Meta-analysis of neostigmine injections given at the Zusanli (ST 36) acupoint in the treatment of postpartum urinary retention
Yan-Li Chen , Yun-Rui Jin , Yi-Hua Fan , Qiang Zhang
1Southwest Hospital Affiliated to Third Military Medical University, Chongqing, China. 2Chongqing Jiangbei Hospital of Traditional Chinese Medicine, Chongqing, China. 3Tianjin University of Traditional Chinese Medicine, Tianjin, China.4Daping Hospital Affiliated to Third Military Medical University, Chongqing, China.
Background
Urinary retention is a common postpartum complication in which the puerpera has difficulty in auto-urination or retains more than 100 mL urine in the bladder after auto-urination within 6–8 h after giving birth. This condition is often seen in puerpera who have acute urinary retention, cannot urinate within 6 h after vaginal delivery or after removing a urinary catheter installed for lower segment cesarean section, or still have 1500 mL urine in the bladder after auto-urination measured after catheterization or using ultrasound. Puerperae typically complain of abdominal fullness without auto-urination. A full bladder can be found on examination, producing local dullness on percussion. Furthermore, a full bladder can influence the position of the uterine fundus by affecting uterine contraction causing it to move higher or tilt to one side [1]. There are many causes of postpartum urinary retention, including edema of the bladder mucus membrane and reduced muscle tone that develop while giving birth, ignoring the urge to urinate due to postpartum fatigue, flaccid abdominal wall and pelvic muscles, pain in the perineum, and not being used to urinating while on a bed, among others [2]. Postpartum urinary retention always leads to urinary tract infections,cystoplegia, accumulation of metabolic waste in the body,and more colporrhagia caused by bad uterine contraction;therefore, it should be treated in a timely manner [3]. Hot coating, massage, listening to running water sounds, and glycerin enemas do not have a beneficial effect [4].Catheterization has an obvious curative effect, but can often cause urinary tract infection and other complications.
Acupoint injection is a developing method, which started in the 1950s, that combines acupuncture and medicine. This method enhances the effects of acupoint and medicine and reduces side-effects, leading to the use of this method booming in clinical practice. The first report of neostigmine injection given at the Zusanli (ST 36) acupoint to treat postpartum urinary retention was published 1979.
The Zusanli (ST 36) acupoint belongs to the stomach meridian and is used mainly when treating abdominal diseases. It has bidirectional effects on the bladder smooth muscle. Neostigmine can help bladder detrusor muscle contraction to promote urination and has often been used to treat postpartum or postoperative urinary retention. There are many reports of neostigmine injections given at the Zusanli (ST 36) acupoint helping postpartum urinary retention, with different injection methods always having a positive effect. However, most of these studies have a small sample size and are of varying quality. Therefore, we decided to perform a meta-analysis of neostigmine injections given at the Zusanli (ST 36) acupoint in the treatment of postpartum urinary retention.
Methods
Search strategy
An electronic search of Cochrane Library, Pubmed, Web of Science, Chinese National Knowledge Infrastructure,Vip Database, and Chinese Biomedical Literature Database was performed to find randomized controlled trials (RCTs) by using a combination of text words and medical subject heading terms. The electronic search combined terms related to neostigmine, Zusanli (ST 36)acupoint, urinary retention, and postpartum. Two independent reviewers critically checked citations identified in two stages by reading the title/abstract and then the full text.
Study selection
According to the PICOS principle, we identified the following selection criteria: 1) Participants (P): Women who urinated in little drops up to 8 h after delivery, with lower abdominal distension pain, filling of the bladder,tenderness, and normal routine urinalysis; or women in whom a postoperative catheter was placed after cesarean section, having difficulty in urinating 6 h after removal of the urinary catheter, or urinated in little drop or even had a complete lack of urination [7]. There were no limits on the patient's age. Women with serious comorbidities, such as gestational hypertension, pregnancy associated with cardiac disease, an gestational diabetes, or other reasons causing urinary retention were excluded. 2) Intervention:(i) Trials (T): Neostigmine was injected at the Zusanli(ST 36) acupoint in the treatment group. (ii) Controls (C):Neostigmine was delivered by intramuscular injection. 3)Outcomes (O): The overall effect includes cure,effectiveness, and invalid. Total effective rate = Cure rate+ Effective rate; Cure rate = Number of cured persons /Participants ×100%; Effective rate = Effective number /Participants×100%. The diagnostic criteria for dysuria were defined according to the Diagnostic Efficacy Standard of TCM Syndromes formulated by the State Administration of Traditional Chinese Medicine in 1994.(i) Cure: Patients can auto-urinate after 30 min treatment without the feeling of incomplete emptying. The bladder cannot be palpated in the lower abdomen. (ii)Effectiveness: Patients who cannot auto-urinate and drain urine away after initial 30 min treatment can auto-urinate after a further 30 min treatment without the feeling of incomplete emptying. The bladder cannot be palpated when examining the lower abdomen. (iii) Invalid:Patients cannot auto-urinate or have the feeling of incomplete emptying. The bladder can be palpated when examining the lower abdomen. 4) Study design (S):RCTs.
We excluded studies if they met one of the following criteria: 1) the required information was not available to extract the necessary data and the data could not be obtained by contacting the authors, 2) it was a republished study, or 3) the outcome measure was ineligible.
Data extraction
Data were independently extracted by reviewers using a predesigned table, which included title, first author,publication year, sex, age, race, length of illness,diagnostic criteria of postpartum urinary retention,intervention, and outcome measures. Authors were contacted when essential data were not available. All information was rechecked by the third author. Any discrepancies were resolved by consensus.
Assessing the risk of bias
The risk of bias of studies was assessed by two independent reviewers in accordance with the Cochrane Collaboration’s tool for risk of bias assessment. The evaluation index included the method used to generate the allocation sequence, the method used to conceal the allocation sequence, blinding, the completeness of outcome data, selective outcome reporting, and other bias.According to the information extracted from primary studies, each domain was rated as ‘high risk’, ‘unclear risk’ or ‘low risk’. Any disagreements were resolved based on consensus.
Publication bias
The funnel plot was created using Revman 5.3 software according to odds ratio of effective rate as the abscissa and standard error as the ordinate. The publication bias was assessed by examining the symmetry of the distribution of data. Such an analysis is ineligible when the number of included studies is less than 10.
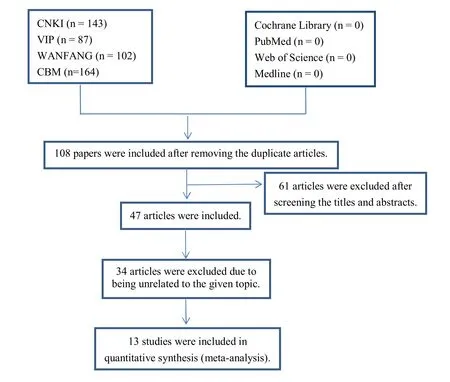
Figure 1 Flow chart
Statistical analysis
The heterogeneity of the studies included in this meta-analysis was assessed using the Q statistic test and the I2statistic test, where I2more than 50% indicated the evidence of heterogeneity. If P < 0.1, I2> 50%, A random-effects model was selected. Otherwise, a fixed-effects model was selected.
Results
Study identification and selection
We identified 496 papers in the initial database search and other sources stage. Of them, 388 articles were duplicated,and 61 were excluded after screening the titles and abstracts according to the selection criteria. After a detailed assessment of the remaining 47, 34 were excluded due to being unrelated to the given topic, a letter to the editor, or no available full text in English.Consequently, 13 eligible studies [9-21] were included in the meta-analysis, including 627 patients in the treatment group and 584 patients in the control group. A flow chart of the study retrieval and selection process is presented in Figure 1.
Study characteristics
All eligible studies were conducted in China and 1211 participants were included in total. Three studies [10, 18,21] used 0.5 mg neostigmine for the acupoint injection and 1 mg for intramuscular injection, including 112 patients in the treatment group and 111 patients in the control group. Three studies [14, 17, 19] used 0.5 mg neostigmine for acupoint injection and intramuscular injection respectively, including 112 patients in the treatment group and 105 patients in the control group.The other studies used 1 mg neostigmine for each of the acupoint injection and intramuscular injection, including 337 patients in the treatment group and 232 patients in the control group. The characteristics of each study included in the meta-analysis are presented in Table 1.
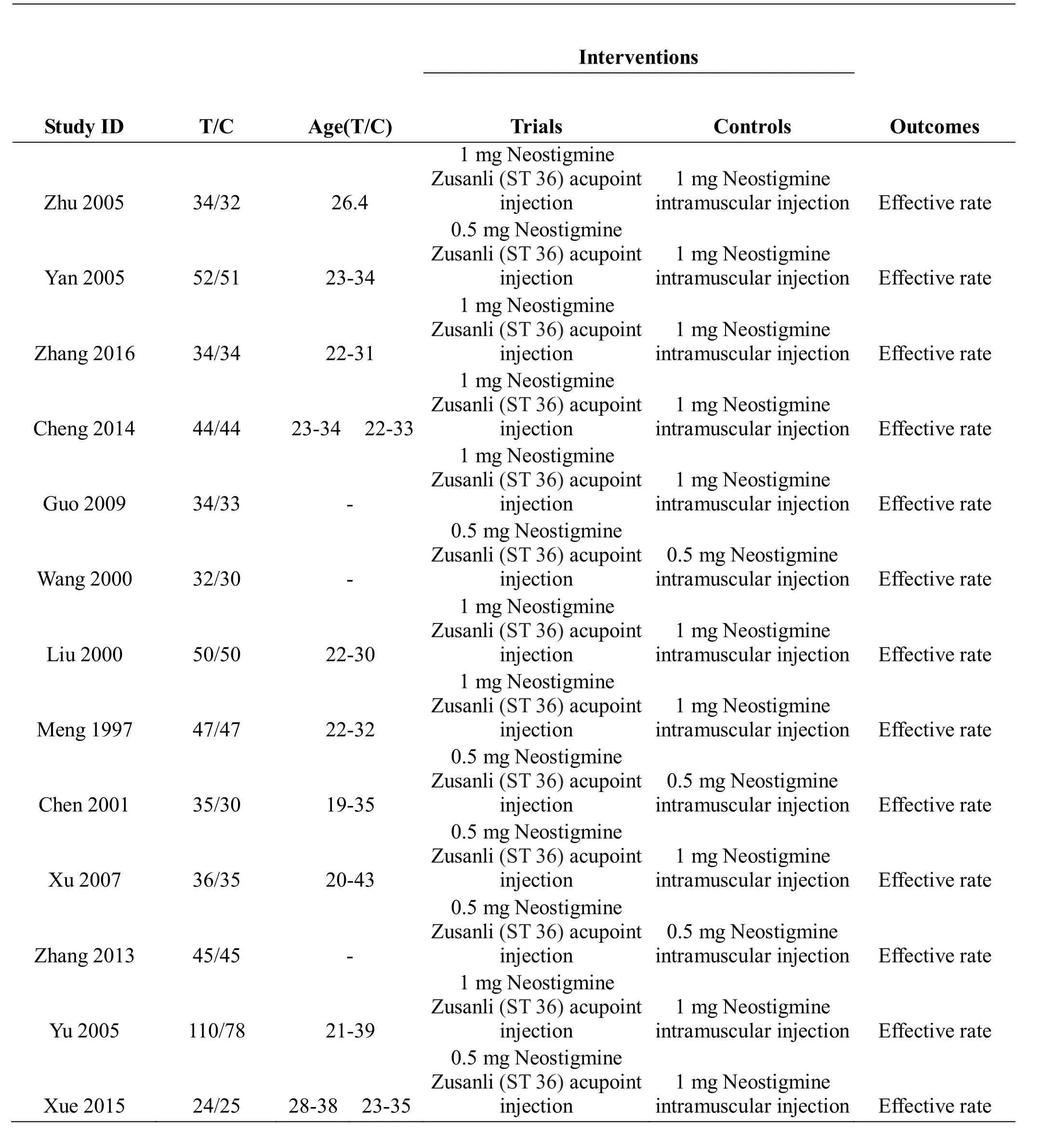
Table 1 The characteristics of each study included in the meta-analysis
Assessing risk of bias
A total of 13 eligible studies were incorporated into the meta-analysis. No studies reported the method used to conceal the allocation sequence or blinding. Eight studies stated a random method had been used but did not report how the allocation sequence was generated. Five studies did not report the method used to generate the allocation sequence and were rated as high risk. No incomplete data or selective outcome reporting bias was reported. The outcome of the risk of bias assessment is shown in Figure 2 and Figure 3.
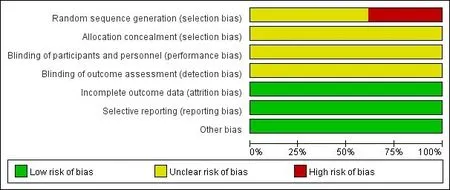
Figure 2 Risk assessment chart
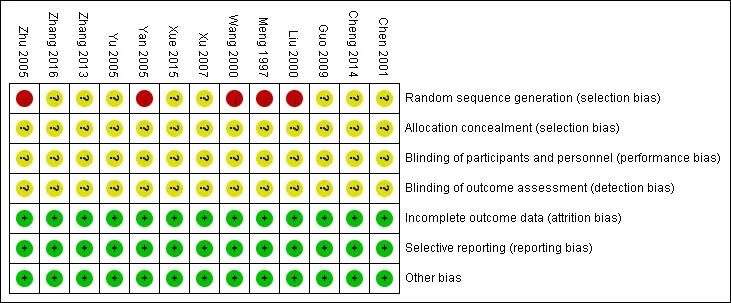
Figure 3 Risk assessment summary chart
Meta-analysis on the overall effective rate
Thirteen studies (12-14, 24-33) that investigated the overall effective rate acupoint injection of neostigmine relative to intramuscular injection were included in this meta-analysis. A fixed-effect model was used because of the lack of heterogeneity in the studies included in this meta-analysis (P = 0.92, I2= 0%). The meta-analysis found a significant difference between acupoint and intramuscular injection of neostigmine [OR = 8.74, 95%CI = (5.83, 13.10), Z = 10.49 P < 0.001]. Subgroup analysis was performed based on the dosage of drugs.Three studies used 0.5 mg neostigmine for acupoint injection and 1 mg for intramuscular injection, including 112 patients in the treatment group and 111 patients in the control group. A fixed-effect model was used because of the lack of heterogeneity in the studies included in this meta-analysis (P = 0.58, I2= 0%). The meta-analysis found a significant difference between acupoint and intramuscular injection of neostigmine [OR = 15.84, 95%CI = (5.74, 43.72), Z = 5.34, P < 0.001]. Three studies[14, 17, 19] used 0.5 mg neostigmine for both acupoint injection and intramuscular injection, including 217 patients. The I2was 42% (P = 0.18) and a fixed-effect model was used. The meta-analysis showed that a significant difference was detected between acupoint and intramuscular injection of neostigmine [OR = 7.30, 95%CI = (3.47, 15.34), Z = 5.249, P < 0.001]. Seven studies used 1 mg neostigmine for both acupoint injection and intramuscular injection, including 337 patients in the treatment group and 232 patients in the control group. A fixed-effect model was used given that I2was 42% (P =0.99). The meta-analysis found a significant difference between acupoint and intramuscular injection of neostigmine [OR = 7.76, 95% CI = (4.46, 13.52), Z =7.25, P < 0.001] (Figure 4).
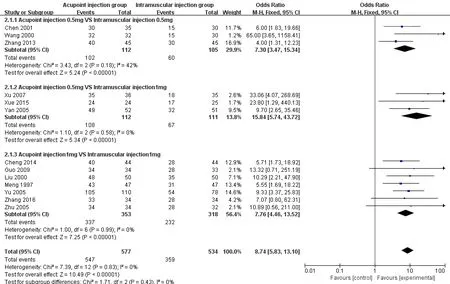
Figure 4 The results of meta - analysis of neostigmine Zusanli (ST 36) acupoint injection for postpartum urinary retention
Funnel plot
The funnel plot was not symmetrical, suggesting that there was publication bias (Figure 5). This may be because no studies with negative results were published or because all included studies were conducted in China.
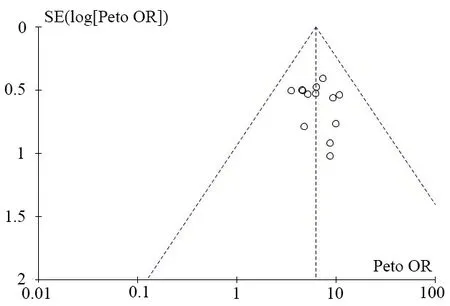
Figure 5 Inverted funnel
Discussion
Postpartum urinary retention is a gynecological emergency. Active treatment of postpartum urinary retention can effectively relieve maternal pain, prevent bladder distention causing postpartum hemorrhage due to uterine contraction, and reduce the need for indwelling catheters, thereby reducing the incidence of urinary tract infections [22].
The acupoint injection of neostigmine plays a dual role of acupuncture and medicine. It has rapid efficacy, no apparent side effects, and its use is simple. The results of the 13 [9-21] studies showed that the effect of neostigmine injection at the Zusanli (ST 36) acupoint on postpartum urinary retention was significant [OR = 8.74,95% CI (5.83, 13.10), Z = 10.49, P < 0.001], and the difference was statistically significant. In addition, this meta-analysis examined neostigmine at different dosages,dividing studies into three groups for subgroup analysis.The result showed that the curative effect in the acupoint injection group was significantly greater than that in the intramuscular injection group.
Neostigmine belongs to the class of anticholinergic drugs. It can stimulate bladder smooth muscle by inhibiting the activity of cholinesterase and increase the contractility of the bladder detrusor to promote micturition [24]. The acupoint injection of neostigmine has the dual effects of acupoints and drugs, and leads to the dredging of channels and collaterals (also known as the third route of administration). Intramuscular injection is merely a route of administration and is limited to the single therapeutic effect of drugs [25]. The Zusanli (ST 36) acupoint is the uniting point of the stomach meridian.It has the function of regulating Qi, blood, dredging the meridian, regulating the spleen and stomach,strengthening Qi, and cultivating vitality [26]. Chinese medicine believes that the postpartum retention of urine belongs to “postpartum dysuria,” that postpartum retention of urine is caused by the deficiency of kidney Qi,Qi deficiency of the spleen and lung, or the unsmooth circulation of Qi and blood [27]. Stimulating Zusanli (ST 36) acupoint can dredge Qi activity in the Middle Jiao and Lower Jiao, dredge channels and collaterals, and lead to recovery of bladder function [26]. Neostigmine injection at the Zusanli (ST 36) acupoint has the double effects of both the drug and acupuncture. The drug can go directly to the disease site along the meridian and stimulation of the acupoint can be sustained. The synergistic action of the drug and acupuncture accelerates the onset time of the drugs and enhances the therapeutic effect. However, there is little clinical research on treating postpartum urinary retention with neostigmine injections at the Zusanli (ST 36) acupoint. In terms of curative effect, it is of great significance for the treatment of postpartum urinary retention with neostigmine injections at the Zusanli (ST 36) acupoint. This meta-analysis confirmed the curative effect of Zusanli (ST 36) acupoint injection of neostigmine in treatment of postpartum urinary retention. This has clinical significance and will provide the basis for treatment of postpartum urinary retention with Zusanli (ST 36) acupoint injection of neostigmine in the treatment of postpartum urinary retention. Furthermore, it lays down foundations for future research.
The limitations of this study are as follows. (1) Only eight studies included in the analysis were randomized,but did not describe the method of randomization. The other five studies did not mention randomization methods,and the included studies were all had small sample sizes.The sample size was not estimated and the test efficiency was low. (2) All studies used a single assessment index that did not measure the residual urine in the bladder. (3)Only one study described adverse reactions. During this study, no patients had abdominal pain or an increase in systemic muscle tension. That no adverse reactions were mentioned in the other studies may affect the indicators of the final outcome. Suggestions for further study include the following. (1) In order to improve the quality of RCTs,multi-center RCTs using large samples should be performed. The necessary sample size should be estimated strictly. And random allocation,allocationconcealment, and blinding method should be correctly used. For the specificity of acupoint injections,it is difficult to effectively blind the subjects and implementers, but the researchers measuring the outcome should be blinded. (2) To ensure the accuracy and objectivity of clinical research, the dosage of the acupoint injection needs to be regulated, diagnostic and efficacy criteria need to be uniform, the intervention measures need to be detailed (especially the measurement of residual urine), and the study of adverse reactions should be strengthened.
To summarize, the curative effect of the treatment of postpartum urinary retention with neostigmine injection at the Zusanli (ST 36) acupoint is certain, but the quality of the studies included in the meta-analysis is low.Furthermore, the treatment’s efficacy needs further study and observation, and more high-quality research is still needed.
1. Chen HZ. Research progress on nursing and occurrence reason of postpartum urinary retention. Chin Nurs Res 2016, 30: 1924-1926.
2. Shi HM. Evaluation of pelvic floor muscle function training in prevention of postoperative urinary retention in cervical cancer. Chin J Prac Nurs 2011,27: 32-33.
3. Jin CH. Reason analysis and nursing of postpartum urinary retention. J Nurs Training 2005, 20: 148-148.
4. Chen LY, Chen L, Wu YM, et al. Comparison of outcomes of three different methods for treatment of postpartum urine retention. Nurs J Chin PLA 2003,20: 17-18.
5. Zhu YH, Chen YH. On effects of acupoints and drugs in acupoint-injection treatment. Chin Acupunct Moxibustion 2005, 25: 46-48.
6. Qi JC. Treatment experience of a case: postpartum urinary retention for 20 days. J Henan Coll Tradit Chin Med 1979, 4: 56-56.
7. Ma BZ. Chinese medicine gynecology. Shanghai:Shanghai Science and Technology Press 1997: 195.
8. Jia SB, Zhao MY, Liang LH, et al. Research of funnel plot in the proper use of meta-analysis. J Math Med 2013, 26(4): 402-405.
9. Zhu HM, Li M. Clinical observation of different methods of injecting neostigmine in the treatment of postpartum urinary retention. J Huaihai Med 2005, 23:148-148.
10. Yan H, Li CL. Efficacy of three therapies for postpartum urinary retention. J Community Med 2005, 3: 85-86.
11. Zhang XH. Postpartum urinary retention in patients with neostigmine acupuncture points after the closure of the efficacy of observation. Gansu Pharm 2016, 35:454-455.
12. Cheng GQ. Comparison of intramuscular injection and two-side Zusanli injection of neostigmine in the treatment of postpartum urinary retention. J Front Med 2014, 4: 81-82.
13. Guo CY, Mao XH. Clinical observation of 67 cases of postpartum urinary retention treated by different methods of neostigmine. Nei Mongol J Tradit Chin Med 2009, 28: 126.
14. Wang GM. Treatment of postpartum urinary retention by neostigmine acupoint injection. Cent Chin Med J 2000, 24: 151.
15. Liu SM, Jiang L. 50 cases postpartum urinary retention treated by neostigmine acupoint injection. J Pract Tradit Chin Med 2000, 16: 22-23.
16. Meng J. Curative effect of Zusanli point block and intramuscular injection of neostigmine on puerperal urine retention. Shanxi Nurs J 1997, 11: 36-36.
17. Chen D. Neostigmine acupoint injection in the treatment of 35 cases of postpartum urinary retention.Chinese Association of Integrative Medicine.Proceedings of the Fifth National Combination of Chinese and Western Medicine Experimental Medicine Symposium. 2001: 2
18. Xu CF. Treatment of 35 cases of postpartum urinary retention by neostigmine acupoint injection. Mod J Integr Tradit Western Med 2007, 16: 2253-2254.
19. Zhang Y. Effect of Zusanli acupoint injection of neostigmine in the treatment of postpartum urinary retention. Clin J Tradit Chin Med 2013, 25: 503-503.
20. Yu QX. Clinical observation of neostigmine Zusanli injection in the treatment of 110 cases postpartum urinary retention. Jiangsu J Tradit Chin Med 2005, 26:40-40.
21. Xue XH. Effect observation of Zusanli injection for postpartum urinary retention. Chin Pract Med 2015,10: 202-203.
22. Liao ZL, Luo YS, Ma YH, et al. Observation and nursing of the effect of two therapies on postpartum urinary retention. Mod Clin Nurs 2007, 6(4): 36-38.
23. Wang DS, Zhang ZL. “Acupoint injection” and“water needle therapy”. Shanghai J Acupunct Moxibustion 1997, 12: 48-48.
24. Yang GQ, Li TJ. The clinical observation on acupuncture point injection neostigmine for treating postpartum urinary retention. J Clin Acupunct Moxibustion 2016, 32: 35-37.
25. Lin JY, Xu YL, Ni F. Research progress of acupoint injection mechanism. J Liaoning Univ Tradit Chin Med 2007, 9: 189-191.
26. Zhao JN. Effect analysis of Zusanli acupoint injection of neostigmine in the treatment of postpartum urinary retention. Nei Mongol J Tradit Chin Med 2017, 36: 106-106.
27. Wu LF. Effect observation of Zusanli injection of neostigmine in the treatment of postpartum urinary retention. Contemp Med 2014, 20: 150-151.
 Traditional Medicine Research2018年2期
Traditional Medicine Research2018年2期
- Traditional Medicine Research的其它文章
- History of recurrent miscarriage in traditional Chinese medicine literature
- Clinical evidence and potential mechanisms of Chinese medicines for the treatment of diabetic retinopathy
- A systematic summary of natural compounds in Radix Glycyrrhizae
- Pharmacological intervention of traditional Chinese medicine for the quality of life in patients with colorectal cancer: a systematic review and meta-analysis
