A Tale of Two STEMI’ s
C.Richard Conti, MD, MACC
Correspondence:C.Richard Conti, MD, MACC,University of Florida Medical School, Gainesville, FL, USA,E-mail: conticr@medicine.ufl.edu
Introduction
Occasionally a clinical dilemma occurs when two patients with a myocardial infarction associated with ST segment elevation on the electrocardiogram,arrive in the emergency department at the same time.Since most cardiologists would consider that these patients have an occlusion of an epicardial coronary, and should undergo an immediate revascularization, a decision must be made as to who should go to the catheterization laboratory flrst.
Differential Diagnosis of ST Segment Elevation
St Segment elevation on the ECG is usually due to occlusion of an epicardial blood vessel, but not always.The following can result in ST elevation:Thrombotic occlusion of a blood vessel, Vasospasm, Epi myocarditis, Takotsubo,Physiologic.
Coronary Disease
The state of the coronary arteries is not known until angiography is performed but as a guess it is more likely than not that a patient with a recovered cardiac arrest has multivessel coronary disease and more extensive LV necrosis than the patient who did not have the cardiac arrest.
Hospital Staff Necessary to Cover Acute Myocardial Infarction
Most hospitals who have cardiologists that perform urgent revascularizations have cardiologists and catheterization laboratory staff, available 24/7 to handle this problem but may not have on-call nonphysician catheterization staff to handle a second patient on a 24/7 basis.
Decision Time
When two patients with a myocardial infarction with ST segment elevation arrive in the emergency department at the same time, the cardiologist is faced with a decision point; should he/she send one of the patients to another facility or should the patient with the best prognosis go to the laboratory and have the vessel opened and the patient with a poor prognosis be put on standby or given thrombolytic therapy.
Therapy should not withheld from the second patient since Nitrates, Blockers, anticoagulants,anti-platelet agents, and thrombolytic therapy are available to any patient who comes into hospital with an ST segment elevation or non-ST segment elevation myocardial infarction.
Patient Presentation
I present two patients, one of which will not likely survive for a year despite the similarity of LV function as determined by an echocardiogram.
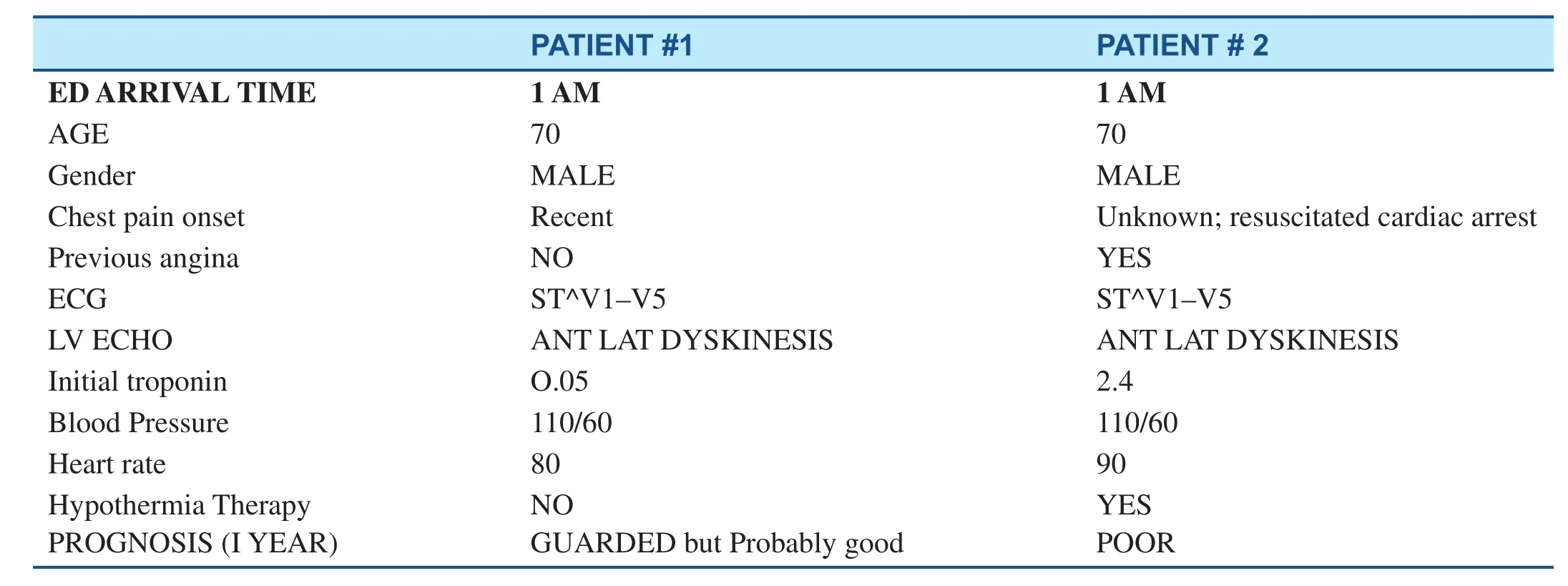
PATIENT # 1 PATIENT # 2 ED ARRIVAL TIME 1 AM 1 AM AGE 70 70 Gender MALE MALE Chest pain onset Recent Unknown; resuscitated cardiac arrest Previous angina NO YES ECG ST^V1–V5 ST^V1–V5 LV ECHO ANT LAT DYSKINESIS ANT LAT DYSKINESIS Initial troponin O.05 2.4 Blood Pressure 110/60 110/60 Heart rate 80 90 Hypothermia Therapy NO YES PROGNOSIS (I YEAR) GUARDED but Probably good POOR
Rationale for Decision Making
lv Dysfunction
It is highly likely that there is more necrosis in the cardiac arrest patient.Although LV function looked similar in the two patients, once again, as a guess,the myocardial tissue at risk may be more viable in the flrst patient than in the second and thus prognosis may be better in the flrst patient compared to the second.
Troponin Level
The “ near normal” troponin level, as seen in the flrst patient suggests that the myocardial infarction may have occurred at a time more recent than in the patient with previous angina and cardiac arrest.Of course, some believe that the high troponin level in the second patient may be due to a large Infarction.Still others believe that the high troponin level is due to spontaneous reperfusion due to washout of infarcted myocardium.This is probably unlikely,since the patient still has ST segment elevation on the ECG.
Still others believe that the patient with the lowest Troponin level and ST segment elevation will do well if treated medically without a reperfusion strategy while others believe that the second patient, regardless of the troponin level might be salvageable with urgent PCI/Stent or thrombolytic therapy.
Still others believe that a second on call group be utilized to handle the second patient e.g.EP Staff.Thus, both patients could be taken for urgent LHC and revascularization.
Conclusion
These cases were presented to CV Division Faculty and CV Fellows to obtain their opinion as to the therapy of these two patients.The majority of those polled who responded favored sending the flrst patient for urgent revascularization.
In my opinion, a clinical decision should be made to “ save the potentially savable” and thus I would send the patient with the lowest troponin for immediate revascularization and treat the second patient with thrombolytic therapy.
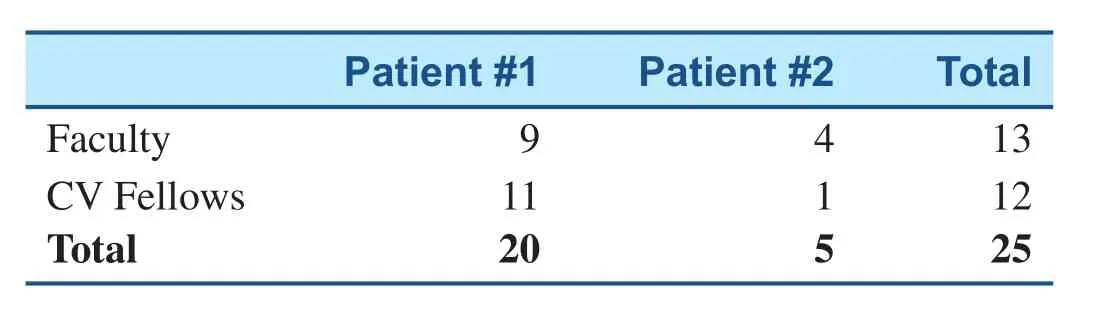
Patient # 1 Patient # 2 Total Faculty 9 4 13 CV Fellows 11 1 12 Total 20 5 25
In a recent issue of JACC: Cardiovascular Interventions
Volume 11, Issue 3, February 2018 “Should We Perform an Immediate Coronary Angiogram in All Patients After Cardiac Arrest? Insights from a Large French Registry” was discussed by Bougouin and colleagues [1].They opined that in cardiac arrest patients, their results suggest that investigations regarding early coronary angiography after OHCA should focus on patients with preserved neurological status and is based on the CAHP score, which is a simple tool, to demonstrate that an early coronary invasive strategy is associated with improved survival in patients with preserved neurological outcome (i.e.,those with a low CAHP score).Low Score = 61% discharged alive.High Score = 3% discharged alive.
The CAHP score is a simple and objective score based on admission parameters, which permits prediction of the neurological outcome in patients admitted to hospital following OHCA.It includes 7 variables associated with poor prognosis (age, non shockable rhythm, time from collapse-to-basic life support (BLS), time from BLS-to-return of spontaneous circulation (ROSC), location of cardiac arrest, epinephrine dose used during resuscitation,and arterial pH.
· So the question arises, “ Should we perform an immediate Coronary angiogram in the patient after Cardiac Arrest? ”
· Maybe!!! But not in every one
· Yes!! if the CAHP score is low i.e.if the neurologic status is good.
REFERENCE
1.Bougouin W, Dumas F, Karam N,Maupain C, Marijon E, Lamhaut L,et al.Should we perform an immediate coronary angiogram in all patients after cardiac arrest? insights from a large French registry.JACC:Cardiovasc Interv 2018;11:249– 56.
 Cardiovascular Innovations and Applications2019年2期
Cardiovascular Innovations and Applications2019年2期
- Cardiovascular Innovations and Applications的其它文章
- Adult Congenital Heart Disease in the Veteran Population: A Case-Based Report
- Differential Impact of Appropriate Use Criteria on the Association between Age and Abnormal Stress Myocardial Perfusion SPECT
- Using 3D-Printed Models to Advance Clinical Care
- Evaluation of the Patient with Incidental Left Ventricular Hypertrophy on Echocardiography
- Practical Clinical Application of Cardiac Computed Tomography– Derived Fractional Flow Reserve
- Imaging Beyond the Angiogram in Women with Suspected Myocardial Infarction and No Obstructive Coronary Artery Disease
