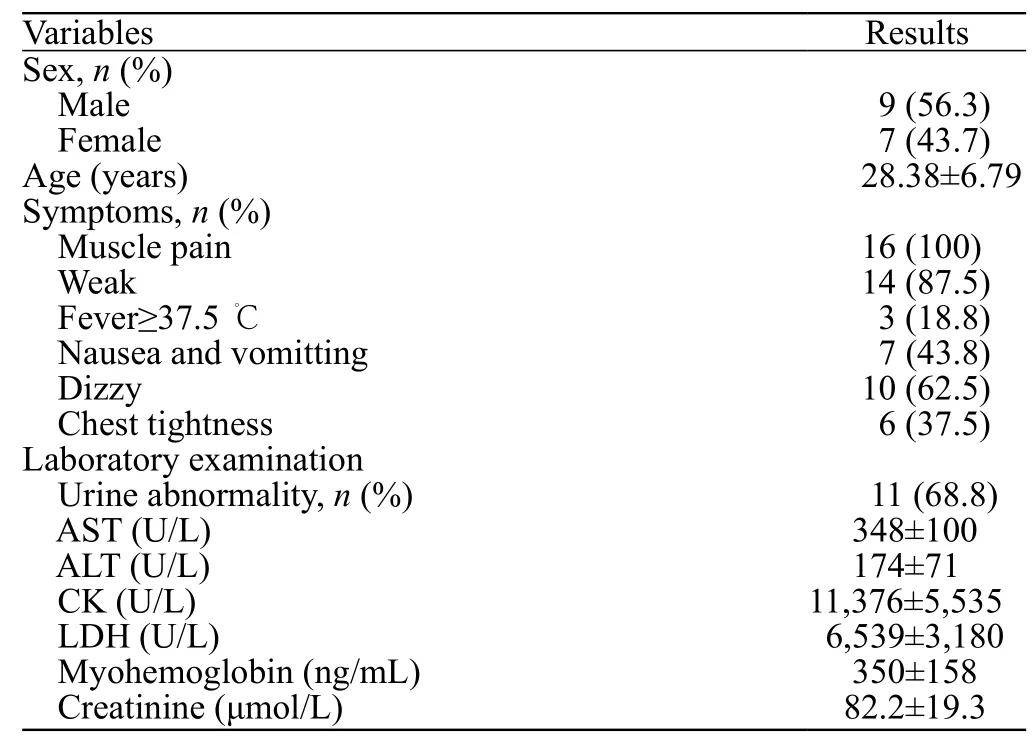
Table 1. Clinical characteristics and laboratory data of patients with Haff disease
Laboratory f indings
Eight patients were positive in the urine occult blood test and 5 patients had proteinuria. All 16 patients developed liver dysfunction. The following elevated levels were reported: ALT (174±71 U/L), AST (348±100 U/L), CK, lactate dehydrogenase (LDH) (6,539±3,180 U/L) and myohemoglobin (MYO) (350±158 ng/mL).Of these, the elevation of CK is the most obvious(11,376±5,535 U/L) compared to the normal range of 38-174 U/L. Only one patient developed renal dysfunction and all others presented as normal (82.2±19.3 μmol/L)(normal range 41-86 μmol/L).
Treatments and prognosis
All patients underwent fluid therapy (involving intravenous infusion of 3,000-4,000 mL isotonic saline every day) to maintain the amount of urine at 100-150 mL per hour. Alkalizing urine by sodium bicarbonate infusion was used to increase the pH value of urine > 6.5.Other treatments included liver function preservation and keeping water and electrolyte balanced.
The symptoms of myalgia in all patients disappeared at 24 to 72 hours after treatment. Liver function and CK level gradually returned to be normal after 72 hours. All 16 patients had good prognosis without obvious renal dysfunction.
DISCUSSION
Rhabdomyolysis is a condition in which injury to the muscle cells results in a breakdown of the cells and leakage of contents into the blood stream. This could lead to the characteristic dark urine due to the elevated serum CK level, muscular pain/tenderness, stiffness, weakness,edema and impaired mobility.[11]Impaired skeletal muscle releases different forms of CK, but CK-MM is the most common isoform of skeletal muscle and therefore is what is measured to diagnose rhabdomyolysis.[11]The level of CK-MM commonly reaches to 100,000 IU/L or more,but acute rhabdomyolysis should be suspected at any CK level above 5,000 IU/L (as total CK level rarely exceed that in cardiomyopathy).[11]
Haff disease is a rare form of rhabdomyolysis,characterized by myalgia often accompanied by myoglobinuria after the ingestion of cooked fish and crustaceans. The proposed mechanisms for acute renal failure in patients with rhabdomyolysis include:i) blockage of the renal tubules with precipitated myoglobin; ii) cortical damage from oxygen free radicals; and iii) myoglobin-induced vasoconstriction of renal arteries.[10]Other proposed mechanisms of Haff disease include other causes of seafood poisoning by heat-stable toxins, typically the bioaccumulation of red and blue-green algal toxins.
Haff disease was firstly reported in Beijing in 2000,and there has since been an obvious increase in the number of reports from other cities.[1]The epidemiological characteristics of the patients with Haff disease in our reports include the following: i) common onset in summer (July to September); ii) a previous history of eating crayfish before the onset of disease; iii) myalgia accompanied by fatigue,dizziness and palpitation; and iv) laboratory findings of an elevation of CK and myohemoglobin. These characteristics are similar to previous reports.[12,13]
Rhabdomyolysis after eating crayf ish usually happens in the middle and lower reaches of the Yangtze River in China. There are heavy rains and water logging in summer, which could easily lead to heavy pollution in these regions. Most of the previous reports are concentrated to the Yangtze River valley,[6-9]however our cases for research were developed in Beijing. Our investigation revealed that all patients had a history of eating crayf ish heads, where there are enriched levels of heavy metals. Previous studies have hypothesized that crayf ish may be contaminated by an unknown toxin, and that the crayf ish itself has autoimmune abilities.[14]
Another factor to note is that 7 (43.75%) patients in our study had a history of undergoing strenuous exercise and drinking alcohol. These could aggravate injury of skeletal muscle cells and potentially lead to the leakage of the cell contents into the blood stream, thus causing an impairment of renal function. However, further in-depth analysis is needed to explore these confounders in our future studies.
CONCLUSION
In conclusion, rhabdomyolysis after eating crayfish is a rare syndrome characterized primarily by unexplained myalgia and fatigue. For those who develop the syndrome, there is a good prognosis with little severe complications. Familiarity with the epidemiological and clinical features of the disease could lead to early diagnosis and prevent any potential renal failure. More researches are needed to f ind out the responsible toxin so preventive measures can be put in place.
ACKNOWLEDGEMENTS
The authors thank Dr. Jiang Zhang for his technical assistance and Dr. Qian Zhang for the advice in data analysis.
Funding:This research was supported by the Beijing Natural Science Foundation (7182055)and Beijing Municipal Administration of Hospitals Incubating Program (Px2016022).
Ethical approval:The protocol was approved by the medical ethics committee of Beijing Chao-yang Hospital.
Conflict of interest:The authors declare that they have no conf licts of interest.
Contribution:CJW and HJZ contributed equally to this study. All authors have substantial contributions to the acquisition, analysis,or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; and f inal approval of the version to be published.
 World journal of emergency medicine2019年3期
World journal of emergency medicine2019年3期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Retroperitoneal hematoma following common iliac artery injury in a child
- Benef its of using an endotracheal tube introducer as an adjunct to a Macintosh laryngoscope for endotracheal intubation performed by inexperienced doctors during mechanical CPR: A randomized prospective crossover study
- Are radiological modalities really necessary for the long-term follow-up of patients having blunt solid organ injuries? A single center study
- A comparison of simulation versus didactics for teaching ultrasound to Swiss medical students
- Prioritization of factors related to mental health of women during an earthquake: A qualitative study
