Practical Clinical Application of Cardiac Computed Tomography– Derived Fractional Flow Reserve
Talal Alzahrani, MD , Ahmed Tashkandi, MD , Abdullah Sarkar, MD , Claudio Smuclovisky,MD , James P.Earls, MD and Andrew D.Choi, MD ,
1 Division of Cardiology, The George Washington University School of Medicine, Washington, DC, USA
2 Department of Medicine, University of Miami, Miami, FL, USA
3 Diagnostic Imaging Center, Holy Cross Hospital, Fort Lauderdale, FL, USA
4 Department of Radiology, The George Washington University School of Medicine, Washington, DC, USA
Abstract
Keywords: coronary artery disease; cardiac computed tomography; fractional flow reserve; fractional flow reserve derived by computed tomography; Ischemia
Introduction
In the past decade, advances in coronary computed tomography angiography (CTA) technology have resulted in high sensitivity and negative predictive value in detecting coronary artery disease (CAD)compared with invasive coronary angiography(ICA), particularly for patients with mild or severe stenosis [1–4].However, anatomical evaluation of CAD by CTA has modest specificity for patients with intermediate-grade stenoses [5, 6].On the basis of this evidence, both major American multisociety guidelines and the European Society of Cardiology recommend the assessment of the functional signifi-cance of CAD in patients with intermediate coronary stenosis before any coronary intervention or stent placement [7, 8].In clinical practice, the functional significance of coronary stenosis is usually assessed
with a noninvasive test such as single-photon emission computed tomography (SPECT) or by invasive fractional flow reserve (I-FFR) measurement.Coronary CTA as an anatomical test has had limited value in assessing the functional significance of coronary artery stenosis.The recent development of the use of cardiac computed tomography (CT)-derived fractional flow reserve (FFR-CT) seeks to address this gap as a proposed method of functional assessment of CAD by CTA.
In this article we aim to mix common clinical cases with the current technical methods, validation, outcomes, and registry studies of FFR-CT analysis to guide the cardiac imaging specialist in evaluating this technique.We also provide a review of flnancial issues related to FFR-CT analysis.
The Importance of I-FFR
I-FFR-guided percutaneous coronary intervention (PCI) has been shown to improve the clinical outcomes and reduce the cost of treating patients with CAD compared with standard angiographyguided PCI as well as medical therapy alone[9–13].Despite the benefits of I-FFR guidance, the method is limited by several factors, which make it difficult to apply this approach in daily routine clinical practice.The use of I-FFR can increase case complexity through the risk of hypotension associated with adenosine use and catheterbased complications such as coronary perforation and dissection.Therefore, FFR-CT analysis was developed as an alternative, noninvasive technology to predict the functional significance of coronary artery stenosis.
Case 1: A 75-Year-Old Woman Presenting with Chest Pain
FFR-CT Method
FFR-CT analysis is a technique developed and owned by HeartFlow Inc.(Redwood City,California, United States).As a case example of FFR-CT analysis in a 75-year-old woman presenting with chest pain, see Figure1.This modeling applies computational fluid dynamics (CFD) to the images from coronary CTA without modification of CTA acquisition protocols to predict I-FFR [14].Modern CFD uses Navier-Stokes equations to describe the relationship between the characteristics, including viscosity, velocity, pressure, temperature, and density, of a moving fluid [15–17].The use of CFD in coronary CTA aims to determine the physiologic significance of coronary artery stenosis in patients with moderate to severe coronary artery stenosis on CTA images as an alternative to the use of I-FFR.
The estimation of FFR-CT depends on three main factors: (1) the anatomical region of the lesion,(2) the boundary conditions at the lesion, and (3)the physical laws of fluid flow.The calculation of FFR-CT is achieved by the following steps: First,an anatomical model for the coronaries is developed from a coronary CTA study.Second, the normal baseline coronary artery flow for the patient is quantified hypothetically for the total coronary arteries and each branch of the coronary arteries.Third, baseline microcirculation resistance is estimated by the CFD technique.Fourth, the change in coronary resistance with hyperemia is estimated.The algorithm incorporates a calculated assumption about the microvascular response to adenosine.Finally, coronary flow, pressure, and velocity at rest and hyperemia are estimated by use of the laws of physics governing fluid dynamics to predict I-FFR [18].The formal processing takes place at HeartFlow’ s central laboratory in California with a special technician and reported process time of 6 hours per patient.In the authors’ clinical practice, this processing time has been 2– 4 hours for an urgent case.Thus, coronary CTA images need to be transferred from the imaging site to the HeartFlow laboratory via encrypted transmission over the Web.
For the practicing clinician, factors from the scanned CT dataset that enable off-site calculation of FFR-CT include quantification of myocardial mass (to calculate coronary blood flow), modeling of the epicardial coronary vessels (diameter and length), and incorporation of CT-based atherosclerosis lesion length and coronary plaque burden[19, 20].
FFR-CT Validation Studies
FFR-CT was initially validated in three major clinical studies that were published between 2011 and 2014.Koo et al.[14] conducted the Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve(DISCOVER-FLOW) study to determine the diagnostic performance of FFR-CT in patients with suspected or known CAD.This study included 103 patients at four clinical sites who underwent coronary CTA and ICA with I-FFR evaluation.This study revealed that FFR-CT analysis increased the diagnostic accuracy of coronary CTA to identify fractional flow reserve (FFR) of 0.80 or less from 58 to 84% compared with ICA on a per-vessel basis.Nakazato et al.[21] expanded on the DISCOVERFLOW study by conducting the Determination of Fractional Flow Reserve by Anatomic Computed Tomography Angiography for Coronary lesions of Intermediate Stenosis Severity (DeFACTO) study to assess the diagnostic performance of FFR-CT in patients with intermediate coronary stenosis.This study included 252 patients from 17 centers and flve countries who underwent coronary CTA and ICA with I-FFR of 0.80 or less as the gold standard.In this study, FFR-CT analysis increased the accuracy of coronary CTA for intermediate coronary stenosis (defined as stenosis of 30– 70%) from 63 to 71% on a per-patient basis.Finally, N ø rgaard et al.[22] conducted the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps) at ten sites in Europe, Asia, and Australia using a refined version of FFR-CT technology to determine its diagnostic performance.This study included 254 patients who underwent coronary CTA and ICA with I-FFR evaluation.This study showed that FFR-CT analysis increases the accuracy of coronary CTA from 53 to 81%.Of note,12% of the scans were excluded because of image artifacts.In summary, validation studies demonstrated that FFR-CT analysis improves the performance and increases the accuracy of coronary CTA compared with ICA in detecting patients with significant CAD.
Case 1 Follow-up
With FFR-CT of 0.56, considered hemodynamically significant, the patient was referred for invasive angiography for PCI for symptom relief of anginal chest pain.
Case 2: A 58-Year-Old Woman with Hypertension and Hyperlipidemia Presenting to the Emergency Department with Chest Pain
FFR-CT Effect on Invasive Angiograms
Several clinical studies evaluated the clinical outcome and downstream effect on invasive angiograms of the use of FFR-CT analysis compared with standard care.As a real-world example of FFR-CT on deferred angiography, see Case 2 ( Figure2).Douglas et al.[23] performed an observational comparative effectiveness study, supported by HeartFlow, the Prospective Longitudinal Trial of FFR-CT: Outcome and Resource Impacts (PLATFORM) study, in symptomatic patients with suspected CAD to compare the outcomes of FFR-CT analysis versus routine functional testing.This study, which included 584 patients, revealed that FFR-CT analysis lowers the rate of unnecessary ICA compared with routine functional testing.Among study participants, 38%of patients in whom noninvasive evaluation had been planned had stenosis of 50% or greater, while 61% of patients in whom invasive angiography had been planned had stenosis of 50% or greater.Invasive angiography was cancelled for 61% of patients receiving FFR-CT results.Lu et al.[24]conducted an observational cohort study in patients with stable chest pain in the PROMISE trial who were referred for ICA after coronary CTA to determine if FFR-CT predicts coronary revascularization and outcomes.This study included 271 patients, of whom 181 patients underwent FFR-CT analysis.In this study, FFR-CT of 0.8 or less was a better predictor of revascularization and major cardiac adverse events compared with severe stenosis in coronary CTA.This study also showed that FFR-CT of 0.80 or less could decrease unnecessary ICA by 44% and increase the proportion of ICA leading to revascularization (appropriate ICA) by 24%.Rabbat et al.[25]showed in a single-center study that FFR-CT analysis reduces unnecessary ICA without an increase in cardiac adverse events in symptomatic patients with suspected CAD compared with coronary CTA alone.
Bilbey et al.[26] modeled, in a study of 1000 symptomatic patients with suspected CAD,the impact of FFR-CT analysis on radiation dose exposure and downstream clinical event rate.This study included four intervention arms (dobutamine echocardiography, SPECT, coronary CTA, and FFR-CT analysis).The results of this study suggested that an approach using FFR-CT analysis(9.7 mSv; 3.7 mSv for coronary CTA, 4.2 mSv for angiography, 1.8 mSv for PCI) has lower radiation dose exposure compared with an approach involving a nuclear stress test (26.5 mSv).This study also showed that the FFR-CT group had the lowest cardiovascular event rate (death/myocardial infarction) at 1 year.To summarize these studies, FFR-CT analysis reduced the need for invasive angiography by 44– 63% without significantly higher cardiovascular event rates.
Real-World Experience: ADVANCE Registry
To move FFR-CT analysis from the clinical trial world to clinical practice, Chinnaiyan et al.[27] in conjunction with HeartFlow designed the Assessing Diagnostic Value of Non-invasive FFRCT in Coronary Care (ADVANCE) registry to evaluate the impact of FFR-CT analysis on decision making, outcomes, and resource utilization.The primary outcome was the reclassification of the treatment strategy.For each patient, an independent review committee developed a management plan that was compared with the therapy delivered by the patient’ s local physician team, who then had the opportunity to reevaluate their strategy.The results were presented in September 2018 at the European Society of Cardiology Congress for 5083 patients from 38 international sites for patients with 30%or more stenosis on coronary CTA [28].Seventy percent of patients were reclassified to have medical therapy and 24% were reclassified to undergo a PCI approach.While 62% of patients had an abnormal FFR-CT of 0.80 or less in at least one coronary vessel, 34% of local-site patients and 47% of the core laboratory patients were recommended for revascularization, with 54% of deferrals occurring for patients with FFR-CT of 0.75– 0.80.The site of the coronary involvement (proximal vs.distal)and at-risk myocardium was not reported by the study investigators.There were no deaths or myocardial infarction within 90 days for patients with FFR-CT greater than 0.80, while there were four patients with myocardial infarction and ten deaths in patients with FFR-CT of 0.80 or less.A limitation of the registry was that about 24% of patients were asymptomatic, perhaps reflecting local practice for the evaluation of ischemic heart disease at international sites.Another important limitation is that about 15% of patients with FFR-CT of 0.8 or less had no atherosclerosis or mild stenosis (0– 30%) on coronary CTA.Potential explanations for this flnding include small coronary diameter due to either anatomical variability or inadequate patient preparation with beta-blockers and nitroglycerin as well as poor image quality.
Case 2 Follow-up
Optimal medical therapy was added for this patient.With FFR-CT greater than 0.8 in the left anterior descending artery, this lesion was managed medically, and the patient was referred for PCI for the obtuse marginal stenosis with hemodynamically significant FFR-CT of 0.69.
Case 3: A 66-Year-Old Man with Hypertension, Diabetes Mellitus, and a Family History Of Premature CAD Presented with Fatigue
FFR-CT in Unique Populations (e.g., after Coronary Intervention, Acute Chest Pain,Hypertrophic Cardiomyopathy, Multivessel CAD, and Surgical Planning)
FFR-CT was evaluated in patients who presented to an emergency department with chest pain to evaluate the association between the measurement of FFR-CT and high-risk plaque.Ferencik et al.[29]measured FFR-CT in patients from the ROMICAT II trial who either had more than 50% stenosis or underwent a secondary noninvasive test.This study showed that abnormal FFR-CT was signifi-cantly associated with high-risk plaque.The highrisk plaque was determined on the basis of qualitative (positive remodeling, low-CT-attenuation plaque, napkin ring sign, spotty calcium) and quantitative (plaque volume, density less than 30 HU,remodeling index greater than 1.1) measurements.This study also showed that adding FFR-CT and high-risk plaque measurement to severe anatomical stenosis increased the discriminatory capacity (the area under the curve increased from 0.77 to 0.87)for acute coronary syndrome significantly compared with stenosis only.
FFR-CT was also studied in patients with hypertrophic cardiomyopathy (HCM).Sellers et al.[30]used FFR-CT in a retrospective analysis to evaluate the coronary artery volume to the myocardial mass ratio.This study compared patients with HCM with patients with normal structural heart and revealed that patients with HCM have decreased coronary artery volume to myocardial mass ratio despite the increase in the coronary artery volume.The coronary artery volume to myocardial mass ratio might be used in the future as a way to grade the severity of HCM and predict the clinical outcome among patients with HCM.
FFR-CT analysis was also investigated in a small prospective study as a novel noninvasive technology to predict the functional outcome of coronary stenting [31].The functional outcome was predicted by estimation of the coronary blood flow after virtual stenting of a coronary lesion.Virtual stenting was achieved by modification of the coronary flow model in FFR-CT analysis to eliminate ischemiacausing stenosis.This study recruited 44 patients with functionally significant coronary artery stenosis (48 lesions).These patients initially underwent coronary CTA and then had ICA with stenting and I-FFR evaluation before and after stenting.This study revealed that the diagnostic accuracy of FFR-CT after stenting was 96% compared with I-FFR.This technology might be used in the future to determine if coronary stenting is necessary by predicting the change in the coronary flow that is associated with coronary stenting.
More recently, FFR-CT was used to calculate the noninvasive functional SYNTAX score in patients with three-vessel CAD.This method was tested in a retrospective study, which included 77 patients from the SYNergy between PCI with TAXus and Cardiac Surgery II (SYNTAX II) study [32].In this study, the noninvasive functional SYNTAX score(obtained in only 53 patients) was not significantly different from the invasive functional SYNTAX score.The main limitation of this study was the small sample size.As an approach that would allow direct revascularization after noninvasive CTA, this presents an intriguing idea requiring further validation in large clinical prospective studies.
FFR Limitations
To review a case example of a patient with multivessel CAD with limitations of FFR-CT, see Figure3.While FFR evaluation serves as a validated, invasive approach for coronary physiology,this method focuses on the epicardial vessels without fully accounting for the coronary microcirculation.In contrast, the evaluation of coronary flow reserve(CFR), perhaps best noninvasively measured by positron emission tomography, accounts for coronary epicardial and microcirculatory flow to quantitatively evaluate the reserve vasodilator capacity of the coronary resistance vessel [33, 34].A 30– 40%discordance has been reported between CFR and I-FFR.Within the backdrop of CFR, I-FFR can be overestimated (falsely normal) in patients with intermediate stenosis and increased microvascular resistance because distal pressure depends on flow across the stenosis, which is determined by both epicardial coronary stenosis and microvascular resistance [33,34].Conversely, CFR can be underestimated with a falsely abnormal I-FFR in these patients because the flow velocity decreases with an increase in microvascular resistance.With regard to CFR, no randomized controlled clinical trials have yet evaluated the use of CFR to guide coronary intervention.While FFR-CT accounts for microcirculatory circulation,the assumptions used in the calculations may account for discordance among FFR-CT, I-FFR, and CFR.To evaluate this discordance clinically, Cook et al.[35] recently conducted a systematic review of the use of individual vessel data from 908 vessels in the published literature.This study showed that 320 vessels (35%) were categorized ischemic by FFR-CT, whereas 244 vessels (26.8%) were categorized ischemic by I-FFR as defined by a value below 0.8.The overall diagnostic accuracy of FFR-CT was 81.9% (95% confidence interval [CI] 79.4– 84.4%)for cutoff values of less than 0.63 or more than 0.83.In the intermediate range of values, the diagnostic accuracy was 74.7% (95% CI 71.9– 77.5%) and 46.1%(95% CI 42.9– 49.3%) for cutoff values of 0.60– 0.70 and 0.70– 0.80, respectively.This last point raises the question of whether FFR-CT of 0.7– 0.8 improves discrimination of ischemia in this important range.
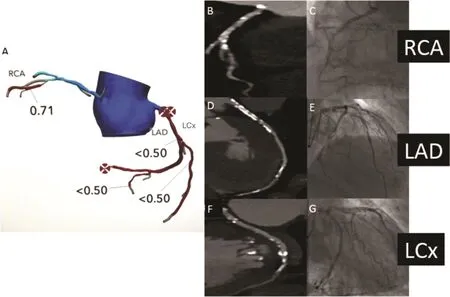
Figure3 A 66-Year-Old Man with Hypertension, Diabetes Mellitus, and a Family History of Premature Coronary Artery Disease Presented with Fatigue.
The authors also note from their analysis that explanations for this modest correlation include uncertainty in the reproducibility of FFR or FFR-CT analysis as well as uncertainty regarding the optimal cutoff for FFR (0.75 vs.0.80).A limitation of the analysis by Cook et al.is potential differences in the point at which the FFR or FFR-CT values were measured.A significant FFR-CT value in the distal part of the vessel may not be correlative with an I-FFR value just beyond the reported stenosis.An editorial by N ø rgaard et al.[36] several months later addressed the analysis by Cook et al.with several rebuttals of the angiography data of Cook et al.First, they note that there have been evolving iterations of the FFR-CT algorithm.Second, they point out that the analysis by Cook et al.used values identified from the digitized flgures rather than original raw data, which does not account for concordant FFR-CT and I-FFR values (35% of the values).They also suggest concerns with intratest variability of I-FFR (and any test) not accounted for by Cook et al.Lastly, they propose the use of FFR-CT analysis as a stand-along noninvasive modality with low event rates in patients that would allow deferred invasive angiography.
Case 3 Follow-up
Because of the presence of multivessel CAD from CTA and invasive angiography, the patient was referred for coronary artery bypass grafting.Although the values were less than 0.8, there was notable discordance in the absolute values between I-FFR and FFR-CT.
Alternative FFR-CT Methods
In addition to the methods discussed so far, other major hardware vendors have developed unique proprietary approaches to coronary CT for patients with intermediate coronary stenosis.A discussion of these methods from Canon (formerly Toshiba Medical Systems Corporation, Tokyo, Japan) and Siemens (Forchheim, Germany) follows.
FFR-CT analysis (SurePlaque, Canon Medical Systems Corporation) is performed on a standard desktop workstation with use of reconstructed CT data as described by Ko et al.[37].The images are obtained through 320-detector CT with acquirement phases of 70, 80, 90, and 99% R-R intervals to assess the luminal deformation of the coronary arteries and aorta during the diastolic phase of the cardiac cycle.The blood fluid hypothesis is modeled as non-Newtonian.Hierarchical Bayes modeling is used to merge CT data and structural and fluid analysis conditions.Fluid simulation is computed by a flxed-element mesh model and reduced-order (onedimensional) model of coronary outlet to calculate tubular cross section flow and pressure of the coronary tree.Initial experience suggests that the value is easily interpreted by a physician or radiographer within 30 minutes with a desktop computer [37].
With validation ongoing, Ko et al.have reported in a small, single-center study of 42 patients that the accuracy, sensitivity, specificity, positive predictive value, negative predictive value, and area under the curve for CTA versus FFR-CT analysis to identify FFR of 0.8 or less (Canon) are 78 versus 84%, 79 versus 78%, 74 versus 87%, 60 versus 74%, 88 versus 89%, and 0.77 versus 0.88, respectively [38].The results indicate FFR-CT analysis (Canon) has better specificity and PPV than CTA alone, while the sensitivity, NPV, and accuracy are approximately similar.
With regard to the Siemens approach, several small studies from multiple centers have been published to determine alternative FFR-CT methods calculated by an onsite desktop computer, with accuracy ranging from 80 to 90% for the detection of obstructive CAD [38–42].In one of the studies,Coenen et al.[43] compared the diagnostic accuracy of machine learning (ML)-based FFR-CT with CFD-based FFR-CT.Five hundred twenty-five vessels with I-FFR measurements from 351 patients were included for comparison.There was very good correlation between ML-based and CFD based FFR-CT, with a Pearson correlation coefficient of 0.997.There was a general shift of lower precision toward the I-FFR threshold of 0.8.The ML-based FFR-CT processing time is relatively short, unlike for the CFD approach, which ranges from 10 minutes to several hours [43].While intriguing, further multicenter studies are required for these on-site analyses before broader clinical implementation.
FFR-CT Cost Analyses
The initial potential economic outcomes of HeartFlow FFR-CT analysis have been evaluated in several studies.Hlatky et al.[44] showed in symptomatic patients without known coronary disease in whom ICA is planned that FFR-CT analysis reduces the cost of care compared with usual care ($7343 vs.$10,734; P < 0.01).Rabbat et al.[25] suggested that in symptomatic patients with suspected CAD,FFR-CT analysis reduces the cost of care compared with coronary CTA alone ($1567 vs.$1355;P = 0.001).
Moving from economic modeling to real-world cost, the current published US Medicare fee for HeartFlow analysis is $1450.There are now a broad number of US private insurers that cover FFR-CT analysis, including Cigna, Blue Cross Blue Shield,and United Healthcare.As part of these coverage decisions, in June 2018, eviCore, a large US beneflts management company, also adopted a policy of use of coronary CTA as a flrst-line test.The Centers for Medicare and Medicaid Services assigned a new technology Ambulatory Payment Classification for the analysis as of January 1, 2018.However,Medicaid coverage is lacking.
Because of these developments, a robust realworld analysis of the cost of this approach is uncertain.As per Villines [45], with the relatively low cost of coronary CTA, it is expected that FFR-CT analysis could increase the overall cost of a cardiac CT study more than fourfold.In addition, there have not yet been robust independently funded studies,with HeartFlow funding all major studies to date.It should also be pointed out that HeartFlow has raised nearly 500 million dollars in venture capital[46] as a Silicon Valley company [45, 47].
Concluding Thoughts
In conclusion, FFR-CT has been evaluated in a broad range of clinical scenarios for patients with CAD and intermediate stenoses in validation studies and, most recently, the large ADVANCE multicenter registry with promising results.There is also potential for FFR-CT to be used for patients with known CAD to allow effective stent planning and in the evaluation of patients with multivessel CAD.By providing information on the physiologic evaluation of stenoses, this early evidence suggests that this technology will enable a reduction in invasive angiography and allow a medical therapy approach for a greater number of patients.
Importantly, potential alternatives to the HeartFlow FFR-CT approach include CT perfusion and, most recently, quantitative plaque analysis,which may offer additional refined approaches to the evaluation of the functional significance of coronary artery stenosis.Quantitative assessment may allow improved prediction of high-risk plaques [48,49] and the ability to predict coronary ischemia.Perhaps most importantly, direct quantification of atherosclerotic plaque burden may become more beneficial for improving risk stratification for CAD while also providing a noninvasive approach to assess the response to novel drug therapies through direct serial assessment of coronary artery plaque volume.These approaches have also begun to be assessed in broad multicenter trials [50, 51].
The ability of HeartFlow analysis to gain wide coverage through Medicare, through many private payers, and in national health care systems (e.g., the UK National Health Service) has been impressive;however, the ultimate cost to patients and the health care system is unclear.For patients who undergo HeartFlow analysis without payer availability (e.g.,Medicaid patients), it is likely that either the hospital or the patient will have to absorb the cost of the test.At the very least, a positive development from the authors’ perspective is that the broadened coverage of FFR-CT analysis has enabled increased payer coverage of coronary CTA.
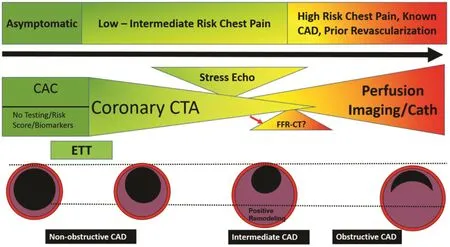
Figure4 FFR-CT within the Current Landscape of Imaging Evaluation of Coronary Artery Disease in the Asymptomatic,Low-Intermediate Risk and High-Risk Chest Pain Patient.
As clinical decision making in the real-world includes both patient-specific factors (clinical risk,patient preferences, ability to achieve optimal medical therapy) and the evaluation of coronary stenosis and physiology, the effect of the FFR-CT value on real-world practice remains uncertain.For the vast majority of patients with mild stenosis and severe stenoses, coronary CTA will be most informative ( Figure4 ).For patients with high-risk chest pain, known CAD, or prior revascularization, stress perfusion (by nuclear imaging, cardiac magnetic resonance imaging or positron emission tomography) is well established, with invasive angiography with FFR evaluation serving as the gold standard approach ( Figure4).Also an open question is the value of coronary revascularization for patients with stable ischemic heart disease regardless of the presence of any cardiac testing as per current clinical guidelines.The ongoing International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) may provide some answers to this question [52].There are as yet no randomized long-term trial data on patients receiving intervention versus no intervention based on FFR-CT data.
It is the belief of the authors that FFR-CT analysis will help reduce additive functional testing, as well as importantly invasive angiography for the small proportion of patients with intermediate stenosis undergoing coronary CTA where the atherosclerosis significance is uncertain.The cases shown (particularly cases 1 and 2) in this article demonstrate the progress that has been made in the application of FFR-CT analysis in a real-world clinical setting.The opportunity to guide potential revascularization decisions in patients with known CAD without invasive angiography is intriguing but not yet proven, with limitations as shown in the heavily calcified coronaries in case 3.In addition, the cardiac imaging fleld requires unbiased studies to understand the costs and outcomes associated with this approach in real-world practice.Given these considerations, the role for FFR-CT analysis may be as a helpful adjunctive technology for a subset of patients undergoing coronary CTA after future study ( Figure4).
Conflict of Interest
The authors declare that they have no conflicts of interest.
 Cardiovascular Innovations and Applications2019年2期
Cardiovascular Innovations and Applications2019年2期
- Cardiovascular Innovations and Applications的其它文章
- A Tale of Two STEMI’ s
- Adult Congenital Heart Disease in the Veteran Population: A Case-Based Report
- Differential Impact of Appropriate Use Criteria on the Association between Age and Abnormal Stress Myocardial Perfusion SPECT
- Using 3D-Printed Models to Advance Clinical Care
- Evaluation of the Patient with Incidental Left Ventricular Hypertrophy on Echocardiography
- Imaging Beyond the Angiogram in Women with Suspected Myocardial Infarction and No Obstructive Coronary Artery Disease
